THC 2021 Exchange Formulary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
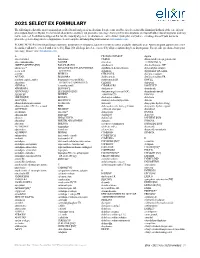
2021 SELECT EX FORMULARY the Following Is a List of the Most Commonly Prescribed Brand and Generic Medications
2021 SELECT EX FORMULARY The following is a list of the most commonly prescribed brand and generic medications. It represents an abbreviated version of the formulary list that is at the core of your prescription drug benefit plan. The list is not all-inclusive and does not guarantee coverage. Some preferred medications overlap with other clinical programs and may not be covered. In addition to drugs on this list, the majority of generic medications are covered under your plan and you are encouraged to ask your doctor to prescribe generic drugs whenever appropriate. Search complete formulary drug information at elixirsolutions.com. PLEASE NOTE: Preferred brand drugs may move to non-preferred status if a generic version becomes available during the year. Any medication approved to enter the market will not be covered until reviewed by Elixir. Not all drugs listed are covered by all prescription drug benefit programs. For specific questions about your coverage, please visit elixirsolutions.com. A B CILOXAN OINTMENT digoxin abacavir tablet balsalazide CIMDUO diltiazem ER (except generics for abacavir-lamivudine BAQSIMI cinacalcet CARDIZEM LA) ABILIFY MAINTENA [INJ] BASAGLAR [INJ] ciprofloxacin dimethyl fumarate DR* abiraterone* BD ULTRAFINE INSULIN SYRINGES ciprofloxacin-dexamethasone diphenoxylate-atropine acetic acid & NEEDLES citalopram dipyridamole ER-aspirin acitretin BELBUCA CITRANATAL divalproex sodium ACUVAIL BELSOMRA clarithromycin divalproex sodium ER acyclovir capsule, tablet benzonatate (except NDCs: clarithromycin ER DIVIGEL -
A Concise Guide to Treating Painful Oral Lesions
Drugs Used to Treat Osteoporosis and Bone Cancer Perio & Implant Centers The Team for of the Monterey Bay (831) 648-8800 Jochen P. Pechak, DDS, MSD in Silicon Valley (408) 738-3423 Which May Cause Osteonecrosis of the Jaws mobile: www.DrPechakapp.com he many bisphosphonates and monoclonal antibodies which are used to treat osteoporosis and bone cancer often web: GumsRus.com causeDrugsDrugs osteonecrosis Used Used of the to jaws.to Treat AsTreat dental clinicians,Osteoporosis Osteoporosis it is important that and andwe are Bone awareBone of this Cancers Cancers side effect before Ttreating our patients who are taking these drugs. The tables below summarize these drugs, the route these drugs are administered, andWhich Whichtheir likelihood May May of causing Cause Cause osteonecrosis Osteonecrosis Osteonecrosis of the jaws as reported byof of Dr. the theRobert Jaws JawsMarx at the University of Miami Division of Oral and Maxillofacial Surgery. PDL tm Osteoporosis Drugs Drugs Osteoporosis Used to Treat Drugs Osteoporosis PerioDontaLetter Jochen P. Pechak, DDS, MSD, Periodontics and Implant Dentistry Spring DrugDrug ClassificationClassification ActionAction DoseDose RouteRoute %% of of ReportedReported CasesCases of of OsteonecrosisOsteonecrosis AlendronateAlendronate BisphosphonateBisphosphonate OsteoclastOsteoclast 7070 mg/wk mg/wk OralOral 8282%% From Our Office A Concise Guide to Treating (Fosamax(Fosamax ToxicityToxicity to Yours... Generic)Generic) Painful Oral Lesions ResidronateResidronate BisphosphonateBisphosphonate OsteoclastOsteoclast 3535 mg/wk mg/wk OralOral 1%1% As dentists specializing in treat- (Actonel Toxicity (Actonel Toxicity ment of diseases of the oral cavity atients present frequently with Treating Cold Sores Atelvia)Atelvia) and associated structures, we are painful oral lesions. They are often also called upon to treat pain- IbandronateIbandronate BisphosphonateBisphosphonate OsteoclastOsteoclast 150150 mg/mos mg/mos OralOral 1%1% usually not serious, but patients And Canker Sores (Boniva) Toxicity IV ful oral lesions in the mouth. -

Making an Elderberry Syrup Or Elixir
Making an Elderberry Syrup or Elixir Herbal syrups are water extractions of herbs (usually decoctions—see below) that are concentrated with a sweetener (preferably organic white sugar or raw honey). This sweetener provides a bit of nutritional support as a carbohydrate and also acts as a preservative. The concentration of sugar is particularly important when making syrups and elixirs; when in water, sugar acts as a food source for micro-organisms (especially molds and yeasts). However, at a high enough concentration, the sugar actually restricts the growth ability of micro-organisms. So we are aiming to get our syrup to be saturated enough to preserve, but not so saturated that the sugar overwhelms the liquid and causes crystallization. When preparing a syrup, one of the following ratios should be used: 1 part decoction : 1 part sweetener 1 part decoction : 2 parts sweetener I tend to follow the 1 part water : 1 part sweetener suggestion, as the 1 : 2 ratio is too sweet for me. But I have access to a refrigerator, which will also help with preservation. If you are keeping your syrup at room temperature, the 1:2 ratio is best. Syrups are a great, palatable method for delivery of herbal medicines (especially for children), and are also a great way to mask the flavor of less tasty tinctures--just combine the tincture and the syrup and you get the medicinal benefits of both. Preserving syrups with honey is also a great way to combine the medicinal benefits of the honey with the herbs that are being used. Do not give syrups preserved with honey to children under the age of one. -

Slang Terms and Jargon Can Cause Medication Errors
Volume 19, Number 10 November/December 2005 Drugs & Therapy B � U � L � L � E � T � I � N MEDICATION SAFETY FORMULARY UPDATE The Pharmacy and Therapeutics Slang terms and jargon can Committee met October 18, 2005. 4 products were added in the Formulary cause medication errors and 2 were deleted. 1 dosage form was evaluated and designated nonformu- his month “Magic Mouthwash” ents. An allergy screen would not be lary and not available, and 2 drugs T was deleted from the Formulary done, unless the individual ingredients were evaluated, but not added. Criteria (see Formulary Update). The P&T are appreciated. for use were modifi ed for 3 drugs. Committee took this action for medica- Magic Mouthwash will no longer be tion safety reasons. This continues the dispensed at Shands UF because there ◆ ADDED policy of not allowing the use of non- is no evidence that it works better than specifi c terms for mixtures that have a plain saline rinse. Clozapine Tablets traditionally been used. This action follows the banning of (generic by IVAX) Terms like “Magic Mouthwash” are the term “Butt Paste” several years Glutaraldehyde 0.6% Solution slang, jargon, or coined phrases for ago. Like Magic Mouthwash, Butt Paste (compounded) mixtures that have a specifi c purpose. is a nonspecifi c mixture of ingredients. Levofl oxacin In this instance, the “magic” is pain The “Butt Paste” mixture contained (Levaquin® by Ortho McNeil)* reduction in patients who have muco- Questran Light® (cholestyramine) in sitis of the mouth. Mucositis is a very Aquaphor®. The theory is that the cho- Ondansetron Tablets ® painful condition in patients receiving lestyramine binds bile acids that may (Zofran by GlaxoSmithKline) aggressive cytotoxic chemotherapy. -

Pharmacy Manual Supplemental Policies, Procedures and Regulations
Last revision date: 12.17.2020 Pharmacy Manual Supplemental Policies, Procedures and Regulations Prepared by: Elixir 800-361-4542 ELIXIRSOLUTIONS.COM 2181 E. Aurora Road, Suite 201 | Twinsburg, OH 44087 Copyright © 2020, Elixir. All rights reserved. Version 41 *This page was intentionally left blank* 1 Table of Contents PHARMACY MANUAL INTRODUCTION......................................................................................................................... 5 GENERAL INFORMATION ............................................................................................................................................. 5 PROPRIETARY AND CONFIDENTIAL .................................................................................................................. 5 ADVERTISING REQUESTS .............................................................................................................................. 6 CONTACT INFORMATION / WHERE TO GET HELP ...................................................................................................... 6 NETWORK ENROLLMENT FORM AND CREDENTIALING GUIDELINES ....................................................................... 6 APPLYING FOR PARTICIPATION ...................................................................................................................... 6 CREDENTIALING AND RECREDENTIALING GUIDELINES ....................................................................................... 7 PROVIDER AND MEMBER SERVICE STANDARDS ..................................................................................................... -
Epinephrine Auto-Injector
ELIXIR; Epinephrine Auto-Injector FINAL DESIGN & PRODUCT SPECIFICATION REPORT DNH603_SEM2 Zoe Avgoustakis n8607912 CONTENTS 1. Introduction 2. Final Product Design 2.1 Description 2.2 Usability 2.3 QoI Table / Product Ecosystem 3. Value Proposition , 4. Design Justification 4.1 Mechanism 4.2 Form 4.3 Usability 5. Technical Documentation 5.1 Product Components 5.2 Product Function 5.3 Specifications 5.4 Standards 5.5 B.O.M Technical Drawings DNH603_16se2 : i-move project Epinephrine Auto-injector Zoe Avgoustakis n8607923 0.03mg Adrenaline 1. INTRODUCTION Over the course of this project, imm-you-nity has worked to provide innovative design solutions focused on interactive interfaces and devices to help people be more aware, in control and engaged with their health and wellness. The project aim was to design and develop a new consumer interactive product that would provide a distinct personal experience, improving the user’s management and relationship with their Health & Wellness. The project was specifically focused towards the user’s engagement with allergy conditions. Design investigation accounted for emerging technologies and how this could be applied to enhance the user’s management and interaction with severe allergies and anaphylaxis. Australia has one of the highest reported incidences of food allergies in the world with one in ten people forecasted to develop a food allergy throughout their lives. As those who obtain allergies become more and more prevalent, people are turning to technology for assitance of this issue. The client approached the team in endeavour to develop a product that could assist people with the management and treatment of severe allergy conditions of anaphylaxis. -

2020 PBD 5 Tier Formulary
2020 Pharmacy Benefit Dimensions 5 Tier Drug Formulary The following information applies to most members enrolled in a Pharmacy Benefit Dimensions pharmacy plan. Note: If you are reading a printed version of this drug formulary, content may have been updated since it was last printed. For the most up-to-date information, please visit www.pbdrx.com. Drug Formulary Introduction • Generic drugs appear in lower case. Brand name drugs are capitalized. • Preferred generic drugs and a few select brand name drugs are assigned to Tier 1. In most instances, once a generic product is available for which there are no bioequivalence concerns, the brand product is removed from the formulary (not covered), and the generic product is assigned to Tier 1. Certain generic drugs may also be covered in a non-preferred tier when efficacy, safety, or cost factors suggest that better alternatives exist on the formulary. • Pharmacy Benefit Dimensions reserves the right to modify drug tiers as necessary. • Some medications are considered non-formulary (not covered). To obtain a medication that is non-formulary, your health care provider is encouraged to submit a Prior Authorization request for coverage through the exception process. If the request is approved, you will be responsible for the cost share associated with a non- preferred drug tier. • Certain self-funded employer groups may not follow this base formulary and certain exclusions may apply. Members in these pharmacy benefit management groups should refer to their summary plan description and/or their benefit administrator. Prior-Authorization Prior Authorization is required for certain medications. To obtain coverage for a medication requiring Prior Authorization, a Prior Authorization request for medical exception must be submitted by your health care provider and approved by Pharmacy Benefit Dimensions. -
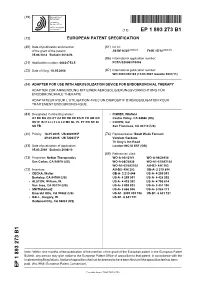
Adapter for Use with Aerosolization Device For
(19) TZZ_¥ ¥_T (11) EP 1 893 273 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61M 16/20 (2006.01) F16K 15/14 (2006.01) 25.06.2014 Bulletin 2014/26 (86) International application number: (21) Application number: 06824753.5 PCT/US2006/019446 (22) Date of filing: 18.05.2006 (87) International publication number: WO 2007/030162 (15.03.2007 Gazette 2007/11) (54) ADAPTER FOR USE WITH AEROSOLIZATION DEVICE FOR ENDOBRONCHIAL THERAPY ADAPTER ZUR ANWENDUNG MIT EINER AEROSOLISIERUNGSVORRICHTUNG FÜR ENDOBRONCHIALE THERAPIE ADAPTATEUR POUR L’UTILISATION AVEC UN DISPOSITIF D’AÉROSOLISATION POUR TRAITEMENT ENDOBRONCHIQUE (84) Designated Contracting States: • FISHER, Winfield AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Castro Valley, CA 94546 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • COHEN, Gal SK TR San Francisco, CA 94110 (US) (30) Priority: 18.05.2005 US 682099 P (74) Representative: Boult Wade Tennant 29.09.2005 US 722637 P Verulam Gardens 70 Gray’s Inn Road (43) Date of publication of application: London WC1X 8BT (GB) 05.03.2008 Bulletin 2008/10 (56) References cited: (73) Proprietor: Nektar Therapeutics WO-A-00/12161 WO-A-98/20938 San Carlos, CA 94070 (US) WO-A-98/20938 WO-A1-02/092169 WO-A1-02/092169 AU-B2- 496 203 (72) Inventors: AU-B2- 496 203 GB-A- 2 219 844 • CECKA, Walter GB-A- 2 219 844 US-A- 4 259 951 Berkeley, CA 94705 (US) US-A- 4 259 951 US-A- 4 428 392 • ALSTON, William, W. -

New York (HARP) Medicaid
New York Health and Recovery Plan (HARP) Lista de medicamentos preferidos aprobada por Medicaid En vigencia desde el 1 de febrero de 2020 Leyenda En cada categoría, los medicamentos se listan en orden alfabético por marca o nombre genérico. Medicamento de marca: letra mayúscula en negrita Medicamento genérico: letra minúscula en texto sin formato AL: restricción de límite de edad DO: programa de optimización de dosis GR: restricción de género OTC: medicamento de venta libre disponible con receta. (Los recetadores deben incluir la sigla OTC en la receta). PA: requiere autorización previa. La autorización previa es el proceso mediante el cual se obtiene la aprobación de los beneficios antes de que se puedan abastecer ciertas recetas. QL: límites de cantidad. Ciertos medicamentos recetados tienen límites de cantidad específicos, por receta o por mes. SP: farmacia de medicamentos especiales ST: requiere terapia escalonada. Es posible que necesite utilizar un medicamento antes de que los beneficios para el uso de otro medicamento puedan autorizarse. Nombre del medicamento Referencia Notas ADYUVANTES FARMACÉUTICOS cvs petroleum jelly external gel CareAll Petroleum Jelly OTC RA Tugaboos Petroleum gnp petroleum jelly gel OTC Jelly RA Tugaboos Petroleum hm petroleum jelly gel OTC Jelly ORA-PLUS ORAL LIQUID OTC petroleum jelly external gel CareAll Petroleum Jelly OTC petroleum jelly external ointment OTC RA Tugaboos Petroleum petroleum jelly gel OTC Jelly RA Tugaboos Petroleum ra petroleum jelly gel OTC Jelly RA TUGABOOS PETROLEUM JELLY GEL OTC -
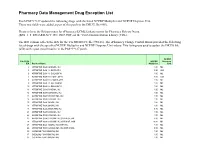
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

Sulfanilamide Disaster
Sulfanilamide Disaster FDA Consumer magazine June 1981 Issue By Carol Ballentine Taste of Raspberries, Taste of Death: The 1937 Elixir Sulfanilamide Incident By the 1930s it was widely recognized that the Food and Drugs Act of 1906 was obsolete, but bitter disagreement arose as to what should replace it. By 1937 most of the arguments had been resolved but Congressional action was stalled. Then came a shocking development--the deaths of more than 100 people after using a drug that was clearly unsafe. The incident hastened final enactment in 1938 of the Federal Food, Drug, and Cosmetic Act, the statute that today remains the basis for FDA regulation of these products. Nobody but Almighty God and I can know what I have been through these past few days. I have been familiar with death in the years since I received my M.D. from Tulane University School of Medicine with the rest of my class of 1911. Covington County has been my home. I have practiced here for years. Any doctor who has practiced more than a quarter of a century has seen his share of death. "But to realize that six human beings, all of them my patients, one of them my best friend, are dead because they took medicine that I prescribed for them innocently, and to realize that that medicine which I had used for years in such cases suddenly had become a deadly poison in its newest and most modern form, as recommended by a great and reputable pharmaceutical firm in Tennessee: well, that realization has given me such days and nights of mental and spiritual agony as I did not believe a human being could undergo and survive. -

Conformal Coating of Powder by Initiated Chemical Vapor Deposition on Vibrating Substrate
pharmaceutics Article Conformal Coating of Powder by Initiated Chemical Vapor Deposition on Vibrating Substrate Katrin Unger and Anna Maria Coclite * Institute of Solid State Physics, Graz University of Technology, 8010 Graz, Austria; [email protected] * Correspondence: [email protected]; Tel.: +43-316-873-8970 Received: 16 July 2020; Accepted: 18 September 2020; Published: 22 September 2020 Abstract: Encapsulation of pharmaceutical powders within thin functional polymer films is a powerful and versatile method to modify drug release properties. Conformal coating over the complete surface of the particle via chemical vapor deposition techniques is a challenging task due to the compromised gas–solid contact. In this study, an initiated chemical vapor deposition reactor was adapted with speakers and vibration of particles was achieved by playing AC/DC’s song “Thunderstruck” to overcome the above-mentioned problem. To show the possibilities of this method, two types of powder of very different particle sizes were chosen, magnesium citrate (3–10 µm, cohesive powder) and aspirin (100–500 µm, good flowability), and coated with poly-ethylene-glycol-di-methacrylate. The release curve of coated magnesium citrate powder was retarded compared to uncoated powder. However, neither changing the thickness coating nor vibrating the powder during the deposition had influence on the release parameters, indicating, that cohesive powders cannot be coated conformally. The release of coated aspirin was as well retarded as compared to uncoated aspirin, especially in the case of the powder that vibrated during deposition. We attribute the enhancement of the retarded release to the formation of a conformal coating on the aspirin powder.