Toxicity Review for Di(2-Ethylhexyl) Phthalate (DEHP)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Newsletter Term 1 19-20
Heritage Skills Event Fifteen of our students attended a workshop session in Perth City Centre aimed at promoting careers using traditional building skills. The event, organised by Perth and Kinross Heritage Trust, gave the pupils an experience of using traditional skills of carpentry, stone masonry, slating and painting. Our students thoroughly enjoyed the event, and some of them highly impressed the organisers! The event was even attended by Depute First Minister, John Swinney MSP, who took time out of his busy schedule to chat to our students and congratulate them for taking part. Primary Language Ambassadors Welcome to our new group of P5-7 Language Ambassadors for this year! They are enthusiastic about celebrating all the languages spoken in St John's Academy and are looking forward to supporting language learning throughout the school. This year's Language Ambassadors are already bursting with ideas, including competitions, lunch clubs and quizzes. Their first task has been to celebrate 'European Day of Languages' on Thursday, 26th September. European Day of Languages On Thursday, 26th September, we celebrated the European Day of Languages. Many classes took part in numerous activities for the promotion of languages. We had fun dressing up in costumes from around the world, completed quizzes about Europe, translated Follow us on Twitter music titles and increased our vocabulary for @sja_languages greeting people in a language other than their mother tongue as well as discussing the benefits of having knowledge of more than one language. Our pupils approached the many activities with great gusto! In addition, on a recent visit to the school, Bishop Stephen Robson was more than happy to help fly the language flag by joining the Senior Leadership Team for a photograph to celebrate this special day. -

(12) Patent Application Publication (10) Pub. No.: US 2004/0224012 A1 Suvanprakorn Et Al
US 2004O224012A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0224012 A1 Suvanprakorn et al. (43) Pub. Date: Nov. 11, 2004 (54) TOPICAL APPLICATION AND METHODS Related U.S. Application Data FOR ADMINISTRATION OF ACTIVE AGENTS USING LIPOSOME MACRO-BEADS (63) Continuation-in-part of application No. 10/264,205, filed on Oct. 3, 2002. (76) Inventors: Pichit Suvanprakorn, Bangkok (TH); (60) Provisional application No. 60/327,643, filed on Oct. Tanusin Ploysangam, Bangkok (TH); 5, 2001. Lerson Tanasugarn, Bangkok (TH); Suwalee Chandrkrachang, Bangkok Publication Classification (TH); Nardo Zaias, Miami Beach, FL (US) (51) Int. CI.7. A61K 9/127; A61K 9/14 (52) U.S. Cl. ............................................ 424/450; 424/489 Correspondence Address: (57) ABSTRACT Eric G. Masamori 6520 Ridgewood Drive A topical application and methods for administration of Castro Valley, CA 94.552 (US) active agents encapsulated within non-permeable macro beads to enable a wider range of delivery vehicles, to provide longer product shelf-life, to allow multiple active (21) Appl. No.: 10/864,149 agents within the composition, to allow the controlled use of the active agents, to provide protected and designable release features and to provide visual inspection for damage (22) Filed: Jun. 9, 2004 and inconsistency. US 2004/0224012 A1 Nov. 11, 2004 TOPCAL APPLICATION AND METHODS FOR 0006 Various limitations on the shelf-life and use of ADMINISTRATION OF ACTIVE AGENTS USING liposome compounds exist due to the relatively fragile LPOSOME MACRO-BEADS nature of liposomes. Major problems encountered during liposome drug Storage in vesicular Suspension are the chemi CROSS REFERENCE TO OTHER cal alterations of the lipoSome compounds, Such as phos APPLICATIONS pholipids, cholesterols, ceramides, leading to potentially toxic degradation of the products, leakage of the drug from 0001) This application claims the benefit of U.S. -

Coronary Effect of Fibrates on Proteins and Enzymes Which Hydrolyze Triacylglycerols
Acta Poloniae Pharmaceutica ñ Drug Research, Vol. 73 No. 3 pp. 579ñ588, 2016 ISSN 0001-6837 Polish Pharmaceutical Society CORONARY EFFECT OF FIBRATES ON PROTEINS AND ENZYMES WHICH HYDROLYZE TRIACYLGLYCEROLS RENATA FRANCIK 1,2*, JADWIGA KRYCZYK 3 and S£AWOMIR FRANCIK 4 1 Department of Bioorganic Chemistry, 2 Department of Food Chemistry and Nutrition, Jagiellonian University, Medical College, Faculty of Pharmacy, 9 Medyczna St., 30-688 KrakÛw, Poland 2 Institute of Health, State Higher Vocational School, 1 Staszica St., 33-300 Nowy Sπcz, Poland 3 Jagiellonian University Medical College, Department of Food Chemistry and Nutrition, 9 Medyczna St., 30-688 KrakÛw, Poland 4 Department of Mechanical Engineering and Agrophysics, University of Agriculture in Krakow, Faculty of Production Engineering and Energetics, 116 B Balicka St., 30-149, KrakÛw, Poland Abstract: Clofibric acid derivatives called fibrates, are quite commonly used lipid-lowering drugs, so it is nec- essary to know beneficial and adverse effects of these compounds on the body. The European Medicines Agencyís Committee for Medicinal Products for Human Use (CHMP) has concluded that benefits of four fibrates such as: bezafibrate, ciprofibrate, fenofibrate and gemfibrozil continue outweigh their risk in treatment of people with blood lipid disorders. According to recommendations of the CHMP fibrates should not be used as first-line drugs, except in patients with severe hypertriglyceridemia and patients who cannot use statins. In this paper, we focused on effect of clofibric acid derivatives -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
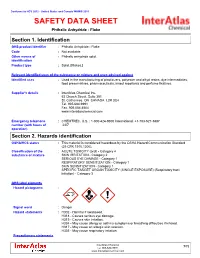
SAFETY DATA SHEET Phthalic Anhydride - Flake
Conforms to HCS 2012 - United States and Canada WHMIS 2015 SAFETY DATA SHEET Phthalic Anhydride - Flake Section 1. Identification GHS product identifier : Phthalic Anhydride - Flake Code : Not available. Other means of : Phthalic anhydride solid. identification Product type : Solid. [Flakes.] Relevant identified uses of the substance or mixture and uses advised against Identified uses : Used in the manufacturing of plasticizers, polyester and alkyd resins, dye intermediates, food preservatives, pharmaceuticals, insect repellants and perfume fixatives. Supplier's details : InterAtlas Chemical Inc. 63 Church Street, Suite 301 St. Catharines, ON CANADA L2R 3C4 Tel. 905.684.9991 Fax. 905.684.4504 www.interatlaschemical.com Emergency telephone : CHEMTREC, U.S. : 1-800-424-9300 International: +1-703-527-3887 number (with hours of 24/7 operation) Section 2. Hazards identification OSHA/HCS status : This material is considered hazardous by the OSHA Hazard Communication Standard (29 CFR 1910.1200). Classification of the : ACUTE TOXICITY (oral) - Category 4 substance or mixture SKIN IRRITATION - Category 2 SERIOUS EYE DAMAGE - Category 1 RESPIRATORY SENSITIZATION - Category 1 SKIN SENSITIZATION - Category 1 SPECIFIC TARGET ORGAN TOXICITY (SINGLE EXPOSURE) (Respiratory tract irritation) - Category 3 GHS label elements Hazard pictograms : Signal word : Danger Hazard statements : H302 - Harmful if swallowed. H318 - Causes serious eye damage. H315 - Causes skin irritation. H334 - May cause allergy or asthma symptoms or breathing difficulties if inhaled. H317 - May cause an allergic skin reaction. H335 - May cause respiratory irritation. Precautionary statements InterAtlas Chemical 1/12 Tel: 905-684-9991 www.interatlaschemical.com Phthalic Anhydride - Flake Section 2. Hazards identification Prevention : P280 - Wear protective gloves. Wear eye or face protection. -

The Condensation of Phenols with Maleic Anhydride
South Dakota State University Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange Theses and Dissertations 1951 The ondeC nsation of Phenols with Maleic Anhydride Leslie D. Kamstra Follow this and additional works at: https://openprairie.sdstate.edu/etd Recommended Citation Kamstra, Leslie D., "The ondeC nsation of Phenols with Maleic Anhydride" (1951). Theses and Dissertations. 2215. https://openprairie.sdstate.edu/etd/2215 This Thesis - Open Access is brought to you for free and open access by Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange. For more information, please contact [email protected]. THE CONDENSATION OF PHENOLS WITH MALEIC ANHYDRIDE By Leslie D. Kamstra This thesis is approved as a creditable independent investigation by a candidate for the degree, Master of Science, and acceptable as meeting the thesis requirements for this degree, but without imVlying that the conclusions reached by the candidate are neces sarily the conclusions of the major department. ,(\ � -� fSOUTH DAKOTA ·STATE COLLEGE LIBRARY page i TABLE OF CONTENTS Introduction• ••.......•..••••••••.•••••....•.•..•.••••• #,• 1 Condensation using Hydrated and Anhydrous Stannic Chloride 2 Preparation of the Original Product•• � •...•• � 2 Determination of Temperature and Time for Optimum -

Review of Exposure Data and Assessments for Select Dialkyl
TABLE OF CONTENTS 1. INTRODUCTION ........................................................................................................... 1-1 2. PRODUCTION AND USE OF PHTHALATES ............................................................. 2-1 2.1. PRODUCTION OF PHTHALATES ................................................................... 2-1 2.1.1. Production of DEHP ................................................................................ 2-1 2.1.2. Production of DBP ................................................................................... 2-2 2.1.3. Production of BBP ................................................................................... 2-2 2.1.4. Production of DINP ................................................................................. 2-3 2.1.5. Production of DIDP ................................................................................. 2-3 2.1.6. Production of DnOP ................................................................................. 2-4 2.2. USE OF PHTHALATES ..................................................................................... 2-4 3. PHYSICO-CHEMICAL AND ENVRONMENTAL FATE PROPERTIES OF PHTHALATES ................................................................................. 3-1 3.1. PHYSICO-CHEMICAL PROPERTIES OF PHTHALATES ............................. 3-1 3.1.1. Benzyl butyl phthalate (BBP) .................................................................. 3-1 3.1.2. Di-n-butyl phthalate (DBP) ..................................................................... -

Polyvinyl Chloride - Wikipedia Polyvinyl Chloride
1/24/2020 Polyvinyl chloride - Wikipedia Polyvinyl chloride Polyvinyl chloride (/ˌpɒlivaɪnəl ˈklɔːraɪd/;[5] colloquial: Polyvinyl chloride polyvinyl, vinyl;[6] abbreviated: PVC) is the world's third-most widely produced synthetic plastic polymer, after polyethylene and polypropylene.[7] About 40 million tonnes are produced per year. PVC comes in two basic forms: rigid (sometimes abbreviated as RPVC) and flexible. The rigid form of PVC is used in construction for pipe and in profile applications such as doors and windows. It is also used in making bottles, non-food packaging, food-covering sheets,[8] and cards (such as bank or membership cards). It can be made softer and more flexible by the addition of plasticizers, the most widely used being phthalates. In this form, it is also used in plumbing, electrical cable insulation, imitation leather, flooring, signage, phonograph records,[9] inflatable products, and many applications where it replaces rubber.[10] With cotton or linen, it is used to make canvas. Pure polyvinyl chloride is a white, brittle solid. It is insoluble in alcohol but slightly soluble in tetrahydrofuran. Contents Discovery Production Microstructure Names Producers IUPAC name Additives poly(1-chloroethylene)[1] Phthalate plasticizers Di-2ethylhexylphthalate Other names Metal stabilizers Polychloroethylene Heat stabilizers Identifiers Properties CAS Number 9002-86-2 (http://ww Mechanical w.commonchemistry. Thermal and fire org/ChemicalDetail.a Electrical spx?ref=9002-86-2) Chemical Abbreviations PVC Applications ChEBI CHEBI:53243 -

Ross Bennett @Golder.Com
REPORT ON-PROPERTY SITE INVESTIGATION WORK PLAN Saint-Gobain Performance Plastics Facility 701 Daniel Webster Highway in Merrimack, New Hampshire Submitted to: New Hampshire Department of Environmental Services Hazardous Waste Remediation Bureau 29 Hazen Drive, PO Box 95 Concord, New Hampshire 03302 Submitted by: Saint-Gobain Performance Plastics Corp. 14 McCaffrey Street Hoosick Falls, New York 12090 Submitted by: Golder Associates Inc. 670 North Commercial Street, Suite 103 Manchester, New Hampshire, USA 03101 June 8, 2018 June 8, 2018 1668623 Table of Contents 1.0 INTRODUCTION ............................................................................................................................................. 1 2.0 BACKGROUND .............................................................................................................................................. 1 2.1 Property and Facility History ................................................................................................................ 1 2.2 Summary of Previous Investigations .................................................................................................... 3 3.0 PRELIMINARY CONCEPTUAL SITE MODEL .............................................................................................. 3 3.1 Geologic and Hydrogeologic Setting .................................................................................................... 4 3.2 Potential Releases and Transport Mechanisms ................................................................................. -

Phthalic Anhydride Catalysts Brochure
Do you want to combine experience with innovation? BASF Phthalic Anhydride Catalysts are the market leading solution for your oxidation process. Introduction Phthalic Anhydride Catalysts 03 Table of Content BASF Catalysts Introduction BASF – We create Chemistry BASF Catalysts Introduction 03 As the world’s leading chemical company, BASF: Offers intelligent solutions and high-quality products BASF Research & Development 09 for most industrial challenges Uses new technologies to optimize additional market opportunities Phthalic Anhydride Catalysts Portfolio 12 Combines added value with environmental protection and social responsibility Phthalic Anhydride Catalysts for o-Xylene Oxidation 12 Phthalic Anhydride Catalysts for Naphthalene/Mixed 16 BASF at a Glance Support Technical Services 19 At BASF, we create chemistry for a sustainable future. We combine economic success with environmental protection and social responsibility. More than 117,000 employees in the BASF Group work on contributing to the success of our customers in nearly all sectors and almost every country in the world. Our portfolio is organized into six segments: Chemicals, Materials, Industrial Solutions, Surface Technologies, Nutrition & Care and Agricultural Solutions. BASF has companies in more than 90 countries. We operate six Verbund sites and 361 additional production sites world- wide. Our Verbund site in Ludwigshafen, Germany, is the world’s largest chemical complex owned by a single company that was developed as an integrated network. This was where the Verbund principle was originally established and continu- ously optimized before being implemented at additional sites. BASF's Catalysts division, headquartered in Iselin, New Jersey, is the world’s leading supplier of environmental and process catalysts. The group employs more than 5,000, with over 30 manufacturing sites worldwide. -

Phthalic Anhydride
Right to Know Hazardous Substance Fact Sheet Common Name: PHTHALIC ANHYDRIDE Synonyms: 1,2-Benzendicarboxylic Anhydride; 1,3-Dioxophthalon CAS Number: 85-44-9 Chemical Name: 1,3-Isobenzofurandione RTK Substance Number: 1535 Date: August 2001 Revision: April 2010 DOT Number: UN 2214 Description and Use EMERGENCY RESPONDERS >>>> SEE LAST PAGE Phthallic Anhydride is a colorless to white, crystalline (sand- Hazard Summary like) or needle-shaped solid, or a pale yellow liquid when in Hazard Rating NJDOH NFPA molten form, with a strong, choking odor. It is used to make HEALTH - 3 plastics, resins, dyes, pharmaceuticals and fungicides. FLAMMABILITY - 1 REACTIVITY - 0 f ODOR THRESHOLD = 0.053 ppm CORROSIVE f Odor thresholds vary greatly. Do not rely on odor alone to POISONOUS GASES ARE PRODUCED IN FIRE determine potentially hazardous exposures. Hazard Rating Key: 0=minimal; 1=slight; 2=moderate; 3=serious; Reasons for Citation 4=severe f Phthallic Anhydride is on the Right to Know Hazardous Substance List because it is cited by OSHA, ACGIH, DOT, f Phthallic Anhydride can affect you when inhaled. NIOSH, DEP, IRIS, NFPA and EPA. f Contact can severely irritate and burn the skin and eyes. f This chemical is on the Special Health Hazard Substance f Inhaling Phthallic Anhydride can irritate the nose, throat List. and lungs. f Phthallic Anhydride may cause a skin allergy and an asthma-like allergy. f Phthallic Anhydride may damage the liver and kidneys. f Phthallic Anhydride is a DOT CORROSIVE. SEE GLOSSARY ON PAGE 5. Workplace Exposure Limits OSHA: The legal airborne permissible exposure limit (PEL) is FIRST AID 3 12 mg/m averaged over an 8-hour workshift. -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement.