Whole-Exome Sequencing to Identify Potential Genetic Risk in Substance Use Disorders: a Pilot Feasibility Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Whole Exome and Whole Genome Sequencing – Oxford Clinical Policy
UnitedHealthcare® Oxford Clinical Policy Whole Exome and Whole Genome Sequencing Policy Number: LABORATORY 024.11 T2 Effective Date: October 1, 2021 Instructions for Use Table of Contents Page Related Policies Coverage Rationale ....................................................................... 1 Chromosome Microarray Testing (Non-Oncology Documentation Requirements ...................................................... 2 Conditions) Definitions ...................................................................................... 2 Molecular Oncology Testing for Cancer Diagnosis, Prior Authorization Requirements ................................................ 3 Prognosis, and Treatment Decisions Applicable Codes .......................................................................... 3 • Preimplantation Genetic Testing Description of Services ................................................................. 4 Clinical Evidence ........................................................................... 4 U.S. Food and Drug Administration ........................................... 22 References ................................................................................... 22 Policy History/Revision Information ........................................... 26 Instructions for Use ..................................................................... 27 Coverage Rationale Whole Exome Sequencing (WES) Whole Exome Sequencing (WES) is proven and Medically Necessary for the following: • Diagnosing or evaluating a genetic disorder -

Whole Exome Sequencing Faqs
WHOLE EXOME SEQUENCING (WES) Whole Exome Sequencing (WES) is generally ordered when a patient’s medical history and physical exam strongly suggest that there is an underlying genetic etiology. In some cases, the patient may have had an extensive evaluation consisting of multiple genetic tests, without identifying an etiology. In other cases, a physician may opt to order one of the Whole Exome Sequencing tests early in the patient’s evaluation in an effort to expedite a possible diagnosis and reduce costs incurred by multiple tests. Whole Exome Sequencing is a highly complex test that is newly developed for the identification of changes in a patient’s DNA that are causative or related to their medical concerns. In contrast to current sequencing tests that analyze one gene or small groups of related genes at a time, Whole Exome Sequencing analyzes the exons or coding regions of thousands of genes simultaneously using next-generation sequencing techniques. The exome refers to the portion of the human genome that contains functionally important sequences of DNA that direct the body to make proteins essential for the body to function properly. These regions of DNA are referred to as exons. There are approximately 180,000 exons in the human genome which represents about 3% of the genome. These 180,000 exons are arranged in about 22,000 genes. It is known that many of the errors that occur in DNA sequences that then lead to genetic disorders are located in the exons. Therefore, sequencing of the exome is thought to be an efficient method of analyzing a patient’s DNA to discover the genetic cause of diseases or disabilities. -

WO 2014/135655 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/135655 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C12Q 1/68 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/EP2014/054384 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 6 March 2014 (06.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13305253.0 6 March 2013 (06.03.2013) EP (84) Designated States (unless otherwise indicated, for every (71) Applicants: INSTITUT CURIE [FR/FR]; 26 rue d'Ulm, kind of regional protection available): ARIPO (BW, GH, F-75248 Paris cedex 05 (FR). CENTRE NATIONAL DE GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, LA RECHERCHE SCIENTIFIQUE [FR/FR]; 3 rue UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, Michel Ange, F-75016 Paris (FR). -

An Efficient and Scalable Analysis Framework for Variant Extraction and Refinement from Population-Scale DNA Sequence Data
Downloaded from genome.cshlp.org on October 4, 2021 - Published by Cold Spring Harbor Laboratory Press Method An efficient and scalable analysis framework for variant extraction and refinement from population-scale DNA sequence data Goo Jun,1,2 Mary Kate Wing,2 Gonçalo R. Abecasis,2 and Hyun Min Kang2 1Human Genetics Center, School of Public Health, The University of Texas Health Science Center at Houston, Houston, Texas 77030, USA; 2Center for Statistical Genetics and Department of Biostatistics, University of Michigan School of Public Health, Ann Arbor, Michigan 48109, USA The analysis of next-generation sequencing data is computationally and statistically challenging because of the massive vol- ume of data and imperfect data quality. We present GotCloud, a pipeline for efficiently detecting and genotyping high- quality variants from large-scale sequencing data. GotCloud automates sequence alignment, sample-level quality control, variant calling, filtering of likely artifacts using machine-learning techniques, and genotype refinement using haplotype in- formation. The pipeline can process thousands of samples in parallel and requires less computational resources than current alternatives. Experiments with whole-genome and exome-targeted sequence data generated by the 1000 Genomes Project show that the pipeline provides effective filtering against false positive variants and high power to detect true variants. Our pipeline has already contributed to variant detection and genotyping in several large-scale sequencing projects, including the 1000 Genomes Project and the NHLBI Exome Sequencing Project. We hope it will now prove useful to many medical sequencing studies. [Supplemental material is available for this article.] The cost of human genome sequencing has declined rapidly, pow- There is a pressing need for software pipelines that support ered by advances in massively parallel sequencing technologies. -

Bioinformatics Approaches to Identify Pain Mediators, Novel Lncrnas and Distinct Modalities of Neuropathic Pain
Bioinformatics approaches to identify pain mediators, novel LncRNAs and distinct modalities of neuropathic pain by Georgios Baskozos A thesis submitted to University College London for the degree of Doctor of Philosophy Institute of Structural and Molecular Biology University College London September 2016 1 Declaration I, Georgios Baskozos, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. ……………………………………… Georgios Baskozos 29 September 2016 2 Abstract This thesis presents a number of studies in the general subject of bioinformatics and functional genomics. The studies were made in collaboration with experimental scientists of the London Pain Consortium (LPC), an initiative that has promoted collaborations between experimental and computational scientists to further understanding of pain. The studies are mainly concerned with the molecular biology of pain and deal with data gathered from high throughput technologies aiming to assess the transcriptional changes involved in well induced pain states, both from animal models of pain and human patients. We have analysed next generation sequencing data (NGS data) in order to assess the transcriptional changes in rodent’s dorsal root ganglions under well induced pain states. We have also developed a customised computational pipeline to analyse RNA- sequencing data in order to identify novel Long non-coding RNAs (LncRNAs), which may function as mediators of neuropathic pain. Our analyses detected hundreds of novel LncRNAs significantly dysregulated between sham-operated animals and animal models of pain. In addition, in order to gain valuable insights into neuropathic pain, including both its molecular signature, somatosensory profiles and clusters of individuals related to pain severity, we analysed clinical data together with data obtained from quality of life pain-questionnaires. -

Clinical Exome Sequencing Tip Sheet – Medicare Item Numbers 73358/73359
Clinical exome sequencing Tip sheet – Medicare item numbers 73358/73359 Glossary Chromosome microarray (CMA or molecular Monogenic conditions (as opposed karyotype): CMA has a Medicare item number to polygenic or multifactorial conditions) are for patients presenting with intellectual caused by variants in a single gene. Variants disability, developmental delay, autism, or at may be inherited (dominant or recessive least two congenital anomalies. CMA is the fashion), or may occur spontaneously (de recommended first line test in these cases as novo) showing no family history. it can exclude a chromosome cause of disease which is unlikely to be detected by Whole exome sequence – sequencing only exome. the protein coding genes (exons). The exome is ~2% of the genome and contains ~85% of Gene panel is a set of genes that are known to disease-causing gene variants. be associated with a phenotype or disorder. They help narrow down the search Whole genome sequence – sequencing the for variants of interest to genes with evidence entire genome (all genes, including coding linking them to particular phenotypes and noncoding regions) Human phenotype ontology (HPO) terms Singleton – Analysis of the child only. describe a phenotypic abnormality using a Trio – analysis of the child and both biological standard nomenclature. Ideally, all clinicians parents. and scientists are using the same terms. Variant - A change in the DNA code that Mendeliome refers to the ~5,000 genes (out of differs from a reference genome. about 20,000 protein coding genes) that are known to be associated with monogenic disease. As variants in new genes are identified with evidence linking them with human disease, they are added to the Mendeliome. -
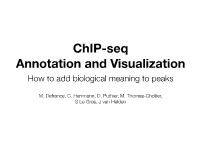
Chip-Seq Annotation and Visualization How to Add Biological Meaning to Peaks
ChIP-seq Annotation and Visualization How to add biological meaning to peaks M. Defrance, C. Herrmann, D. Puthier, M. Thomas-Chollier, S Le Gras, J van Helden Our data in the context Custom track uploded by the user (here ESR1 peaks in siGATA3 context) public UCSC annotation/data tracks Typical questions - What are the genes associated to the peaks? ChIP-seq peaks - Are some genomic categories over-represented? - Are some functional categories over-represented? - Are the peaks close to the TSS, …? ChIP-seq peaks Annotation Visualisation Enrichment profiles Annotated peaks Genomic & functional Average Profile near TSS Average Profile near TTS Annotation Genomic location Relation to CpG island 0.30 1.0 2500 0.8 chr start end Gene 0.25 chr15 65294195 65295186 0.6 chrX 19635923 19638359 Chst7 Average Profile Average Profile Average 3000 chr8 33993863 33995559 1500 0.4 0.20 chr10 114236977 114239326 Trhde # of regions # of regions 0.2 Distribution of Peak Heights chrX 69515082 69516482 Gabre 500 chr4 49857142 49858913 Grin3a 1000 −3000 −2000 −1000 0 1000 2000 3000 −3000 −2000 −1000 0 1000 2000 3000 0 5 10 15 chr16 7352861 7353410 Rbfox1 0 0 Relative Distance to TSS (bp) Relative Distance to TTS (bp) chr7 64764156 64765421 Gabra5 ChIP Regions (Peaks) over Chromosomes Average Gene Profile chrX 83436881 83438330 Nr0b1 CGI Shore Distant chr10 120288598 120289143 Msrb3 Multiple 1 Promoter Intergenic 2 chr5 67446361 67446855 Limch1 Gene Body 3 0.8 4 5 6 7 0.6 8 9 Average Profile Average 10 0.4 11 12 Chromosome 13 0.2 14 15 −1000 0 1000 2000 3000 4000 16 Upstream (bp), 3000 bp of Meta−gene, Downstream (bp) 17 18 19 Average Concatenated Exon Profile Average Concatenated Intron Profile X Y 0.0e+00 5.0e+07 1.0e+08 1.5e+08 2.0e+08 1.0 Chromosome Size (bp) 1.0 0.8 0.8 0.6 0.6 Average Profile Average Profile Average 0.4 0.4 0.2 0.2 0 20 40 60 80 100 0 20 40 60 80 100 Relative Location (%) Relative Location (%) Distribution of Peak Heights 0 5 10 15 ChIP Regions (Peaks) over Chromosomes 1 2 3 4 5 6 7 8 9 10 11 12 Chromosome W.Huang et al. -

Exome Sequencing in Early Disease Diagnosis
Diabetes Updates Short Communication ISSN: 2631-5483 Exome Sequencing in early disease diagnosis: Are we on the right track? Musambil M* Department of Genetics, Strategic Center for Diabetes Research, King Saud University, Riyadh, Saudi Arabia Identification of genetic variants associated with monogenic to whole exome sequencing (WES) and targeted gene sequencing. syndromes, complex disorders and related traits opened up an avenue But WGS still remains very much expensive compared with WES and that had not been explored before, which is to translate the genetic targeted sequencing [6] (Tables 1 and 2). screening information into disease predicting tools which could WES could be briefly explained as the process of sequencing provide more efficient management of the disease by improving risk exons or the protein-encoding parts of the genes which represent and its prediction capabilities. The methods to uncover the genetics of these complex disorders have evolved over time. The International the functional part of the genome. WES gives a clear picture of high HapMap Project, carried out as a part of the Human Genome Project, penetrance allelic variation and its relationship to disease phenotype was successful in providing information about more than one million [7]. As WES targets exons and with the knowledge that Mendelian or SNPs (Single Nucleotide Polymorphisms) across the human genome. partly Mendelian variations are mediated by non-synonymous, splice A revolution in SNP genotyping technology had occurred, making it site and frameshift variations, exomes remain the most ideal regions possible to genotype hundreds of thousands of SNPs, opening new to be screened in order to link genetic variation to health and disease. -

Supplementary Information For
Supplementary Information for Increased Muscleblind levels by chloroquine treatment improve myotonic dystrophy type 1 phenotypes in in vitro and in vivo models. Ariadna Bargiela, Maria Sabater-Arcis, Jorge Espinosa-Espinosa, Miren Zulaica, Adolfo Lopez de Munain and Ruben Artero. Corresponding author: Ruben Artero Email: [email protected] This PDF file includes: Supplementary text Figs. S1 to S13 Tables S1 References for SI reference citations 1 www.pnas.org/cgi/doi/10.1073/pnas.1820297116 Supplementary Information Text Materials and methods. Fly strains and crosses w1118 line was obtained from the Bloomington Drosophila Stock Center (Indiana University, Bloomington, IN, USA). Mhc-Gal4 flies were described in (1). Mhc-Gal4 UAS-(CTG)480 flies were generated in (2). All crosses were carried out at 25 °C with standard fly food. For oral administration of chloroquine (Chloroquine diphosphate salt solid, ≥98%, C6628 Sigma Aldrich), a maximum of 25 one-day adult flies were collected in tubes containing standard food supplemented with chloroquine (10 or 100 μM). Flies were transferred to tubes containing fresh food every 2-3 days for a total administration time of 7 days. Determination of caspase-3 and caspase-7 activity Ten adult female flies of the indicated genotypes were homogenized in 100 μl of cold PBS buffer using TissueLyser LT (Qiagen, Hilden, Germany). After a 10 min centrifugation, the supernatant was transferred into a white 96-well plate. Caspase-3 and caspase-7 activity was measured using the Caspase-Glo 3/7 Assay Systems (Promega, Fitchburg, WI, USA). Briefly, 100 μl of Caspase-Glo 3/7 reagent was added per well and the plate was incubated at room temperature for 30 min. -

Microarray and Pattern Miner Analysis of AXL and VIM Gene Networks in MDA‑MB‑231 Cells
MOLECULAR MEDICINE REPORTS 18: 4147-4155, 2018 Microarray and pattern miner analysis of AXL and VIM gene networks in MDA‑MB‑231 cells SUDHAKAR NATARAJAN1, VENIL N SUMANTRAN2, MOHAN RANGANATHAN1 and SURESH MADHESWARAN1 1Department of Biotechnology, Faculty of Engineering and Technology; 2Dr. A.P.J. Abdul Kalam Centre for Excellence in Innovation and Entrepreneurship, Dr. M.G.R. Educational and Research Institute, Tamil Nadu, Chennai 600095, India Received March 20, 2018; Accepted August 2, 2018 DOI: 10.3892/mmr.2018.9404 Abstract. MDA-MB-231 cells represent malignant triple-nega- migration, metastasis and chemoresistance, whereas the VIM tive breast cancer, which overexpress epidermal growth factor gene network regulates novel tumorigenic processes, such as receptor (EGFR) and two genes (AXL and VIM) associated lipogenesis, senescence and autophagy. Notably, these two with poor prognosis. The present study aimed to identify novel networks contain 12 genes not reported for TNBC. therapeutic targets and elucidate the functional networks for the AXL and VIM genes in MDA-MB-231 cells. We identi- Introduction fied 71 genes upregulated in MDA-MB-231 vs. MCF7 cells using BRB-Array tool to re-analyse microarray data from six Triple negative breast cancers (TNBC) lack expression of three GEO datasets. Gene ontology and STRING analysis showed important receptors (ER, PR, and HER2). These cancers account that 43/71 genes upregulated in MDA-MB-231 compared with for 10-15% of breast cancers, and are characterized by overex- MCF7 cells, regulate cell survival and migration. Another pression of epidermal growth factor receptor (EGFR), high 19 novel genes regulate migration, metastases, senescence, proliferative rate, and mutations in the p53 and BRCA1 tumour autophagy and chemoresistance. -
Guide to Interpreting Genomic Reports: a Genomics Toolkit
Guide to Interpreting Genomic Reports: A Genomics Toolkit A guide to genomic test results for non-genetics providers Created by the Practitioner Education Working Group of the Clinical Sequencing Exploratory Research (CSER) Consortium Genomic Report Toolkit Authors Kelly East, MS, CGC, Wendy Chung MD, PhD, Kate Foreman, MS, CGC, Mari Gilmore, MS, CGC, Michele Gornick, PhD, Lucia Hindorff, PhD, Tia Kauffman, MPH, Donna Messersmith , PhD, Cindy Prows, MSN, APRN, CNS, Elena Stoffel, MD, Joon-Ho Yu, MPh, PhD and Sharon Plon, MD, PhD About this resource This resource was created by a team of genomic testing experts. It is designed to help non-geneticist healthcare providers to understand genomic medicine and genome sequencing. The CSER Consortium1 is an NIH-funded group exploring genomic testing in clinical settings. Acknowledgements This work was conducted as part of the Clinical Sequencing Exploratory Research (CSER) Consortium, grants U01 HG006485, U01 HG006485, U01 HG006546, U01 HG006492, UM1 HG007301, UM1 HG007292, UM1 HG006508, U01 HG006487, U01 HG006507, R01 HG006618, and U01 HG007307. Special thanks to Alexandria Wyatt and Hugo O’Campo for graphic design and layout, Jill Pope for technical editing, and the entire CSER Practitioner Education Working Group for their time, energy, and support in developing this resource. Contents 1 Introduction and Overview ................................................................ 3 2 Diagnostic Results Related to Patient Symptoms: Pathogenic and Likely Pathogenic Variants . 8 3 Uncertain Results -

Personalised Medicine: the Odyssey from Hope to Practice
Journal of Personalized Medicine Review Personalised Medicine: The Odyssey from Hope to Practice Sophie Visvikis-Siest 1,2,*,†, Vesna Gorenjak 1,† and Maria G. Stathopoulou 1,† 1 Inserm, IGE-PCV, Université de Lorraine, 54000 Nancy, France; [email protected] (V.G.); [email protected] (M.G.S.) 2 Department of Internal Medicine and Geriatrics, CHU Technopôle Nancy-Brabois, Rue du Morvan, F-54511 Vandoeuvre-lès-Nancy, France * Correspondence: [email protected]; Tel.: +33-6-0760-2569 † These authors contributed equally to this work. Received: 4 September 2018; Accepted: 18 September 2018; Published: 21 September 2018 Abstract: In this endeavour, inspired by the Odyssey, we aim to embark with the reader on a journey on a ship from Troy to Ithaca, coursing through the history of the momentous events and achievements that paved the way for personalised medicine. We will set sail amidst important genetic discoveries, beginning with the discovery of the first human genome, and voyage through the projects that contributed to the progress of pharmacogenomic studies. Concurrently, we will propose methods to overcome the obstacles that are slowing the potential full implementation of accumulated knowledge into everyday practice. This journey aims to reflect on the frontiers of current genetic knowledge and the practical use of this knowledge in preventive, diagnostic and pharmacogenomic approaches to directly impact the socio-economic aspects of public health. Keywords: personalised medicine; pharmacogenomics; ethics; omics; Odyssey 1. The Journey from DNA Structure to Personalised Medicine “Tell me, O Muse, of that ingenious hero who travelled far and wide after he had sacked the famous town of Troy.