2020 Legislative Agenda
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protect Your Collective Bargaining Rights!
PROTECT YOUR COLLECTIVE BARGAINING RIGHTS! On April 26th, a majority of the members of the Massachusetts of House Representatives voted to dramatically restrict the rights of municipal employees to collectively bargain over the issue of health insurance. It is critically important that you let your Representative know how you feel about their vote. These Representatives voted IN FAVOR of your collective bargaining rights: Democrats: Geraldo Alicea Denise Andrews Bruce Ayers Michael Brady Paul Brodeur Thomas Calter Christine Canavan James Cantwell Tackey Chan Nicholas Collins Edward Coppinger Geraldine Creedon Mark Cusack Marcos Devers James Dwyer Lori Ehrlich Christopher Fallon Robert Fennell John Fresolo Denise Garlick Coleen Garry John Mahoney Paul Mark James Miceli Kevin Murphy Rhonda Nyman James O’Day Thomas Petrolati Denise Provost Kathi-Anne Reinstein Carl Sciortino Joyce Spiliotis Thomas Stanley David Sullivan Walter Timilty Timothy Toomey Cleon Turner Marty Walsh Steven Walsh Alice Wolf Republicans: Bradford Hill Daniel Winslow If your state representative stood up for you, it is important that you call them and thank them for their support. You can say something like this: My name is ____________________ and I live in __________________. I work for the city/town of ___________ as a _____________. I am calling because Rep. ____________ voted in favor of maintaining collective bargaining rights for municipal workers like me. I wanted to thank Rep. ______________ for standing up for my union rights. These Representatives voted AGAINST -

2013-2014 Legislative Scorecard
Legislative Scorecard Votes and Leadership 2013-14 LEGISLATIVE SESSION - 1 - This is the inaugural edition of the Environmental League of Massachusetts legislative scorecard. We produced this scorecard to inform citizens about how their legislators voted on important environmental issues. We are pleased and grateful for the support of so many environmental leaders in the legislature. The scorecard relies first on roll call votes on legislation that deals with environmental and energy issues. Because there are so few roll call votes each session—and often these votes are unanimous—we have scored additional actions by legislators to further distinguish environmental champions. Bonus points were awarded to legislators who introduced bills that were ELM priorities or who introduced important amendments, particularly budget amendments to increase funding for state environmental agencies. In addition, we subtracted points for legislators who introduced legislation or amendments that we opposed. We want to recognize leadership and courage, in addition to votes, and have made every attempt to be fair and transparent in our scoring. Much happens during the legislative process that is impractical to score such as committee redrafts, committee votes to move or hold a bill, and measures that would improve flawed legislation. We have not attempted to include these actions, but we recognize that they greatly influence the process and outcomes. None of the bills or amendments scored here should be a surprise to legislators in terms of ELM’s support or opposition. Going forward, ELM will include votes and other actions that support additional revenues for transportation and promote transit, walking and biking. George Bachrach, President Erica Mattison, Legislative Director Highlights of the Session projects. -

An Act to Provide Identification to Homeless Youth and Families
________________________________________________________________________________________________ Everyone Needs ID: An Act to Provide Identification to Homeless Youth and Families Senate Bill 2043 and House Bill 3066 Sponsored by Senator Harriette Chandler and Representative Kay Khan Lead Sponsors: Senator Harriette Chandler and Representative Kay Khan Senate Cosponsors: Senators Will Brownsberger, Jo Comerford, Julian Cyr, Sal DiDomenico, Jamie Eldridge, Cindy Friedman, Pat Jehlen, Jason Lewis, Mike Moore, and Becca Rausch House Cosponsors: Representatives Ruth Balser, Natalie Blais, Daniel Carey, Mike Connolly, Dan Donahue, Marjorie Decker, Mindy Domb, Carolyn Dykema, Nika Elugardo, Tricia Farley-Bouvier, Sean Garballey, Carmine Gentile, Carlos González, Tami Gouveia, James Hawkins, Kevin Honan, Mary Keefe, David LeBoeuf, Jack Patrick Lewis, David Linsky, Adrian Madaro, Liz Malia, Paul Mark, Paul McMurtry, Liz Miranda, Jim O’Day, Elizabeth Poirier, Denise Provost, Dave Rogers, Lindsay Sabadosa, Jon Santiago, Tom Stanley, José Tosado, Steve Ultino, Aaron Vega, and Bud Williams Bill History: Both Senate Bill 2043 and House Bill 3066 were refiled in January 2019, and were reported out favorably by the Joint Committee on Transportation in November 2019. S. 2043 was sent to the Senate Committee on Ways and Means, and may come up for a vote by the full Senate soon. H. 3066 was sent to the Joint Committee on Health Care Financing, and is awaiting action. Last session, the bill (Senate Bill 2568) passed the Senate unanimously. Importance of -
View the Vote Chart
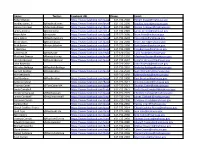
UPDATE THE BOTTLE BILL YES! I pledge to help. The Bottle Bill (5¢ deposit on some beverage containers) is the single most successful recycling tool in the country. But the Updated Bottle Bill—adding water, juice and sports drinks to the deposits—is being blocked by powerful business interests on Beacon Hill. The Updated Bottle Bill (H890/S1650) will reduce litter, increase recycling, and save cities and towns money in trash disposal and litter cleanup. In fact, 208 cities and towns, 375 small businesses, and 90 state and local organizations have endorsed our campaign and joined the effort to pass this bill. Despite this overwhelming support, the Updated Bottle Bill has been “bottled up” in the Legislature for more than a decade. It has never been brought to the floor for a vote, and we need your help now. No more delays! Here’s how you can help: STEP 1: To find out the name of your representative and senator, go to www.WhereDoIVoteMA.com STEP 2: Find out where your legislators stand on the Updated Bottle Bill. See the back of this flyer for a complete guide. STEP 3: Call your state senator and representative today. The State House main number is (617) 722- 2000. Ask for your senator (and then call back and ask for your representative). Tell them: “I am a voter in (name your town) and I support the Updated Bottle Bill. There should be no more delays, this bill needs to come up for a vote now.” (If your legislator supports the Updated Bottle Bill, make sure to thank them, if they are undecided or not supporting the bill, ask them to consider supporting the bill.) STEP 4: After you call, please email [email protected] to let us know your legislator’s response. -

An Act to Promote Public Safety and Better Outcomes for Young Adults – S.825/H.3420
An Act to Promote Public Safety and Better Outcomes for Young Adults – S.825/H.3420 Lead Sponsors MASSACHUSETTS CURRENTLY SPENDS THE MOST MONEY ON Sen. Joseph Boncore (Winthrop) YOUNG ADULTS IN THE JUSTICE SYSTEM AND GETS THE Rep. James O'Day (West Boylston) Rep. Kay Khan (Newton) WORST OUTCOMES Co-Sponsors Shifting 18- to 20-year-olds into the juvenile system, where Rep. Ruth Balser (Newton) they must attend school and participate in rehabilitative Rep. Christine Barber (Somerville) programming, would lower recidivism. The young adult Sen. Michael Brady (Brockton) brain is still developing making them highly amenable to Rep. Mike Connolly (Cambridge) rehabilitation. This development is influenced – Sen. Brendan Crighton (Lynn) positively or negatively – by their environment. Rep. Daniel Cullinane (Dorchester) Sen. Julian Cyr (Truro) An overly punitive approach can actually cause more Rep. Marjorie Decker (Cambridge) Rep. Marcos Devers (Lawrence) offending: Most young people "age out" of offending by their Sen. Sal DiDomenico (Everett) mid-twenties, particularly with developmentally appropriate Rep. Daniel Donahue (Worcester) interventions. Exposure to toxic environments, like adult jails Rep. Carolyn Dykema (Holliston) and prisons, entrenches young people in problematic Sen. James Eldridge (Acton) behaviors, increasing probability of recidivism. Rep. Tricia Farley-Bouvier (Pittsfield) Sen. Cindy Friedman (Arlington) Recidivism among young people incarcerated in the adult Rep. Sean Garballey (Arlington) corrections is more than double similar youth released Rep. Carlos González (Springfield) from department of youth services commitment Rep. Tami Gouveia (Acton) Teens and young adults incarcerated in Massachusetts’ adult Rep. Jim Hawkins (Attleboro) correctional facilities have a 55% re-conviction rate, Rep. Stephan Hay (Fitchburg) compared to a similar profile of teens whose re-conviction Rep. -

Massachusetts Caucus of Women Legislators
Massachusetts Caucus of Women Legislators STATE HOUSE R O O M 4 6 0 BOSTON MASSACHUSETTS 02133 617 722 2266 Winter 2013 Senator Candaras and Representative Balser to Lead Caucus President Therese Murray (D-Plymouth), who reviewed what had been accomplished during the last legislative session and discussed continuing oversight on agencies throughout the Commonwealth, finding balances with gun control, and drinking and wastewater issues. She also discussed the importance of keeping the focus on economic drivers such as healthcare and tourism and fighting for struggling industries like fishing and agriculture. The new Co-Chairs then started their term with an overview of the Caucus’ bylaws, specifically the purpose, which is to enhance the economic status and equality of women and encourage and to support women in all levels of government. Two themes emerged after a lively discussion with Caucus members: pay equity and professional development. To meet these themes, the Caucus agreed to sponsor events focusing on pay equity, invite spokespersons on both sides of the pay equity issue so that their colleagues and the public would be [R-L] Representative Denise Andrews (D-Orange), Co-Chair Representative Ruth privy to all viewpoints, and become educated and conversant on Balser (D-Newton), Co-Chair Senator Gale Candaras (D-Wilbraham), and Bethany the topic. Caucus members suggested ideas like tracking a day in Stevens, Deputy Chief Appeals & Training Bureau in the Middlesex DA’s Office the life of an average female, securing visits from both members attend Caucus’ Bills Co-sponsorship event. of big corporations in the private sector and public figures such as Senator Elizabeth Warren, and ensuring as much publicity as In January, Senator Gale Candaras (D-Wilbraham) and possible for these issues and events to spark interest in the Representative Ruth Balser (D-Newton) succeeded Senator general population of Massachusetts. -

METCO Legislators 2020
Phone (617) Address for newly District Senator/Representative First Name Last Name 722- Room # Email elected legislators Boston Representative Aaron Michlewitz 2220 Room 254 [email protected] Boston Representative Adrian Madaro 2263 Room 473-B [email protected] Natick, Weston, Wellesley Representative Alice Hanlon Peisch 2070 Room 473-G [email protected] East Longmeadow, Springfield, Wilbraham Representative Angelo Puppolo 2006 Room 122 [email protected] Boston Representative Rob Consalvo [email protected] NEW MEMBER Needham, Wellesley, Natick, Wayland Senator Becca Rausch 1555 Room 419 [email protected] Reading, North Reading, Lynnfield, Middleton Representative Bradley H. Jones Jr. 2100 Room 124 [email protected] Lynn, Marblehead, Nahant, Saugus, Swampscott, and Melrose Senator Adam Gomez [email protected] NEW MEMBER Longmeadow, Hampden, Monson Representative Brian Ashe 2430 Room 236 [email protected] Springfield Representative Bud Williams 2140 Room 22 [email protected] Springfield Representative Carlos Gonzales 2080 Room 26 [email protected] Sudbury and Wayland, Representative Carmine Gentile 2810 Room 167 [email protected] Boston Representative Chynah Tyler 2130 Room 130 [email protected] Woburn, Arlington, Lexington, Billerica, Burlington, Lexington Senator Cindy Friedman 1432 Room 413-D [email protected] Boston Senator Nick Collins 1150 Room 410 [email protected] Newton, Brookline, Wellesley Senator Cynthia Stone Creem 1639 Room 312-A [email protected] Boston, Milton Representative Dan Cullinane 2020 Room 527-A [email protected] Boston, Milton Representative Fluker Oakley Brandy [email protected] Boston, Chelsea Representative Daniel Ryan 2060 Room 33 [email protected] Boston Representative Daniel J. -

An Act Requiring Mental Health Parity for Disability Policies H. 908/S
An act requiring mental health parity for disability policies H. 908/S. 615 Summary of Issue Currently there are discriminatory limitations in private short- and long-term disability policies on benefits paid to persons disabled by mental disorders. Either no benefits are paid to these workers or they are paid for a shorter period of time than persons disabled by physical disorders. Sponsor of Act: Rep. Ruth Balser, Sen. Joan Lovely co-sponsors: Sen. James Eldridge, Sen. Pat Jehlen, Sen. John Keenan, Sen. Bruce Tarr, Sen. Sal DiDomenico, Sen. Michael Barrett, Sen. Diana DiZoglio, Sen. Joanne Comerford, Sen. Brendan Crighton, Sen. Rebecca Rausch, Rep. Thomas Stanley, Rep. Mike Connolly, Rep. Lori Ehrlich, Rep. Carlos Gonzalez, Rep. Christine Barber, Rep. Tram Nguyen, Rep. Elizabeth Malia, Rep. Sean Garballey, Rep. Kay Khan, Rep. Michael Day, Rep. Adrian Madaro, Rep. Denise Provost, Rep. Mathew Muratore, Rep. Angelo Puppolo, Jr., Rep. David Linsky, Rep. Steven Ultrino, Rep. Ken Gordon, Rep. Angelo Scaccia, Rep. Carmine Gentile, Rep. Jay Livingstone, Rep. James J. O’Day, Rep. Jose Tosado, Rep. Bud Williams, Rep. Liz Miranda, Rep. David Rogers, Rep. Mary Keefe, Rep. Daniel Cahill, Rep. Colleen Garry, Rep. Tami Gouveia, Rep. Natalie Higgins, Rep. Mindy Domb, Rep. Marjorie Decker, Rep. Jon Santiago, Rep. David Henry Argosky LeBoeuf, Rep. Christopher Hendricks, Rep. David Biele, Rep. Brian Murray. Status: Joint Committee on Financial Services Partial list of current and former organizational supporters: Attorney General Maura Healey, Disability -
Name: Twitter: Facebook URL Phone: Email: Robert Deleo
Name: Twitter: Facebook URL Phone: Email: Robert DeLeo https://www.facebook.com/pages/House-Speaker-Robert-A-DeLeo/401891743246684617-722-2500 [email protected] Bradley Jones, Jr. @RepBradJones https://www.facebook.com/brad.jones.5832617-722-2100 [email protected] Denise Andrews @deniseandrews https://www.facebook.com/deniseandrews2012617-722-2460 [email protected] James Arciero @JimArciero https://www.facebook.com/jim.arciero617-722-2320 [email protected] Brian Ashe @repashe https://www.facebook.com/pages/State-Representative-Brian-Ashe/313981658724617-722-2090 [email protected] Cory Atkins @RepCoryAtkins https://www.facebook.com/pages/Representative-Cory-Atkins/43717444568617-722-2692 [email protected] Bruce Ayers @BruceJAyers https://www.facebook.com/pages/Massachusetts-State-Representative-Bruce-J-Ayers/450787785367617-722-2230 [email protected] Ruth Balser @repruthbalser https://www.facebook.com/ruth.b.balser617-722-2396 [email protected] F. Barrows https://www.facebook.com/pages/State-Representative-F-Jay-Barrows/380289168915617-722-2488 [email protected] Carlo Basile @RepBasile https://www.facebook.com/repbasile617-626-0736 [email protected] Matthew Beaton @beatonforrep https://www.facebook.com/pages/Matt-Beaton-for-State-Representative/10150091953615647617-722-2230 [email protected] Jennifer Benson @RepJenBenson https://www.facebook.com/pages/Jen-Benson/9704649510617-722-2637 [email protected] John Binienda 617-722-2692 [email protected] -

MASC Legislative Directory 2020
2020 Massachusetts State Legislative Directory Massachusetts Constitutional Officers Governor Charlie Baker (617) 725-4005 Room 280 Lt. Governor Karyn Polito (617) 725-4005 Room 360 Treasurer Deborah Goldberg (617) 367-6900 Room 227 Atty. General Maura Healey (617) 727-2200 1 Ashburton Place, 18th Floor [email protected] Sec. of the State William Galvin (617) 727-9180 Room 340 [email protected] State Auditor Suzanne Bump (617) 727-2075 Room 230 [email protected] Massachusetts Senate (617) 722- Email (@masenate.gov) Room # (617) 722- Email (@masenate.gov) Room # Michael Barrett 1572 Mike.Barrett 109-D Patricia Jehlen 1578 Patricia.Jehlen 424 Joseph Boncore 1634 Joseph.Boncore 112 John Keenan 1494 John.Keenan 413-F Michael Brady 1200 Michael.Brady 416-A Edward Kennedy 1630 Edward.Kennedy 70 William Brownsberger 1280 William.Brownsberger 319 Eric Lesser 1291 Eric.Lesser 410 Harriette Chandler 1544 Harriette.Chandler 333 Jason Lewis 1206 Jason.Lewis 511-B Sonia Chang-Diaz 1673 Sonia.Chang-Diaz 111 Joan Lovely 1410 Joan.Lovely 413-A Nick Collins 1150 Nick.Collins 312-D Mark Montigny 1440 Mark.Montigny 312-C Joanne Comerford 1532 Jo.Comerford 413-C Michael Moore 1485 Michael.Moore 109-B Cynthia Creem 1639 Cynthia.Creem 312-A Patrick O'Connor 1646 Patrick.OConnor 419 Brendan Crighton 1350 Brendan.Crighton 520 Marc Pacheco 1551 Marc.Pacheco 312-B Julian Cyr 1570 Julian.Cyr 309 Rebecca Rausch 1555 Becca.Rausch 218 Sal DiDomenico 1650 Sal.DiDomenico 208 Michael Rodrigues 1114 Michael.Rodrigues 212 Diana DiZoglio 1604 Diana.DiZoglio 416-B -

Ocn432661025-2010-2Nd Quarter.Pdf
Caucus of Women Legislators ROOM 460 STATE HOUSE BOSTON MASSACHUSETTS 02133 617 722 2266 2nd Quarter 2010 Caucus Showcases Girls Inc. lens; gathering data on girls’ compromised, the health of their needs and strengths and work- children is too; if educational ing to identify strategies to sup- opportunities are not available, DATES port girls across the Common- their earning power and the abil- wealth. ity to care for their children is ―Girls Inc. is all about provid- compromised. The health and ing opportunities for girls. From well being of the girls and 2009/2010 the opportunity to have a safe women in a community is the Close to 50 legislators and place; to get homework help; to strongest barometer of the over- Legislative Session staff attended a presentation visit museums, women’s bas- all health and resiliency of the ends given by Girls Inc at the State ketball games and women- community.‖ July 31, 2010 House in May. Girls Inc., owned businesses; to opportuni- There are over 12,000 girls in which offers gender specific ties to be leaders in our commu- Massachusetts benefitting from programming internationally, nities by testifying at city coun- Girls Inc. programming, many of was represented at the State cil meetings, organizing park- whom are most at-risk for the Celebrate the House by program directors cleanups and proposing regula- very issues Girls Inc. addresses. 90th Anniversary from across the Commonwealth tions around drug parapherna- Suzanne Parker, Executive Di- of participating in a forum held by lia, Girls Inc. offers concrete rector of Girls Inc. of Holyoke, Women’s Suffrage the Caucus. -

The Statement
Massachusetts Caucus of Women Legislators State House, Room 460 Boston, MA 02133 – 1045 WWW.MAWOMENSCAUCUS.COM FOR IMMEDIATE RELEASE Contact: July 19th, 2019 Nicole Stephens Executive Director 617-412-8380 Massachusetts Caucus of Women Legislators Stand with Congresswomen BOSTON – We are a bipartisan and bicameral Caucus and certainly have a range of policy opinions in our ranks, but we value and respect each and every one of our members. One of the guiding principles of the MCWL is to “encourage and support women in all levels of government.” We stand in support of our colleague Congresswoman Ayanna Pressley and Congresswomen Ocasio-Cortez, Omar, and Tlaib. We condemn the racist and incendiary language volleyed at them by the President of the United States—that language has no place in the United States of America or in the halls of government. Representative Liz Malia Senator Cindy Friedman House Chair of the MCWL Senate Chair of the MCWL Speaker Pro-Tempore Patricia Haddad Senate President Karen Spilka Representative Ruth Balser Representative Mindy Domb Representative Christine Barber Representative Michelle DuBois Representative Jennifer Benson Representative Carolyn Dykema Representative Natalie Blais Representative Lori Ehrlich Representative Linda Campbell Representative Nika Elugardo Senator Harriette Chandler Representative Farley-Bouvier Representative Michelle Ciccolo Representative Kim Ferguson Senator Joanne Comerford Representative Carole Fiola Senator Cynthia Creem Representative Denise Garlick Representative Claire Cronin