Recommendations of the Advisory Committee on Immunization Practices for Use of Herpes Zoster Vaccines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treating Herpes Zoster and Postherpetic Neuralgia
® VOVOLL XX I XXIII• NO 1• NO• JU 4N E• MAY2013 2015 Treating Herpes Zoster and Postherpetic Neuralgia Vol.ÊXXI,ÊIssueÊ1Ê JuneÊ2013 Editorialostherpetic Board neuralgia (PHN) but a minority of patients experience months and 15% had pain at 2 years in is the most frequent chronic pain (PHN) persisting for months, years, a Dutch study.6 In the landmark zoster Editor-in-Chief PsychosocialÊAspectsÊofÊChronicÊPelvicÊPain complication of herpes zoster or even a lifetime. vaccine study, which included almost JaneÊC.ÊBallantyne,ÊMD,ÊFRCA (shingles).1 Herpes zoster (HZ) Anesthesiology,ÊPainÊMedicine 40,000 people aged 60 years or older PUSA represents a reactivation of the vari- Epidemiology of HZ and PHN (of whom fewer than 1000 developed cella zoster virus (VZV), a ubiquitous, Pain is unwanted, is unfortunately common, and remains essential for survival (i.e., AdvisoryÊBoard HZ) and where PHN was defined as highly neurotropic, exclusively human Accordingevading toda ang recenter) and systematic facilitating medical diagnoses. This complex amalgamation of MichaelÊJ.ÊCousins,ÊMD,ÊDSC pain intensity of 3/10 or more, 30% of -herpesvirus. Primary infection causes review,sensati theon, incidence emotions, of a ndHZ t houghis 3–5 ts manifests itself as pain behavior. Pain is a moti- α PainÊMedicine,ÊPalliativeÊMedicine 1patients who developed HZ had PHN - Australia casesvati perng f1000actor person-years.for physician 3c Theonsu ltations and for emergency department visits and is varicella (chickenpox), after which VZV at 1 month, 12% at 3 months, and 5% age-specific incidence rates of HZ were becomes latent in sensory ganglia along at 6 months in the placebo group.7 Ac- similar across countries, with a steep the entire neuraxis. -

Update on Herpes Zoster: Treatment and Prevention of Shingles 27Th Annual Primary Health Care of Women Conference
UPDATE ON HERPES ZOSTER: TREATMENT AND PREVENTION OF SHINGLES 27TH ANNUAL PRIMARY HEALTH CARE OF WOMEN CONFERENCE DECEMBER 5, 2019 PAMELA G. ROCKWELL, DO, FAAFP ASSOCIATE PROFESSOR DEPARTMENT OF FAMILY MEDICINE UNIVERSITY OF MICHIGAN NO FINANCIAL DISCLOSURES • AAFP Liaison of the Advisory Committee on Immunization Practices (ACIP) • AAFP Liaison ACIP Hepatitis, Pediatric and Adult RSV, and General Recommendations Work Groups • MAFP Liaison MDHHS Immunizations Committee • Co-Chair Immunization Committee, University of Michigan GOALS AND OBJECTIVES • Review Varicella Zoster Virus infection • Review Herpes Zoster (Shingles) Disease & Epidemiology • Review Shingles Risk Factors & Complications • Learn How to Diagnose and Treat Shingles and Common Complications • Learn How to Best Prevent Shingles/Update on Vaccination VARICELLA ZOSTER VIRUS (VZV) • Human α-herpesvirus, present worldwide, highly infectious • Primary infection with VZV causes varicella (chicken pox) • CDC estimate: ~ 4 million cases annually prior to 1995 • Annual incidence15-16 cases per 1,000 U.S. population • High annual burden of disease with hospitalization • 100-150 deaths per year https://www.cdc.gov/chickenpox/about/index.html CHICKENPOX • Transmitted person to person by direct contact, inhalation of aerosols from vesicular fluid of skin lesions of acute varicella or zoster (shingles), or aerosolized infected respiratory tract secretions CHICKENPOX • >95% of people born before 1980 in the U.S infected with wild-type VZV despite having no recall of disease* • VZV remains -

Non-Live Recombinant Herpes Zoster Vaccine (SHINGRIX)
Rx Files: Q&A Summary www.RxFiles.ca - Updated May 2021 Originally prepared by: M Jin, PharmD Non-Live Recombinant Herpes Zoster Vaccine (SHINGRIX) P L Bottom Line… SHINGRIX is indicated for the prevention of herpes zoster (HZ or shingles) in adults age ≥ 50 SHINGRIX reduces the risk of shingles by 91% (ARR=3.1%, NNT=32) & postherpetic neuralgia (PHN) by ~90% (ARR=0.30%, NNT=333) in 3 yrs. NNT: Eg. for every 333 vaccinated with SHINGRIX, 10 shingle cases (age ≥ 50 years) and 1 PHN cases (age ≥50 years) were prevented over ~ 3 yrs. SHINGRIX demonstrated efficacy for prevention of shingles effective in all age groups 50-80+. ZOSTAVAX less effective with increasing age. SHINGRIX use in patients with a history of shingles has been studied {open-label, non-randomized trial (n=93 patients, age 50-89 yr) for 3 months}.ZOSTER-033 Vaccine can be given after shingles symptoms/rash resolved CDC or ≥1 yr CDN Cost ~ $ 300 for 2 doses given intramuscularly (IM) 2-6 months apart (can give up to 12 months apart if needed to increase compliance). (Refrigerate 2 to 8°C; Discard if frozen) (New Jan/2021 NIHB covers for those between 65 & 70 years of age) Canadian NACI’18 recommends SHINGRIX should be offered to individuals ≥50 yrs without contraindications including: -Individuals previously vaccinated with ZOSTAVAX or ZOSTAVAX II; Re-vaccinate with two doses of RZV at least one year after receiving ZOSTAVAX -Individuals with a previous episode of herpes zoster disease. Provide two doses of SHINGRIX at least one year after herpes zoster episodeexpert opinion -Immunocompromised individuals, may be considered on a case-by-case assessment of the benefits vs risks expert opinion ZOSTAVAX II may be considered for immunocompetent individuals ≥50 yrs without contraindications when SHINGRIX is contraindicated, unavailable or inaccessible. -

View Board (KMUH-IRB-EXEMPT- We Further Investigated Whether HF Is a Time- 20130059)
Wu et al. BMC Infectious Diseases (2015) 15:17 DOI 10.1186/s12879-015-0747-9 RESEARCH ARTICLE Open Access A nationwide population-based cohort study to identify the correlation between heart failure and the subsequent risk of herpes zoster Ping-Hsun Wu1,4, Yi-Ting Lin2, Chun-Yi Lin6, Ming-Yii Huang3, Wei-Chiao Chang5,7 and Wei-Pin Chang6* Abstract Background: The association between heart failure (HF) and herpes zoster has rarely been studied. We investigated the hypothesis that HF may increase the risk of herpes zoster in Taiwan using a nationwide Taiwanese population- based claims database. Method: Our study cohort consisted of patients who received a diagnosis of HF in 2001 ~ 2009 (N = 4785). For a comparison cohort, three age- and gender-matched control patients for every patient in the study cohort were selected using random sampling (N = 14,355). All subjects were tracked for 1 year from the date of cohort entry to identify whether or not they had developed herpes zoster. Cox proportional-hazard regressions were performed to evaluate 1-year herpes zoster-free survival rates. Results: The main finding of this study was that patients with HF seemed to be at an increased risk of developing herpes zoster. Of the total patients, 211 patients developed herpes zoster during the 1-year follow-up period, among whom 83 were HF patients and 128 were in the comparison cohort. The adjusted hazard ratio (AHR) of herpes zoster in patients with HF was higher (AHR: 2.07; 95% confidence interval (CI): 1.54 ~ 2.78; p < 0.001) than that of the controls during the 1-year follow-up. -

Volume 27 • Number 1 • 2010
Newsletter A publication of the Controlled Release Society Volume 27 • Number 1 • 2010 What’s Inside New C&DP Representative Joins Newsletter Board Portland Awaits Phase Separation Behavior of Fusidic Acid in Microspheres Tailoring In Vitro Cell Responses of Porous Silicon Nanoencapsulation Using Microfluidizer® Processors Gamma Scintigraphy and Canine Respiratory Models News from the CRS Focus Groups CRS-AAPS Workshop a Success C&DP Patent Watch IT’S ALL ABOUT THE CONTENT That’s why subscribers of Drug Delivery Technology spend 40 minutes reading each issue. Drug Delivery Technology is the only publication completely dedicated to product development. Highlight your message to our 20,000 subscribers through print and online marketing opportunities! Y 10 printed issues Y eNewsletter sent twice per month, featuring the latest news CONTACT US TODAY shaping the industry (lim ited to 5 sponsors per month) EAST & MIDWEST Victoria Geis • Tel: (703) 212- 7735 • [email protected] Y Website Banner Advertising WEST Y Webinars and webcasts Warren DeGraff • Tel: (415) 721-0664 • [email protected] INTERNATIONAL Y Listings in the Resource Directory Ralph Vitaro • Tel: (973) 263-5476 • [email protected] (All listings in print and the digital WEBINARS version posted online) Michael J. Masters • 973-299-1200 • [email protected] Newsletter Steven Giannos Vol. 27 • No. 1 • 2010 Editor Table of Contents From the Editor ................................................................................................................. -

Communicable Disease (CD) Quarterly Report San Francisco Department of Public Health 2018 Quarter 2 • November 26, 2018
Communicable Disease (CD) Quarterly Report San Francisco Department of Public Health 2018 Quarter 2 • November 26, 2018 Disease Reporting: 415-554-2830 (phone); 415-554-2848 (fax); http://www.sfcdcp.org Tomás Aragón, MD, DrPH, Health Officer Juliet Stoltey, MD, MPH, Director, Communicable Disease Control and Prevention The Communicable Disease Control Unit receives and responds to reports of communicable diseases. For urgent reports during business hours, please call (415) 554-2830. For urgent or emergent reports after hours, please call (415) 554-2830 and follow instructions to contact the on-call physician. For non-urgent reports, please fax a Confidential Morbidity Report (CMR) to (415) 554-2848. Please see our website for more information: http://www.sfcdcp.org Sign up to receive Health Alerts at: https://www.sfcdcp.org/health-alerts-emergencies/health-alerts/register-for-health-alerts/ Table 1: Number of Selected Reported Communicable Disease Cases Current Recommendations for Shingles Prevention 2018 2017 Herpes zoster, or shingles, is a painful vesicular rash caused by reactivation of Q2 Q1-Q2 Q2 Q1-Q2 the varicella-zoster virus (VZV, the virus that causes chickenpox). The rash most commonly occurs in a dermatomal distribution and usually heals in 2-4 weeks. Botulism 0 0 1 1 In 10-13% of cases over age 50, a painful postherpetic neuralgia develops that Invasive Meningococcal Disease 0 0 0 0 may last for weeks, months, and occasionally, years. Risk of shingles increases # with age; CDC estimates a 50% lifetime risk in persons living to age 85. Altered Meningitis— Bacterial 1 4 4 6 immunocompetence increases the risk for shingles as well as risk of severe Meningitis— Viral 7 9 2 4 complications. -

Budget-Impact Analysis of Alternative Herpes Zoster Vaccine Strategies: a U.S
RESEARCH Budget-Impact Analysis of Alternative Herpes Zoster Vaccine Strategies: A U.S. HMO Perspective Jonathan Graham, BS; Josephine Mauskopf, PhD; Kosuke Kawai, ScD; Kelly D. Johnson, PhD, MPH; Ruifeng Xu, PhD; and Camilo J. Acosta, MD, PhD, MSc ABSTRACT driven primarily by vaccination costs. The results of the scenario analyses BACKGROUND: A herpes zoster vaccine has been approved by the FDA for showed that lower vaccination costs because of the application of copay- use in prevention of herpes zoster in individuals who are aged 50 years or ments for a managed care organization reduced the magnitude of the total older. The Advisory Committee on Immunization Practices (ACIP) recom- cost increase associated with the increase in uptake. mends vaccination only in individuals who are aged 60 years and older. CONCLUSIONS: Vaccinating individuals aged 50 to 59 years with the herpes zoster vaccine would likely have an impact on a health plan’s budget OBJECTIVES: To (a) estimate the overall budget and health impact of either because of the expected increase in the total number of individuals being the introduction of a new vaccination strategy (individuals over the age vaccinated in the population, with limited cost savings because of fewer of 50 years vs. individuals over the age of 60 years) within a hypothetical cases of herpes zoster. Higher coverage of vaccinations resulted in a greater health plan or simply an increase in coverage within the population aged increase in total costs each year. However, increasing coverage would also 60 years and over and (b) discern what effect copayments and changes to result in a decrease in the number of individuals developing zoster and copayments have on the health plan’s budget. -

Recombinant Zoster (Shingles) Vaccine
VACCINE INFORMATION STATEMENT Many Vaccine Information Statements are available in Spanish and other languages. Recombinant Zoster (Shingles) See www.immunize.org/vis Hojas de información sobre vacunas están disponibles en español y en muchos otros Vaccine: What You Need to Know idiomas. Visite www.immunize.org/vis 1 Why get vaccinated? Recombinant shingles 2 vaccine Recombinant zoster (shingles) vaccine can prevent shingles. Recombinant shingles vaccine provides strong protection against shingles. By preventing shingles, Shingles (also called herpes zoster, or just zoster) is recombinant shingles vaccine also protects against a painful skin rash, usually with blisters. In addition PHN. to the rash, shingles can cause fever, headache, chills, or upset stomach. More rarely, shingles can lead Recombinant shingles vaccine is the preferred to pneumonia, hearing problems, blindness, brain vaccine for the prevention of shingles. However, a inflammation (encephalitis), or death. different vaccine, live shingles vaccine, may be used in some circumstances. The most common complication of shingles is long-term nerve pain called postherpetic neuralgia The recombinant shingles vaccine is recommended (PHN). PHN occurs in the areas where the shingles for adults 50 years and older without serious rash was, even after the rash clears up. It can last for immune problems. It is given as a two-dose series. months or years after the rash goes away. The pain This vaccine is also recommended for people who from PHN can be severe and debilitating. have already gotten another type of shingles vaccine, the live shingles vaccine. There is no live virus in this vaccine. Shingles vaccine may be given at the same time as other vaccines. -

Postherpetic Neuralgia
Journal of Pain & Palliative Care Pharmacotherapy. 2011;25:187–189. Copyright © 2011 Informa Healthcare USA, Inc. ISSN: 1536-0288 print / 1536-0539 online DOI: 10.3109/15360288.2010.550990 PATIENT EDUCATION AND SELF-ADVOCACY: QUESTIONS AND RESPONSES ON PAIN MANAGEMENT Edited by Yvette Colon´ Postherpetic Neuralgia Naileshni Singh ABSTRACT Questions from patients about analgesic pharmacotherapy and responses from authors are presented to help educate patients and make them more effective self-advocates. The topic addressed in this issue is postherpetic neuralgia, symptoms, risk factors, and treatment. KEYWORDS acyclovir, capsaicin, corticosteroids, herpes zoster, lidocaine, neuropathic analgesics, posther- petic neuralgia, shingles, varicella-zoster QUESTION FROM A PATIENT tion and the chronic pain syndrome of postherpetic neuralgia. In their youth, many people have had I had shingles earlier in the year and thought I re- chicken pox, which is caused by the same virus, covered well, but I still have a lot of pain. My doctor called varicella-zoster. After this first infection, it is calls it postherpetic neuralgia. What are the best treat- thought that the virus lies within the sensory nerves For personal use only. ments for it and how can I get rid of the pain? I’m 57 in the spinal cord. With older age or in patients with years old and in fairly good health otherwise. poor immune systems, the virus can often “reacti- vate” and cause a rash accompanied by pain. The pain may subside, but in certain instances, individ- Answer uals may develop persistent pain that can last for sev- Postherpetic neuralgia (PHN) can be an unfortunate eral years. -
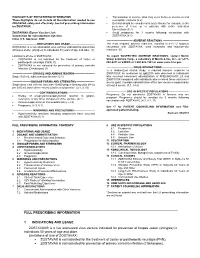
Full Prescribing Information 1 Indications and Usage Zostavax
HIGHLIGHTS OF PRESCRIBING INFORMATION Transmission of vaccine virus may occur between vaccinees and These highlights do not include all the information needed to use susceptible contacts (5.2) ZOSTAVAX safely and effectively. See full prescribing information Deferral should be considered in acute illness (for example, in the for ZOSTAVAX. presence of fever) or in patients with active untreated tuberculosis (5.3) ZOSTAVAX® (Zoster Vaccine Live) Avoid pregnancy for 3 months following vaccination with Suspension for subcutaneous injection ZOSTAVAX (8.1) Initial U.S. Approval: 2006 ------------------------------ ADVERSE REACTIONS ------------------------------ ----------------------------INDICATIONS AND USAGE ---------------------------- The most frequent adverse reactions, reported in ≥1% of subjects ZOSTAVAX is a live attenuated virus vaccine indicated for prevention vaccinated with ZOSTAVAX, were headache and injection-site of herpes zoster (shingles) in individuals 50 years of age and older. (1) reactions. (6) Limitations of Use of ZOSTAVAX: To report SUSPECTED ADVERSE REACTIONS, contact Merck ZOSTAVAX is not indicated for the treatment of zoster or Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877- postherpetic neuralgia (PHN) (1) 888-4231 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov. ZOSTAVAX is not indicated for prevention of primary varicella infection (Chickenpox) (1) -------------------------------DRUG INTERACTIONS------------------------------- In a randomized clinical study, a reduced immune response to ----------------------- DOSAGE AND ADMINISTRATION------------------------ ZOSTAVAX as measured by gpELISA was observed in individuals Single 0.65 mL subcutaneous injection (2.1) who received concurrent administration of PNEUMOVAX® 23 and ZOSTAVAX compared with individuals who received these vaccines 4 --------------------- DOSAGE FORMS AND STRENGTHS --------------------- weeks apart. Consider administration of the two vaccines separated by Single dose vials with not less than 19,400 plaque-forming units [PFU] at least 4 weeks. -

Book Review Editorial
BookEditorial Review Two Ounces of Prevention Jeffrey M. Weinberg, MD iven the morbidity and treatment challenges Herpes zoster is another disease for which a new posed by many disease states, prevention of vaccine is in development. The incidence and severity G those conditions clearly would be a preferable of this condition and the associated postherpetic neu- alternative. Over the past year, we have observed exam- ralgia increases with age, and we have an increasingly ples of progress in this direction, especially in the field aging population. Oxman et al3 conducted a large study of infectious diseases. The 2 most recent prevention to determine if vaccination against varicella-zoster strategies will have direct relevance to dermatologists. virus would decrease the incidence, severity, or both of In October 2005, Merck announced that an inves- herpes zoster and postherpetic neuralgia among older tigational vaccine (quadrivalent human papillo- adults. They enrolled 38,546 subjects 60 years or mavirus [HPV] types 6, 11, 16, and 18, recombinant older in a randomized, double-blind, placebo-controlled vaccine) prevented 100% of high-grade cervical pre- trial of an investigational live attenuated Oka/Merck cancers and noninvasive cervical cancers associated varicella-zoster virus vaccine (“zoster vaccine”). The with HPV types 16 and 18 in a recent phase 3 study pain and discomfort associated with herpes zoster were (PϽ.001).1 The analysis compared the vaccine to measured repeatedly for 6 months. The primary end placebo in women who were not infected with HPV point was the burden of illness due to herpes zoster, a types 16 and 18 at enrollment and who remained free measure affected by the incidence, severity, and dura- of infection through the completion of the vaccina- tion of the associated pain and discomfort. -

Management of Varicella
Management of Varicella Clinical scenarios 1) 'Kids have got chicken pox and granny is coming to stay – could she catch it? She's had it before': If you have ever had chicken pox you are considered immune for life. However 10% of the UK adult population are seronegative i.e. not immune. She could previously have been misdiagnosed as having chicken pox and therefore NOT be immune. As chicken pox is often a more serious infection in adults it may be sensible that she remains at home. 2) Should we have a chicken pox party: Mortality is 4-9/100 000 infections. 80% of these will be in adults i.e. more serious infection in adults. 20% of the above deaths will still be in children – so can still represent risk. If was to recommend a 'chicken pox party' and the child then died after contracting chicken pox would this be medico-legally defensible? The clinician could discuss the risks, numbers etc with the parent but the ultimate decision and consequences of that decision should reside with the parent. 3) 'I'm a primary school teacher. I'm 8 weeks pregnant and a child in my class has got chicken pox. What should I do'? Pregnant women are 5 times more likely to die than non-pregnant women should they develop chicken pox in pregnancy. Has she ever had chicken pox? Risk is only if she is non-immune. Test for antibodies to varicella zoster. A significant exposure is classed as 5 mins face to face or 15 mins in the same room with someone 48h before lesions appear and until last lesion has crusted over.