Premature Ejaculation: Practice Essentials, Background, Pathophysiology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE PHYSIOLOGY and ECOPHYSIOLOGY of EJACULATION Tropical and Subtropical Agroecosystems, Vol
Tropical and Subtropical Agroecosystems E-ISSN: 1870-0462 [email protected] Universidad Autónoma de Yucatán México Lucio, R. A.; Cruz, Y.; Pichardo, A. I.; Fuentes-Morales, M. R.; Fuentes-Farias, A.L.; Molina-Cerón, M. L.; Gutiérrez-Ospina, G. THE PHYSIOLOGY AND ECOPHYSIOLOGY OF EJACULATION Tropical and Subtropical Agroecosystems, vol. 15, núm. 1, 2012, pp. S113-S127 Universidad Autónoma de Yucatán Mérida, Yucatán, México Available in: http://www.redalyc.org/articulo.oa?id=93924484010 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Tropical and Subtropical Agroecosystems, 15 (2012) SUP 1: S113 – S127 REVIEW [REVISIÓN] THE PHYSIOLOGY AND ECOPHYSIOLOGY OF EJACULATION [FISIOLOGÍA Y ECOFISIOLOGÍA DE LA EYACULACIÓN] R. A. Lucio1*, Y. Cruz1, A. I. Pichardo2, M. R. Fuentes-Morales1, A.L. Fuentes-Farias3, M. L. Molina-Cerón2 and G. Gutiérrez-Ospina2 1Centro Tlaxcala de Biología de la Conducta, Universidad Autónoma de Tlaxcala, Tlaxcala-Puebla km 1.5 s/n, Loma Xicotencatl, 90062, Tlaxcala, Tlax., México. 2Depto. Biología Celular y Fisiología, Instituto de Investigaciones Biomédicas, Universidad Nacional Autónoma de México, Ciudad Universitaria, 04510, México, D.F., México. 3Laboratorio de Ecofisiologia Animal, Departamento de Fisiologia, Instituto de Investigaciones sobre los Recursos Naturales, Universidad Michoacana de San Nicolás de Hidalgo, Av. San Juanito Itzicuaro s/n, Colonia Nueva Esperanza 58337, Morelia, Mich., México * Corresponding author ABSTRACT RESUMEN Different studies dealing with ejaculation view this Diferentes estudios enfocados en la eyaculación, process as a part of the male copulatory behavior. -
Andrology User Handbook
Document code: AY.P001 Version number: 7 Date of issue: 29/06/2020 USER HANDBOOK FOR ANDROLOGY SERVICES Diagnostic Semen Analysis Post Vasectomy Semen Analysis Retrograde Ejaculation Analysis Page 1 of 24 Document code: AY.P001 Version number: 7 Date of issue: 29/06/2020 Contents: 1. Introduction .................................................................................................................... 3 2. Location and Opening Times .......................................................................................... 4 3. Useful contacts ............................................................................................................... 4 4. Services provided by the laboratory ............................................................................... 5 5. Requesting semen analysis ............................................................................................ 5 6. Analysis test types .......................................................................................................... 8 6.1 Diagnostic semen analysis (DSA) test for fertility ......................................................... 8 6.1a Instructions for collection of a semen sample for DSA (fertility)............................... 9 6.1b How Diagnostic Semen Analysis assessments are reported .................................10 6.2 Retrograde Analysis ....................................................................................................11 6.2a Instructions for collection of urine for retrograde ejaculation -

Erectile Dysfunction and Premature Ejaculation
GUIDELINES ON MALE SEXUAL DYSFUNCTION: Erectile Dysfunction and Premature Ejaculation (Text update April 2014) K. Hatzimouratidis (chair), I. Eardley, F. Giuliano, D. Hatzichristou, I. Moncada, A. Salonia, Y. Vardi, E. Wespes Eur Urol 2006 May;49(5):806-15 Eur Urol 2010 May;57(5):804-14 Eur Urol 2012 Sep;62(3):543-52 ERECTILE DYSFUNCTION Definition, epidemiology and risk factors Erectile dysfunction (ED) is the persistent inability to attain and maintain an erection sufficient to permit satisfactory sex- ual performance. Although ED is a benign disorder, it affects physical and psychosocial health and has a significant impact on the quality of life (QoL) of sufferers and their partners. There is increasing evidence that ED can be an early mani- festation of coronary artery and peripheral vascular disease; thus, ED should not be regarded only as a QoL issue but also as a potential warning sign of cardiovascular disease includ- ing lack of exercise, obesity, smoking, hypercholesterolaemia, and the metabolic syndrome. The risk of ED may be reduced by modifying these risk factors, particularly taking exercise or losing weight. Another risk factor for ED is radical prostatec- tomy (RP) in any form (open, laparoscopic, or robotic) because of the risk of cavernosal nerve injury, poor oxygenation of the corpora cavernosa, and vascular insufficiency. 130 Male Sexual Dysfunction Diagnosis and work-up Basic work-up The basic work-up (minimal diagnostic evaluation) outlined in Fig. 1 must be performed in every patient with ED. Due to the potential cardiac risks associated with sexual activity, the three Princeton Consensus Conference stratified patients with ED wanting to initiate, or resume, sexual activity into three risk categories. -

Sexually Transmitted Infections Treatment Guidelines, 2021
Morbidity and Mortality Weekly Report Recommendations and Reports / Vol. 70 / No. 4 July 23, 2021 Sexually Transmitted Infections Treatment Guidelines, 2021 U.S. Department of Health and Human Services Centers for Disease Control and Prevention Recommendations and Reports CONTENTS Introduction ............................................................................................................1 Methods ....................................................................................................................1 Clinical Prevention Guidance ............................................................................2 STI Detection Among Special Populations ............................................... 11 HIV Infection ......................................................................................................... 24 Diseases Characterized by Genital, Anal, or Perianal Ulcers ............... 27 Syphilis ................................................................................................................... 39 Management of Persons Who Have a History of Penicillin Allergy .. 56 Diseases Characterized by Urethritis and Cervicitis ............................... 60 Chlamydial Infections ....................................................................................... 65 Gonococcal Infections ...................................................................................... 71 Mycoplasma genitalium .................................................................................... 80 Diseases Characterized -

Therapy for Premature Ejaculation
pISSN: 2287-4208 / eISSN: 2287-4690 World J Mens Health 2016 December 34(3): 173-178 https://doi.org/10.5534/wjmh.2016.34.3.173 Review Article Ancient Chinese Fangzhongshu (Sexual Skills and Methods) Therapy for Premature Ejaculation Yong Zhu1, Qiang Chen2, Yuexing Gu1, Jin Yue1, Qingqi Zeng3 1Department of Andrology, Traditional Chinese Medicine Hospital of Yancheng City Affiliated with the Nanjing University of Chinese Medicine, Yancheng, 2Institute of Andrology, Nanjing University of Chinese Medicine, 3Department of Integrative Medicine, Jiangsu Jiankang Vocational College, Nanjing, China Premature ejaculation (PE) is a common male sexual dysfunction that can have significant effects on a couple’s relationship. Behavioral therapy and psychotherapy are both safe and effective methods of treating PE. Ancient Chinese fangzhongshu (sexual skills and methods), which reflects a summary of expert experiences in sexology, contains many therapies for sexual dysfunction that are similar to those used in behavioral therapy or psychotherapy. A brief introduction dealing with the latest definitions of PE and treatment strategies drawn from behavioral therapy and psychotherapy is provided. Typical therapies for PE from ancient Chinese fangzhongshu are listed and briefly analyzed in order to define their domain of applicability and instructions for use. Ancient Chinese fangzhongshu contains many effective and safe therapies for PE. It should be incorporated into modern medical practice after critical analysis, and its scientific aspects should be promoted as a way of improving reproductive health, both to benefit individuals affected by PE and to promote traditional Chinese culture. Based on an analysis of the condition of the individual patient, one or multiple therapies guided by fangzhongshu can be expected to have an effect on the patient. -

Fact Sheet from Reproductivefacts.Org
Fact Sheet From ReproductiveFacts.org The Patient Education Website of the American Society for Reproductive Medicine Intrauterine insemination (IUI) When a woman conceives naturally, sperm travel from the vagina is provided by the doctor’s office or andrology laboratory, a laboratory through the cervix (narrow, lower part of the womb), into the uterus that specializes in dealing with male health issues. Sperm can also be (womb), and up into one of the fallopian tubes. If sperm arrive in a tube collected during sex in a special condom that the doctor provides. If soon after the release of the egg from the ovary (ovulation); the sperm a man has retrograde ejaculation, the sperm can be retrieved in the and egg can meet and unite (fertilization) in the tube. laboratory from urine he has collected. The cervix naturally limits the number of sperm that enter the Men who have a difficult time with erection or ejaculation despite using uterus. This means that only a small percentage of the sperm in the medications, as well as men with a spinal cord injury, may be able ejaculate actually make their way into the fallopian tubes. Intrauterine to produce a sperm sample with the help of vibratory stimulation or insemination (IUI) is a procedure that places sperm past the cervix electroejaculation. Vibratory stimulation commonly takes place in an and in a woman’s uterus around the time of ovulation. This makes office and uses a handheld vibratory device. Electroejaculation uses the passage to the fallopian tubes much shorter, and there is a better electrical stimulation in order to produce a sperm specimen. -

Male Fertility Following Spinal Cord Injury: a Guide for Patients Second Edition
Male Fertility Following Spinal Cord Injury: A Guide For Patients Second Edition By Nancy L. Brackett, Ph.D., HCLD Emad Ibrahim, M.D. Charles M. Lynne, M.D. 1 2 This is the second edition of our booklet. The first was published in 2000 to respond to a need in the spinal cord injured (SCI) community for a source of information about male infertility. At that time, we were getting phone calls almost daily on the subject. Today, we continue to get numerous requests for information, although these requests now arrive more by internet than phone. These requests, combined with numerous hits on our website, attest to the continuing need for dissemination of this information to the SCI community as well as to the medical community. “The more things change, the more they stay the same.” This quote certainly holds true for the second edition of our booklet. In the current age of advanced reproductive technologies, numerous avenues for help are available to couples with male partners with SCI. Although the help is available, we have learned from our patients as well as our professional colleagues that not all reproductive medicine specialists are trained in managing infertility in couples with SCI male partners. In some cases, treatments are offered that may be unnecessary. It is our hope that the information contained in this updated edition of our booklet can be used as a talking point for patients and their medical professionals. The Male Fertility Research Program of the Miami Project to Cure Paralysis is known around the world for research and clinical efforts in the field of male infertility in the SCI population. -

A Man's Guide to Overcoming Premature Ejaculation
A man’s guide to overcoming Premature Ejaculation Premature ejaculation affects up to 30% of men at some time in their lives yet remains an embarrassing condition which men are uncomfortable talking about. Our guide to premature ejaculation will give you the lowdown on what causes the condition, the impact it can have and advice on a variety of treatments. THE CAUSES of Premature Ejaculation How the condition can occur Premature ejaculation is a common male medical condition yet the precise causes are still not fully understood. Despite its prevalence among men, the subject is largely taboo but failure to talk about or confront the issue often serves to exacerbate the problem for sufferers. Defining what exactly constitutes premature ejaculation can be difficult as different men come at different times – but if it’s a serious concern for both partners then that’s a good working definition of premature ejaculation. This guide talks through the types, causes and impact of premature ejaculation, separates the facts from the fiction, and finally offers advice on the variety of treatments available to help sufferers manage the condition. Let’s start by looking at the two broad types of premature ejaculation: Primary/Lifelong Premature Ejaculation This is where a man has suffered from premature ejaculation since becoming sexually active. It occurs from the first sexual encounter and continues throughout life, and can be attributed to physical or psychological factors or may be hereditary. Primary premature ejaculation is often triggered by psychological impulses, such as conditioning, upbringing, or a traumatic sexual experience. www.doctorfox.co.uk Secondary/Acquired Premature Ejaculation This is when a man goes years without suffering any ejaculation problems but then either gradually or suddenly begins to experience premature ejaculation. -
Investigation of Retrograde Ejaculation Sept 13
Car Parking Hospital District Yeovil main carparkat Department and Pathology Location of There are visitor pay and display car parks at both Taunton and Yeovil Hospitals. Somerset Pathology Service Andrology Investigation of Retrograde Ejaculation Appointments for Taunton & Yeovil 01823 343903 Hospital, Taunton Musgrove Park car parksat Department and Pathology Location of To help us improve our service we do run occasional patient satisfaction surveys, so you may be asked to complete a questionnaire for us when you attend the laboratory. Leaflet No 71009013 Q.pulse ARE_M001 09/13 Version 1.2 Author: P Hancock Please read and follow these Can my partner bring in my sample? First wash your hands and genitals with soap instructions thoroughly Provided she can let the laboratory know the and water, ensure complete removal of all soap Testing your sample entire sample has been collected, or if part was residues and dry thoroughly lost which part (first, middle or last part), and she Collect your semen sample by masturbation Please contact the Andrology secretary to knows your general health record, that is not a directly into the container. (Do NOT use a arrange an appointment for bringing in a problem. sheath/condom for collection as they will kill semen sample for testing. There will be a wait Is there anything that may affect my results? sperm. Other forms of sample collection are for an appointment, however, if you have a also not acceptable). Collect the entire sample. fertility clinic appointment do let the secretary Failure to follow the collection guidance can Once the semen sample is collected, empty your know the date when you telephone for an seriously alter semen analysis results. -

Male Sexual Dysfunction
Guidelines on Male Sexual Dysfunction: Erectile dysfunction and premature ejaculation K. Hatzimouratidis (Chair), I. Eardley, F. Giuliano, I. Moncada, A. Salonia © European Association of Urology 2015 TABLE OF CONTENTS PAGE 1. INTRODUCTION 4 1.1 Aim 4 1.2 Publication history 4 1.3 Panel composition 4 2. METHODS 4 3. THE GUIDELINE 5 3A ERECTILE DYSFUNCTION 5 3A.1 Epidemiology/aetiology/pathophysiology 5 3A.1.1 Epidemiology 5 3A.1.2 Risk factors 5 3A.1.3 Pathophysiology 5 3A.1.4 Post-radical prostatectomy ED, post-radiotherapy ED & post-brachytherapy ED 6 3A.1.5 Conclusions on the epidemiology/aetiology/pathophysiology of ED 7 3A.2 Classification 7 3A.3 Diagnostic evaluation 7 3A.3.1 Basic work-up 7 3A.3.2 Sexual history 7 3A.3.3 Physical examination 8 3A.3.4 Laboratory testing 8 3A.3.5 Cardiovascular system and sexual activity: the patient at risk 8 3A.3.5.1 Low-risk category 10 3A.3.5.2 Intermediate- or indeterminate-risk category 10 3A.3.5.3 High-risk category 10 3A.3.6 Specialised diagnostic tests 10 3A.3.6.1 Nocturnal penile tumescence and rigidity test 10 3A.3.6.2 Intracavernous injection test 10 3A.3.6.3 Duplex ultrasound of the penis 10 3A.3.6.4 Arteriography and dynamic infusion cavernosometry or cavernosography 10 3A.3.6.5 Psychiatric assessment 10 3A.3.6.6 Penile abnormalities 10 3A.3.7 Patient education - consultation and referrals 10 3A.3.8 Recommendations for the diagnostic evaluation of ED 11 3A.4. -

Developmental Status of Topical Therapies for Erectile and Ejaculatory Dysfunction
International Journal of Impotence Research (2000) 12, Suppl 4, S80±S85 ß 2000 Macmillan Publishers Ltd All rights reserved 0955-9930/00 $15.00 www.nature.com/ijir Developmental status of topical therapies for erectile and ejaculatory dysfunction A Morales1* 1Queen's University, Department of Urology, Kingston General Hospital, Kingston, Ontario, Canada The most common of the sexual dysfunctions in men are premature ejaculation and impotence. Large strides have been made in the treatment of erectile disturbances but only limited and temporary successes have been achieved in the therapy of ejaculatory abnormalities. This manuscript examines the realm of topical therapy, its current limitations and the challenges that must be addressed if topical therapy is ever to have a niche in the urologist's treatment armamentarium. Topical agents for the treatment of premature ejaculation include anesthetics and herbal medications. The limited nature of the studies reported to date does not yet permit a reliable assessment of their ef®cacy. For the treatment of erectile dysfunction, some of the drugs administered by various other systemic routes appear to have some ef®cacy when delivered transdermally. Again, the studies and results are too limited for the urologist to develop a clear opinion about their ef®cacy. Further investigation of these drugs with the use of absorption enhancers is needed. International Journal of Impotence Research (2000) 12, Suppl 4, S80±S85. Keywords: erectile dysfunction; premature ejaculation; topical therapy; review Introduction Oral,1 intraurethral2 and sublingual3 administration of drugs have opened new and more acceptable avenues of therapy for ED. In the case of PE, the The most common sexual complaints in men are picture is different. -
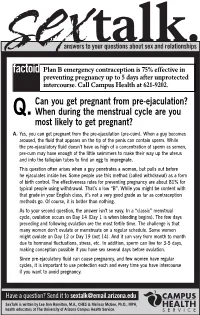
Q.Can You Get Pregnant from Pre-Ejaculation? When During The
answers to your questions about sex and relationships Plan B emergency contraception is 75% effective in preventing pregnancy up to 5 days after unprotected intercourse. Call Campus Health at 621-9202. Can you get pregnant from pre-ejaculation? Q. When during the menstrual cycle are you most likely to get pregnant? A. Yes, you can get pregnant from the pre-ejaculation (pre-cum). When a guy becomes aroused, the fluid that appears on the tip of the penis can contain sperm. While the pre-ejaculatory fluid doesn’t have as high of a concentration of sperm as semen, pre-cum may have enough of the little swimmers to make their way up the uterus and into the fallopian tubes to find an egg to impregnate. This question often arises when a guy penetrates a woman, but pulls out before he ejaculates inside her. Some people use this method (called withdrawal) as a form of birth control. The effectiveness rates for preventing pregnancy are about 81% for typical people using withdrawal. That’s a low “B”. While you might be content with that grade in your English class, it’s not a very good grade as far as contraception methods go. Of course, it is better than nothing. As to your second question, the answer isn’t so easy. In a “classic” menstrual cycle, ovulation occurs on Day 14 (Day 1 is when bleeding begins). The few days preceding and following ovulation are the most fertile time. The challenge is that many women don’t ovulate or menstruate on a regular schedule.