Appendix B: Provincial Case Definitions for Diseases of Public Health Significance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Presentation of Meningitis in Adults
Clinical Presentation of Meningitis in Adults Prof. Dr. Serhat Ünal FACP, FEFIM Hacettepe University, Faculty of Medicine Department of© Infectious by author Diseases , ANKARA Meningitis Update ESCMIDESCMID PostgraduateOnline Lecture Educational Library Course September 2013, İzmir Why Is Clinical Examination Important? "If, in a fever, the neck be turned awry on a sudden, so that the sick can hardly swallow, and yet no tumour appear, it is mortal.- © by author ESCMID“Aphorism Online XXXV Lecture of Hippocrates Library” Meningitis • Meningitis is a clinical syndrome characterized by inflammation of the meninges • Infectious Meningitis – caused by a variety of infectious agents • bacteria, viruses, fungi, and parasites. • Clinical signs and symptoms at presentation may predict prognosis • Only 25% of adults© by have author a classic presentation and are not a diagnostic dilemma. • ESCMIDMany patients Online have a Lecture less obvious Library presentation Mace SE, Emerg Med Clin N Am 2008;38:281 Spanos A et al JAMA 1998;262:2700 Clinicians Suspecting Meningitis • While taking the patient's history • Examine for – General symptoms of infection • such as fever, chills, and myalgias – Symptoms suggesting central nervous system infection © by author • photophobia, headache, nausea and vomiting, focal neurologic symptoms, or changes in mental status ESCMID Online Lecture Library Clinical Presantation of Meningitis (Dept. Of Emergency) The suspicion of ABM is critically dependent on the early recognition of the meningitis syndrome. • 156 patients with meningitis -Taiwan – I nitial ED diagnosis was correct in only 58% of the cases. • The 3 most common© by alternative author diagnoses – Nonmeningeal infection ESCMID– Metabolic encephalopathy Online Lecture Library – Nonspecific conditions Chern CH, Ann Emerg Med. -

Pentose Phosphate Pathway in Health and Disease: from Metabolic
UNIVERSIDADE DE LISBOA FACULDADE DE FARMÁCIA DEPARTAMENTO DE BIOQUÍMICA PENTOSE PHOSPHATE PATHWAY IN HEALTH AND DISEASE: FROM METABOLIC DYSFUNCTION TO BIOMARKERS Rúben José Jesus Faustino Ramos Orientador: Professora Doutora Maria Isabel Ginestal Tavares de Almeida Mestrado em Análises Clínicas 2013 Pentose Phosphate Pathway in health and disease: From metabolic dysfunction to biomarkers . Via das Pentoses Fosfato na saúde e na doença: Da disfunção metabólica aos biomarcadores Dissertação apresentada à Faculdade de Farmácia da Universidade de Lisboa para obtenção do grau de Mestre em Análises Clínicas Rúben José Jesus Faustino Ramos Lisboa 2013 Orientador: Professora Doutora Maria Isabel Ginestal Tavares de Almeida The studies presented in this thesis were performed at the Metabolism and Genetics group, iMed.UL (Research Institute for Medicines and Pharmaceutical Sciences), Faculdade de Farmácia da Universidade de Lisboa, Portugal, under the supervision of Prof. Maria Isabel Ginestal Tavares de Almeida, and in collaboration with the Department of Clinical Chemistry, VU University Medical Center, Amsterdam, The Netherlands, Dr. Mirjam Wamelink. De acordo com o disposto no ponto 1 do artigo nº 41 do Regulamento de Estudos Pós- Graduados da Universidade de Lisboa, deliberação nº 93/2006, publicada em Diário da Republica – II série nº 153 – de 5 julho de 2003, o autor desta dissertação declara que participou na conceção e execução do trabalho experimental, interpretação dos resultados obtidos e redação dos manuscritos. Para os meus pais e -

Hantavirus Infections
Revista MVZ Córdoba ISSN: 0122-0268 ISSN: 1909-0544 [email protected] Universidad de Córdoba Colombia Hantavirus Infections Guzmán T, Camilo; Calderón R, Alfonso; González T, Marco; Mattar V, Salim Hantavirus Infections Revista MVZ Córdoba, vol. 22, 2017 Universidad de Córdoba, Colombia Available in: http://www.redalyc.org/articulo.oa?id=69353273020 PDF generated from XML JATS4R by Redalyc Project academic non-profit, developed under the open access initiative Camilo Guzmán T, et al. Hantavirus Infections Revisión de Literatura Hantavirus Infections Infecciones por hantavirus Camilo Guzmán T Redalyc: http://www.redalyc.org/articulo.oa?id=69353273020 Universidad de Córdoba, Colombia [email protected] Alfonso Calderón R Universidad de Córdoba, Colombia [email protected] Marco González T Universidad de Córdoba, Colombia [email protected] Salim Mattar V Universidad de Córdoba, Colombia [email protected] Received: 16 August 2016 Accepted: 08 March 2017 Abstract: Hantaviruses are the causative agents of hantavirus pulmonary syndrome in humans in the Americas; e primary reservoirs are in the rodents of the subfamily Sigmodontinae. In South America, cases of hantavirus pulmonary syndrome caused by numerous viral genotypes have been diagnosed. In Colombia, different serological studies have reported the circulation of hantavirus in humans and rodents. ese viruses act in an intimate association with a rodent species that serves as a reservoir and have a distribution around the wild rodent, being limited to a specific geographic region. In South America, the first HPS-associated hantavirus was described in 1993 in Brazil and was called Juquitiva and from 1993 to 2012, more than 1400 cases had been identified in Brazil. -

Research Article
z Available online at http://www.journalcra.com INTERNATIONAL JOURNAL OF CURRENT RESEARCH International Journal of Current Research Vol. 9, Issue, 12, pp.62497-62502, December, 2017 ISSN: 0975-833X RESEARCH ARTICLE INCLUSION BODIES - A REVIEW 1Dr. Mrunalini Mahesh Dadpe, 2, *Dr. Sourab Kumar, 3Dr. Mahesh Dadpe, 4Dr. Payoshnee Bhalinge Jadhav, 5Dr. Abhishek Jadhav and 6Dr. Shilpi Suman 1, 4Department of Oral Pathology, M A Rangoonwala Dental College, Aazam Campus, Camp, Pune 411001, India 2, 5, 6Department of oral Pathology, D.Y. Patil School of Dentistry, Nerul, Navi Mumbai 400706, India 3MIDSR Dental College, Vishwanathpuram, Amba Jogai Road, Latur 413531, India ARTICLE INFO ABSTRACT Article History: The word inclusion means incorporation. Inclusion bodies are nuclear or cytoplasmic aggregates of Received 16th September, 2017 stainable substances which are usually ‘proteins’. They typically represent sites of viral multiplication Received in revised form in bacteria or in a eukaryotic cell and usually consist of viral capsid proteins. Inclusion bodies are 17th October, 2017 typically identified within a cell by their different appearance. Accepted 25th November, 2017 Published online 27th December, 2017 Key words: Proteins, Viral, Types, Structures Copyright © 2017, Mrunalini Mahesh Dadpe et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Citation: Dr. Mrunalini Mahesh Dadpe, Dr. Sourab Kumar, Dr. Mahesh Dadpe, Dr. Payoshnee Bhalinge Jadhav, Dr. Abhishek Jadhav and Dr. Shilpi Suman, 2017. “Inclusion Bodies - A Review”, International Journal of Current Research, 9, (12), 62497-62502. Classification INTRODUCTION Viral inclusion bodies Inclusion bodies (IB) can also be hallmarks of genetic diseases, as in the case of Neuronal Inclusion bodies in neural disorders, A. -
ECG in Pericarditis Pericardial Effusion Pericardium the Pericardium Is a Double Sheet Made up by Two Layers of Not So Distensible Fibrous Tissue That Wraps the Heart
Pericardial effusion with emphasis on the electrocardiographic aspects By Andrés Ricardo Pérez-Riera MDPhD ECG In pericarditis Pericardial effusion Pericardium The pericardium is a double sheet made up by two layers of not so distensible fibrous tissue that wraps the heart. The internal or visceral layer is adhered to the heart. The external or parietal layer is wrapped by the visceral one. Between both there is a space with a small amount of serofibrinous liquid (ö20 to 50 ml). The parietal layer fixes the heart in its place within the chest and prevents direct contact between the organ and neighboring structures. Functions of the pericardium The pericardium has three main functions: mechanical, membranous and ligamentous. Mechanical function: it restricts cardiac dilatation increasing the efficiency of the heart, maintaining ventricular compliance and distributing hydrostatic forces. Additionally, it creates a closed chamber with subatmospheric pressure, aiding atrial filling and reducing parietal transmural pressures. Membranous function: it protects the heart, reducing its external friction and acting as a barrier against propagation of infections and neoplasia’s. Ligamentous function: it anatomically fixes the heart, preventing the latter from balancing. Other functions: Barrier against infections; barrier against dissemination of neoplasias; preventing excessive movements of the organ; preventing direct contact of the heart with neighboring structures; conditioning less friction between the heart and other organs; allowing diastolic distention of the chambers due to negative atmospheric pressure. Pericarditis Concept of pericarditis: syndrome caused by inflammation of the pericardium, a sack made up by two sheets (parietal and visceral) that wrap the heart and the great vessels. Etiological classification of pericarditis • Idiopathic (unknown): 26-86% of cases. -

West Nile Virus Infection Lineages by Including Koutango Virus, a Related Virus That America
West Nile Virus Importance West Nile virus (WNV) is a mosquito-borne virus that circulates among birds, Infection but can also affect other species, particularly humans and horses. Many WNV strains are thought to be maintained in Africa; however, migrating birds carry these viruses to other continents each year, and some strains have become established outside West Nile Fever, Africa. At one time, the distribution of WNV was limited to the Eastern Hemisphere, and it was infrequently associated with serious illness. Clinical cases usually occurred West Nile Neuroinvasive Disease, sporadically in humans and horses, or as relatively small epidemics in rural areas. West Nile Disease, Most human infections were asymptomatic, and if symptoms occurred, they were Near Eastern Equine Encephalitis, typically mild and flu-like. Severe illnesses, characterized by neurological signs, Lordige seemed to be uncommon in most outbreaks. Birds appeared to be unaffected throughout the Eastern Hemisphere, possibly because they had become resistant to the virus through repeated exposure. Since the 1990s, this picture has changed, and WNV has emerged as a significant Last Updated: August 2013 human and veterinary pathogen in the Americas, Europe, the Middle East and other areas. Severe outbreaks, with an elevated case fatality rate, were initially reported in Algeria, Romania, Morocco, Tunisia, Italy, Russia and Israel between 1994 and 1999. While approximately 80% of the people infected with these strains were still asymptomatic, 20% had flu-like signs, and a small but significant percentage (<1%) developed neurological disease. One of these virulent viruses entered the U.S. in 1999. Despite control efforts, it became established in much of North America, and spread to Central and South America and the Caribbean. -

Heterogeneous Alleles Comprising G6PD Deficiency Trait in West Africa Exert Contrasting Effects on Two Major Clinical Presentations of Severe Malaria Shivang S
Shah et al. Malar J (2016) 15:13 DOI 10.1186/s12936-015-1045-0 Malaria Journal RESEARCH Open Access Heterogeneous alleles comprising G6PD deficiency trait in West Africa exert contrasting effects on two major clinical presentations of severe malaria Shivang S. Shah1,4*, Kirk A. Rockett1, Muminatou Jallow2, Fatou Sisay‑Joof2, Kalifa A. Bojang2, Margaret Pinder2, Anna Jeffreys1, Rachel Craik1, Christina Hubbart1, Thomas E. Wellems4, Dominic P. Kwiatkowski1,3 and MalariaGEN Consortium Abstract Background: Glucose-6-phosphate dehydrogenase (G6PD) deficiency exhibits considerable allelic heterogeneity which manifests with variable biochemical and clinical penetrance. It has long been thought that G6PD deficiency confers partial protection against severe malaria, however prior genetic association studies have disagreed with regard to the strength and specificity of a protective effect, which might reflect differences in the host genetic ‑back ground, environmental influences, or in the specific clinical phenotypes considered. Methods: A case-control association study of severe malaria was conducted in The Gambia, a region in West Africa where there is considerable allelic heterogeneity underlying expression of G6PD deficiency trait, evaluating the three major nonsynonymous polymorphisms known to be associated with enzyme deficiency (A968G, T542A, and C202T) in a cohort of 3836 controls and 2379 severe malaria cases. Results: Each deficiency allele exhibited a similar trend toward protection against severe malaria overall (15–26 % reduced risk); however, in stratifying severe malaria to two of its constituent clinical subphenotypes, severe malarial anaemia (SMA) and cerebral malaria (CM), the three deficiency alleles exhibited trends of opposing effect, with risk conferred to SMA and protection with respect to CM. -

Cardiovascular Semiotics: the Personalities Behind the Eponyms
International Journal of Cardiovascular Sciences. 2016;29(5):396-406 396 REVIEW ARTICLE Cardiovascular Semiotics: The Personalities Behind the Eponyms Renata Gudergues Pereira de Almeida1, Juliana dos Santos Macaciel1, Érico Araújo Reis Santos1, Thiago Calvet Cavalcanti Garcia1, Anastacia Midori Hashimoto1, Cláudio Tinoco Mesquita1,2 Departamento de Medicina Clínica – Faculdade de Medicina – Universidade Federal Fluminense1, Programa de Pós-Graduação em Ciências Cardiovasculares da UFF2, Niterói, RJ – Brazil Abstract observed in life today is also present in medicine and its teaching. Currently, many teachers and students Since its inception, medicine has been based tend to neglect cardiac auscultation in favor of on observation of signs and specific findings in ill imaging examinations to evaluate the heart, such as patients. Semiotics is, therefore, an ancient study. echocardiography and magnetic resonance imaging. Cardiac semiology, although more recent, is more However, it is worth noting that, in many cases, the complex in its learning due to difficulties in the reality of medicine distances patients from access interpretation of auscultatory findings. Austin Flint, to cardiovascular imaging examinations, even in Rivero Carvallo, Antonio Valsalva, and Adolf Kussmaul large centers. are some of the many physicians who have dedicated The lack of competence for cardiac auscultation themselves to the academic study of cardiac semiology can be seen in several countries around the world. and became eternalized in the medical field through -

Post-Traumatic Meningitis Is a Diagnostic Challenging Time: a Systematic Review Focusing on Clinical and Pathological Features
International Journal of Molecular Sciences Review Post-Traumatic Meningitis Is a Diagnostic Challenging Time: A Systematic Review Focusing on Clinical and Pathological Features Raffaele La Russa 1,2, Aniello Maiese 2,3, Nicola Di Fazio 1, Alessandra Morano 4, Carlo Di Bonaventura 4, Alessandra De Matteis 1, Valentina Fazio 1, Paola Frati 1,2 and Vittorio Fineschi 1,2,* 1 Department of Anatomical, Histological, Forensic and Orthopaedic Sciences, Sapienza University of Rome, Viale Regina Elena 336, 00161 Rome (RM), Italy; raff[email protected] (R.L.R.); [email protected] (N.D.F.); [email protected] (A.D.M.); [email protected] (V.F.); [email protected] (P.F.) 2 IRCSS Neuromed Mediterranean Neurological Institute, Via Atinense 18, 86077 Pozzilli (IS), Italy; [email protected] 3 Department of Surgical Pathology, Medical, Molecular and Critical Area, Institute of Legal Medicine, University of Pisa, 56126 Pisa (PI), Italy 4 Neurology Unit, Department of Neurosciences, Mental Health, “Sapienza” University, 00161 Rome (RM), Italy; [email protected] (A.M.); [email protected] (C.D.B.) * Correspondence: vfi[email protected] Received: 21 May 2020; Accepted: 8 June 2020; Published: 10 June 2020 Abstract: Post-traumatic meningitis is a dreadful condition that presents additional challenges, in terms of both diagnosis and management, when compared with community-acquired cases. Post-traumatic meningitis refers to a meningeal infection causally related to a cranio-cerebral trauma, regardless of temporal proximity. The PICO (participants, intervention, control, and outcomes) question was as follows: “Is there an association between traumatic brain injury and post-traumatic meningitis?” The present systematic review was carried out according to the Preferred Reporting Items for Systematic Review (PRISMA) standards. -

Eosinophilic Gastroenteritis: Clinical Manifestation, Natural Course and Evaluation Of
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2019 Eosinophilic Gastroenteritis: Clinical Manifestation, Natural Course, and Evaluation of Treatment with Corticosteroids and Vedolizumab Grandinetti, Tanja ; Biedermann, Luc ; Bussmann, Christian ; Straumann, Alex ; Hruz, Petr Abstract: BACKGROUND Eosinophilic gastroenteritis (EGE) is a rare, chronic inflammatory condition of the gastrointestinal tract. Little is known about its natural history and treatment outcomes. The aims of our analysis were to describe clinical presentation, response to current medical treatments, and to evaluate the response of refractory EGE to anti-integrin therapy. METHODS Patients with confirmed diagnosis of EGE fulfilling the diagnostic criteria: (1) the presence of gastrointestinal symptoms, (2)dense eosinophilic infiltration of the gastrointestinal mucosa, and (3) exclusion of other conditions leadingto gastrointestinal eosinophilia were included in this analysis. In patients non-responding to corticosteroids and/or anti-TNF treatment the integrin blocker vedolizumab was used. RESULTS EGE patients (n = 22) were predominantly female (63%) with a median age at diagnosis of 41.5 years. The most frequent symptoms were abdominal pain (100%), diarrhea (59%), nausea/vomiting (36%), and bloating (27%). No pathognomonic endoscopic alterations were found. Eosinophilic infiltration was observed in the majority of patients in more than one segment. Patients were treated with systemic steroids, topical, and enteral release steroids in 21/22 (95%) patients, proton pump inhibitors in 7/22 (32%), TNF inhibitors in 3/22 (14%), and vedolizumab in 4/22 (18%) patients. In 3/4 of steroid-refractory patients vedolizumab induced a clinical and histological improvement. CONCLUSIONS The combination of highly variable clinical presentation, subtle endoscopic abnormalities, and involvement of several GI segments undermines the difficulty to diagnose EGE and the need for structured biopsy sampling. -
Eosinophilic Gastroenteritis: Case Presentation
Grand Round Presentation Dipendra Parajuli 2-19-04 University of Louisville Case Report: -A 51 y/o causasian male was referred to a gastroenterology office by his primary care provider for the evaluation of new onset ascites. -The patient had been in his basal level of health till about three months prior to presentation at which time he had been prescribed some antibiotic for presumed prostatitis.University of Louisville -A few days after starting the antibiotic he started experiencing diffuse abdominal cramps associated with nausea, vomiting and watery diarrhea. -He also noticed some staining of the toilet paper with blood but denied any bleeding into the toilet bowl or bloody bowel movements. At this time he also had a low-grade fever. University of Louisville -He denied any chest pains or shortness of breath. -At about the same time however he also started noticing abdominal swelling which kept on increasing and he presented to his primary care provider and was subsequently referred. University of Louisville -PMH Hypertension and DJD and spinal disc disease for which he had had knee and cervical spine surgeries in the remote past. - Personal Hx did admit to heavy alcohol consumption in his younger days a habit he had quit someUniversity 25 years ago. of Louisville Physical Exam -middle aged w/m of stocky built , tattoo on each forearm. -Vital signs were stable and pt was anicteric -He had moderate ascites but none of the other stigmata of chronic liver disease. -Rest of the examination was unremarkable. University of Louisville LABS CBC WBC-16.7, -Neutrophils-38.9 %, - Lymphocytes-15%, HGB-15.3 Platelets -307 ESR-18 BMP Normal Values University of Louisville Liver profile Alk PO4 -89 AST -19 ALT -14 TP - 7.6 Alb -3.8 PT -11 Viral Hepatitis panel - Negative University of Louisville USN -Liver and GB with dopplers revealed cholelithiasis, shrunken liver, ascites and right pleural effusion. -
C O N F E R E N C E 15 17 January 2018
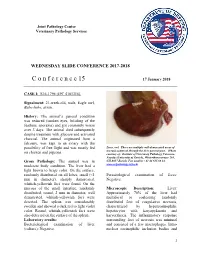
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2017-2018 C o n f e r e n c e 15 17 January 2018 CASE I: S16-1796 (JPC 4101316). Signalment: 21-week-old, male, Eagle owl, Bubo bubo, avian. History: The animal’s general condition was reduced (sunken eyes, bristling of the feathers, anorexia) and got constantly worse over 3 days. The animal died subsequently despite treatment with glucose and activated charcoal. The animal originated from a falconry, was kept in an aviary with the possibility of free flight and was mostly fed Liver, owl. There are multiple well-demarcated areas of necrosis scattered through the liver parenchyma. (Photo on chicken and pigeons. courtesy of: Institute of Veterinary Pathology Vetsuisse- Faculty (University of Zurich), Winterthurerstrasse 268, Gross Pathology: The animal was in CH-8057 Zurich, Fax number +41 44 635 89 34, moderate body condition. The liver had a www.vetpathology.uzh.ch) light brown to beige color. On the surface, randomly distributed on all lobes, small (<1 Parasitological examination of feces: mm in diameter), sharply demarcated, Negative. whitish-yellowish foci were found. On the mucosa of the small intestine, randomly Microscopic Description: Liver: distributed, round, 2 mm in diameter, well Approximately 70% of the liver had demarcated, whitish-yellowish foci were multifocal to coalescing randomly detected. The spleen was considerably distributed foci of coagulative necrosis, swollen and showed a dark red to light violet characterized by hypereosinophilic color. Round, whitish-yellowish foci were hepatocytes with karyopyknosis and also detected on the surface of the spleen. karyorrhexis. The inflammatory response Laboratory results: surrounding foci of necrosis was minimal Bacteriological examination of liver and consisted of a few macrophages.