Demodectic Mange
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plasma Pharmacokinetic Profile of Fluralaner (Bravecto™) and Ivermectin Following Concurrent Administration to Dogs Feli M
Walther et al. Parasites & Vectors (2015) 8:508 DOI 10.1186/s13071-015-1123-8 SHORT REPORT Open Access Plasma pharmacokinetic profile of fluralaner (Bravecto™) and ivermectin following concurrent administration to dogs Feli M. Walther1*, Mark J. Allan2 and Rainer KA Roepke2 Abstract Background: Fluralaner is a novel systemic ectoparasiticide for dogs providing immediate and persistent flea, tick and mite control after a single oral dose. Ivermectin has been used in dogs for heartworm prevention and at off label doses for mite and worm infestations. Ivermectin pharmacokinetics can be influenced by substances affecting the p-glycoprotein transporter, potentially increasing the risk of ivermectin neurotoxicity. This study investigated ivermectin blood plasma pharmacokinetics following concurrent administration with fluralaner. Findings: Ten Beagle dogs each received a single oral administration of either 56 mg fluralaner (Bravecto™), 0.3 mg ivermectin or 56 mg fluralaner plus 0.3 mg ivermectin/kg body weight. Blood plasma samples were collected at multiple post-treatment time points over a 12-week period for fluralaner and ivermectin plasma concentration analysis. Ivermectin blood plasma concentration profile and pharmacokinetic parameters Cmax,tmax,AUC∞ and t½ were similar in dogs administered ivermectin only and in dogs administered ivermectin concurrently with fluralaner, and the same was true for fluralaner pharmacokinetic parameters. Conclusions: Concurrent administration of fluralaner and ivermectin does not alter the pharmacokinetics -

Medical Parasitology
MEDICAL PARASITOLOGY Anna B. Semerjyan Marina G. Susanyan Yerevan State Medical University Yerevan 2020 1 Chapter 15 Medical Parasitology. General understandings Parasitology is the study of parasites, their hosts, and the relationship between them. Medical Parasitology focuses on parasites which cause diseases in humans. Awareness and understanding about medically important parasites is necessary for proper diagnosis, prevention and treatment of parasitic diseases. The most important element in diagnosing a parasitic infection is the knowledge of the biology, or life cycle, of the parasites. Medical parasitology traditionally has included the study of three major groups of animals: 1. Parasitic protozoa (protists). 2. Parasitic worms (helminthes). 3. Arthropods that directly cause disease or act as transmitters of various pathogens. Parasitism is a form of association between organisms of different species known as symbiosis. Symbiosis means literally “living together”. Symbiosis can be between any plant, animal, or protist that is intimately associated with another organism of a different species. The most common types of symbiosis are commensalism, mutualism and parasitism. 1. Commensalism involves one-way benefit, but no harm is exerted in either direction. For example, mouth amoeba Entamoeba gingivalis, uses human for habitat (mouth cavity) and for food source without harming the host organism. 2. Mutualism is a highly interdependent association, in which both partners benefit from the relationship: two-way (mutual) benefit and no harm. Each member depends upon the other. For example, in humans’ large intestine the bacterium Escherichia coli produces the complex of vitamin B and suppresses pathogenic fungi, bacteria, while sheltering and getting nutrients in the intestine. 3. -

ESCCAP Guidelines Final
ESCCAP Malvern Hills Science Park, Geraldine Road, Malvern, Worcestershire, WR14 3SZ First Published by ESCCAP 2012 © ESCCAP 2012 All rights reserved This publication is made available subject to the condition that any redistribution or reproduction of part or all of the contents in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise is with the prior written permission of ESCCAP. This publication may only be distributed in the covers in which it is first published unless with the prior written permission of ESCCAP. A catalogue record for this publication is available from the British Library. ISBN: 978-1-907259-40-1 ESCCAP Guideline 3 Control of Ectoparasites in Dogs and Cats Published: December 2015 TABLE OF CONTENTS INTRODUCTION...............................................................................................................................................4 SCOPE..............................................................................................................................................................5 PRESENT SITUATION AND EMERGING THREATS ......................................................................................5 BIOLOGY, DIAGNOSIS AND CONTROL OF ECTOPARASITES ...................................................................6 1. Fleas.............................................................................................................................................................6 2. Ticks ...........................................................................................................................................................10 -

Deconstructing Canine Demodicosis”
TESIS DOCTORAL TITULO: “Deconstructing canine demodicosis” AUTOR: Ivan Ravera DIRECTORES: Lluís Ferrer, Mar Bardagí, Laia Solano Gallego. PROGRAMA DE DOCTORADO: Medicina i Sanitat Animals DEPARTAMENTO: Medicina i Cirurgia Animals UNIVERSIDAD: Universitat Autònoma de Barcelona 2015 Dr. Lluis Ferrer i Caubet, Dra. Mar Bardagí i Ametlla y Dra. Laia María Solano Gallego, docentes del Departamento de Medicina y Cirugía Animales de la Universidad Autónoma de Barcelona, HACEN CONSTAR: Que la memoria titulada “Deconstructing canine demodicosis” presentada por el licenciado Ivan Ravera para optar al título de Doctor por la Universidad Autónoma de Barcelona, se ha realizado bajo nuestra dirección, y considerada terminada, autorizo su presentación para que pueda ser juzgada por el tribunal correspondiente. Y por tanto, para que conste firmo el presente escrito. Bellaterra, el 23 de Septiembre de 2015. Dr. Lluis Ferrer, Dra. Mar Bardagi, Ivan Ravera Dra. Laia Solano Gallego Directores de la tesis doctoral Doctorando AGRADECIMIENTOS A los alquimistas de guantes azules A los otros luchadores - Ester Blasco - Diana Ferreira - Lola Pérez - Isabel Casanova - Aida Neira - Gina Doria - Blanca Pérez - Marc Isidoro - Mercedes Márquez - Llorenç Grau - Anna Domènech - los internos del HCV-UAB - Elena García - los residentes del HCV-UAB - Neus Ferrer - Manuela Costa A los veterinarios - Sergio Villanueva - del HCV-UAB - Marta Carbonell - dermatólogos españoles - Mónica Roldán - Centre d’Atenció d’Animals de Companyia del Maresme A los sensacionales genetistas -

Review on Epidemiology of Camel Mange Mites
ISSN: 2574-1241 Volume 5- Issue 4: 2018 DOI: 10.26717/BJSTR.2018.08.001605 Wubishet Z. Biomed J Sci & Tech Res Mini Review Open Access Review on Epidemiology of Camel Mange Mites Jarso D1, Birhanu S1 and Wubishet Z*2 1Haramaya University College of Veterinary Medicine, Haramaya, Ethiopia 2Oromia Pastoralist Area Development Commission Yabello Regional Veterinary Laboratory, Ethiopia Received: August 10, 2018; Published: August 17, 2018 *Corresponding author: Wubishet Z, Oromia Pastoralist Area Development Commission Yabello Regional Veterinary Laboratory, Ethiopia Abstract We reviewed the paper to document the status of mange mite in camel raising arid and semi-arid areas of the world. Different published obtained online by web browsing and books from university library. Mange is caused by different species of Sarcoptus, Psoroptus, Chorioptus and Demodexresearch papersin camels. and This books parasite from is1980 important to 2018 parasite on ecto-parasites in camel raising of the area camel of the (including world. High mange infestations mites) wereare noted reviewed. during Published rainy season, papers at young were and old age, camel with poor body condition, and in large herds. Relatively, Sarcoptic mange caused by Sarcoptes scabieivarcameli is considered to be one of the most and economically important zoonotic and epizootic diseases with spread capacity among animals via direct physical contact with infested animal and indirectly through fomites.It is also one of the most prevalent type of camel mange. Occurrence of the disease is mostly associated with poor management and a mingling of diseased camels with healthy ones. Camel mange mite infestation usually starts from head region and then extends to the neck and other areas of the body with thin skin. -

Sarcoptic Mange in Cattle
March 2005 Agdex 663-47 Sarcoptic Mange in Cattle Sarcoptic mange, or barn itch, is a disease caused by the parasitic mite, Sarcoptes scabiei. Mange produced by this How do cattle get mange? mite can be severe because the mite burrows deeply into Infection is usually spread by direct contact between cattle. the skin, causing intense itching. Cattle affected by Straw bedding and other objects that come into contact sarcoptic mange lose grazing time and do not gain weight with infected animals can become contaminated with mites as rapidly as do uninfected cattle. and can spread infection. Infestations are generally more common when cattle are housed for the winter and spread more slowly during summer months when cattle are on Life cycle of Sarcoptes scabiei pasture. The entire life cycle of this microscopic mite (see Figure 1) occurs on the cow and takes 14 to 21 days to complete: Does this mite only affect cattle? • The newly-mated female uses its teeth (called There are several varieties of Sarcoptes scabiei. Each variety chelicerae) to form tunnels in which the life cycle is generally occurs on a different host animal and is given a completed. During her life span, she will burrow up to special name. For example, the cattle form is called 2 to 3 centimeters. Sarcoptes scabiei var. bovis, while the swine form is called • A female lays 3 or 4 eggs each day, producing 40 to Sarcoptes scabiei var. suis. 50 eggs during her lifetime. • Eggs hatch in four or five days, releasing larvae that will Sarcoptic mites are generally host-specific. -

Allergic Reaction
ARIZONA COOPERATIVE E TENSION AZ1396 Revised 03/12 There’s Something Bugging Me—Or Is There? Kelly Murray Young Symptoms ¡ Mosquitoes, bedbugs and kissing bugs feed on human blood, but do not live in or on human bodies. Kissing Common symptoms include itching, redness and bumps bugs and bedbugs feed while the person sleeps, leaving on the skin. It feels as if your body has been invaded by spots of blood on the bedding in the morning. To prevent “bugs” crawling under your skin, burrowing into you and mosquitoes and kissing bugs from getting into the house, gnawing and biting. Nothing seems to help, including install screens on all windows. Bedbugs are a growing scratching, digging or using lotions and creams. problem in Arizona. The insects are large enough to be The tiny “bugs” may appear to jump long distances or seen without magnification. Scout around near the bed change colors. and look for rust colored insects, or their droppings, You feel certain that your house and furniture are infested along the mattress seams, between the mattress and box too. Sometimes they come out of linens, tobacco, stored spring and behind the headboard. food or cleaning products. The “bugs” may even seem to ¡ NOTE: Do not apply pesticides to your body, your follow you from place to place. No one has been able to clothing, or your property unless an insect pest has see them but you. You’ve tried having your home treated been positively identified. If an insect pest has been by professional pest control, perhaps even fumigated. -
Sarcoptes Also Called: • Scabies • Sarcoptic Mange • Sarcoptic
Sarcoptes Also called: • Scabies • Sarcoptic mange • Sarcoptic acariasis What is Sarcoptes? Sarcoptes is a microscopic mite that burrows in the outer layer of the skin of dogs. In doing so, it causes tremendous irritation: sarcoptic mange is one of the itchiest conditions in dogs. Although it can affect any area of the skin, the itching is often most severe on the dog’s abdomen, chest, legs, and ears. Where does the mite come from? The mites can be transmitted when a dog is in contact with another infected pet dog or other member of the canine family (such as a fox). Although the mites spend their entire lives on the dog, some mites do fall off into the environment when the dog scratches. These mites can survive in the environment for up to 3 weeks in the right climate, and provide a source of infection for other dogs. Also, because some dogs can harbor (and transmit) the mite without showing signs of skin disease, all the dogs in the home of an infected dog have the potential to be infected and to require treatment. Can the mite infect humans? Yes. The mites prefer to live on dogs, but can also live for at least 6 days on humans. They cause an itchy, uncomfortable skin condition. If you are exhibiting any unusual symptoms, please see your physician or dermatologist. How is it diagnosed? The mite infestation is usually diagnosed by a skin scraping, which is a simple in- clinic procedure performed by a veterinarian. Since the mites can be very difficult to find, we sometimes make the diagnosis based on the signs exhibited by the dog and their subsequent response to treatment. -

Cattle Scabies
292 Cattle Scabies IRWIN H.ROBERTS AND N. G. COBBETT SCABIES is a contagious skin disease laying eggs. The entire cycle takes no caused by minute parasitic organisms more than 12 days. known as mites. It affects cattle of all Psoroptic mites attack the hairy parts ages and breeds. Sometimes it is of the body. They generally begin an referred to as scab, mange, or barn infestation over the withers, but some- itch. Similar infections attack other times also over the back or around the classes of livestock, wild animals, and tailhead. The mites prick the skin to birds, as well as people. obtain food. Tissue fluids ooze from Scabies, the medical term for which the wounds. After many mites have is acariasis, is common throughout the fed, the fluids dry, become mixed with world. It generally causes a severe in- tissue debris, and form scabs. flammation of the skin and itching. The lesions made by the mites spread Mites are related to ticks, spiders, as the parasites increase in number and scorpions, and are not true in- and involve large areas of the back and sects. Unlike insects, adult mites have sides. The condidon may advance over 4 pairs of legs instead of 3. They are practically the entire body if it is not wingless and usually are so small that checked. As the disease worsens, hair they can barely be seen with the naked falls out, and the body is covered with eye. thick, rough crusts. The skin becomes Of the thousands of known kinds of hard and thickened and it takes on mites, four are commonly parasitic to a corrugated look. -
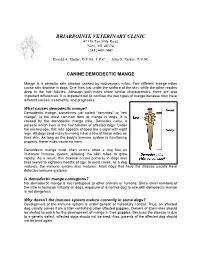
Canine Demodectic Mange
BRIARPOINTE VETERINARY CLINIC 47330 Ten Mile Road Novi, MI 48374 (248) 449-7447 Ronald A. Studer, D.V.M., L.P.C. John S. Parker, D.V.M. CANINE DEMODECTIC MANGE Mange is a parasitic skin disease caused by microscopic mites. Two different mange mites cause skin disease in dogs. One lives just under the surface of the skin, while the other resides deep in the hair follicles. Although both mites share similar characteristics, there are also important differences. It is important not to confuse the two types of mange because they have different causes, treatments, and prognoses. What causes demodectic mange? Demodectic mange, sometimes just called "demodex" or “red mange”, is the most common form of mange in dogs. It is caused by the demodectic mange mite, Demodex canis, a parasite which lives in the hair follicles of affected dogs. Under the microscope, this mite appears shaped like a cigar with eight legs. All dogs (and many humans) have a few of these mites on their skin. As long as the body's immune system is functioning properly, these mites cause no harm. Demodectic mange most often occurs when a dog has an immature immune system, allowing the skin mites to grow rapidly. As a result, this disease occurs primarily in dogs less than twelve to eighteen months of age. In most cases, as a dog matures, the immune system also matures. Adult dogs that have the disease usually have defective immune systems. Is demodectic mange contagious? No, demodectic mange is not contagious to other animals or humans. Since small numbers of the mite is found on virtually all dogs, exposure of a normal dog to one with demodectic mange is not dangerous. -

<I>Demodex Musculi</I> in the Skin of Transgenic Mice
REPORTS Demodex musculi in the Skin of Transgenic Mice LORI R. HILL, DVM,1 PAM S. KILLE, LAT,1 DALE A. WEISS, LATG,1 THOMAS M. CRAIG, DVM, PHD,2 AND LEZLEE G. COGHLAN, DVM1 Abstract ͉ Although infestations by a number of Demodex mite species have been described in mice, the occurrence of Demodex musculi infestation was last reported by Hirst in 1917. This communication describes the occurrence of D. musculi infestation in two lines of transgenic mice and their F1-hybrid offspring. We first found the Demodex mite in mouse hair samples collected during efficacy screenings in an ongoing ectoparasite treatment trial for the fur mite Radfordia affinis. An investigation was undertaken to determine the extent of the Demodex infestation within the facility and the original source of the parasite. D. musculi was found in three of the four mouse genotypes present in the index room and in one of these genotypes in two other rooms. The mite was not found in sentinel mice, other strains, or stocks within the facility. The mites were more easily recovered from the immunodeficient B6,CBA-TgN(CD3E)26Cpt transgenic (Tg) and the hybrid double-Tg (B6,CBA-TgN(CD3E)26Cpt x B6,SENCARB- TgN(pk5prad1)7111Sprd)F1 mice than from the B6,SENCARB-TgN(pk5prad1)7111Sprd Tg mouse, which is believed to be immunocompetent despite its thymic abnormalities. Histopathologic examination showed D. musculi superficially in hair follicles but not in the preputial or clitoral gland or in serial sections of the head, eyelids, or ears, the locations favored by other mouse demodicids. -

External Parasites Or Other Conditions Requiring Medical Care
Sarcoptic Mange Mites Demodectic mange is usually confirmed by taking a skin scraping and Mite Basics examining it under a microscope. Microscopic sarcoptic mange mites cause sarcoptic mange, also Treatment and Control known as scabies. Sarcoptic mange can affect dogs of all ages and Your veterinarian will discuss treatment options with you. Treatment of sizes, during any time of the year. Sarcoptic mange mites are highly dogs with localized demodectic mange generally results in favorable contagious to other dogs and may be passed by close contact with outcomes. Generalized demodecosis, however, may be difficult to treat, infested animals, bedding, or grooming tools. and treatment may only control the condition, rather than cure it. Diagnosis, Risks and Consequences — IMPORTANT POINTISm— portant Points Sarcoptic mange mites burrow through the top layer of the dog’s skin and cause intense itching. Clinical signs include generalized hair • Look for fleas, ticks, and coat abnormalities any time you groom your loss, a skin rash, and crusting. Skin infections may develop secondary dog or cat or when you return home from areas that are likely to to the intense irritation. People who come in close contact with an have higher numbers of these parasites. affected dog may develop a skin rash and should see their physician. • Consult your veterinarian if your pet excessively scratches, chews, or Sarcoptic mange is usually confirmed by taking a skin scraping and licks its coat, or persistently shakes its head or scratches its ears. examining it under a microscope. These clinical signs may indicate the presence of external parasites or other conditions requiring medical care.