Navigating Professional Complexities When Counselling in Alcohol and Other Drug Settings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Excesss Karaoke Master by Artist
XS Master by ARTIST Artist Song Title Artist Song Title (hed) Planet Earth Bartender TOOTIMETOOTIMETOOTIM ? & The Mysterians 96 Tears E 10 Years Beautiful UGH! Wasteland 1999 Man United Squad Lift It High (All About 10,000 Maniacs Candy Everybody Wants Belief) More Than This 2 Chainz Bigger Than You (feat. Drake & Quavo) [clean] Trouble Me I'm Different 100 Proof Aged In Soul Somebody's Been Sleeping I'm Different (explicit) 10cc Donna 2 Chainz & Chris Brown Countdown Dreadlock Holiday 2 Chainz & Kendrick Fuckin' Problems I'm Mandy Fly Me Lamar I'm Not In Love 2 Chainz & Pharrell Feds Watching (explicit) Rubber Bullets 2 Chainz feat Drake No Lie (explicit) Things We Do For Love, 2 Chainz feat Kanye West Birthday Song (explicit) The 2 Evisa Oh La La La Wall Street Shuffle 2 Live Crew Do Wah Diddy Diddy 112 Dance With Me Me So Horny It's Over Now We Want Some Pussy Peaches & Cream 2 Pac California Love U Already Know Changes 112 feat Mase Puff Daddy Only You & Notorious B.I.G. Dear Mama 12 Gauge Dunkie Butt I Get Around 12 Stones We Are One Thugz Mansion 1910 Fruitgum Co. Simon Says Until The End Of Time 1975, The Chocolate 2 Pistols & Ray J You Know Me City, The 2 Pistols & T-Pain & Tay She Got It Dizm Girls (clean) 2 Unlimited No Limits If You're Too Shy (Let Me Know) 20 Fingers Short Dick Man If You're Too Shy (Let Me 21 Savage & Offset &Metro Ghostface Killers Know) Boomin & Travis Scott It's Not Living (If It's Not 21st Century Girls 21st Century Girls With You 2am Club Too Fucked Up To Call It's Not Living (If It's Not 2AM Club Not -

I Got My Glasses from Lions’ …And Went on to Be a Success Front to Pg29:Brandmagazine 8/2/10 1:34 AM Page 2 15
Front to pg29:BrandMagazine 8/2/10 1:34 AM Page 1 WWW.LIONSCLUBS.ORG SEPTEMBER 2010 ‘I got my glasses from Lions’ …and Went on to Be a Success Front to pg29:BrandMagazine 8/2/10 1:34 AM Page 2 15 U.S. DOLLARS TEACHES A STUDENT ABOUT LEADERSHIP AND DEVELOPS POSITIVE LIFE SKILLS THROUGH THE LIONS QUEST PROGRAM. Lions Clubs International Foundation mobilizes resources and raises funds to deliver humanitarian programs around the world. 100% of our donations reach their intended goal, and each donation is important to fulfilling our mission. DONATE NOW Front to pg29:BrandMagazine 8/2/10 1:35 AM Page 3 CONTENTS VOL. 93 NO. 2 LIONS CLUBS INTERNATIONAL MAGAZINE FEATURES DEPARTMENTS 14 ‘I Got My Glasses from Lions’ 4 IN THE SPOTLIGHT News Briefs 8 IDEAS THAT ROAR Wheelchairs for Latin America April Snow Showers Date with Dad 12 LIONS ON LOCATION Unique Recycling 20 Fixtures of Fun Tennis Tournament Longtime projects unite communities. COLUMNS 28 October is Service 3 PRESIDENT’S MESSAGE 47 RECRUITING MEMBERS Commitment Month 48 RAISING FUNDS ALSO IN THIS ISSUE 44 NEW DIRECTORS 45 VISIONARY WORK 46 FOUNDATION IMPACT 50 CLUB BRIEFS 52 ANNIVERSARIES/KEY AWARDS 52 CALENDAR 30 GLOBAL SERVICE CAMPAIGNS IN SPOTLIGHT 53 INFORMATION 32 IOWA LIONS ON THE CUTTING EDGE 52 ON THE WEB 34 FREEDOM RIDE 54 THANK YOU 55 DONOR PROFILE 56 LAST ROAR Front to pg29:BrandMagazine 8/2/10 1:35 AM Page 4 STAFF Wing-Kun Tam, Unit 1901-2, 19/F, Far East Finance Editor-in-Chief: Peter Lynch Centre, 16 Harcourt Road, Hong Kong, China; Sec- Managing Editor: Dane La Joye ond Vice President Wayne A. -

Karaoke Book
10 YEARS 3 DOORS DOWN 3OH!3 Beautiful Be Like That Follow Me Down (Duet w. Neon Hitch) Wasteland Behind Those Eyes My First Kiss (Solo w. Ke$ha) 10,000 MANIACS Better Life StarStrukk (Solo & Duet w. Katy Perry) Because The Night Citizen Soldier 3RD STRIKE Candy Everybody Wants Dangerous Game No Light These Are Days Duck & Run Redemption Trouble Me Every Time You Go 3RD TYME OUT 100 PROOF AGED IN SOUL Going Down In Flames Raining In LA Somebody's Been Sleeping Here By Me 3T 10CC Here Without You Anything Donna It's Not My Time Tease Me Dreadlock Holiday Kryptonite Why (w. Michael Jackson) I'm Mandy Fly Me Landing In London (w. Bob Seger) 4 NON BLONDES I'm Not In Love Let Me Be Myself What's Up Rubber Bullets Let Me Go What's Up (Acoustative) Things We Do For Love Life Of My Own 4 PM Wall Street Shuffle Live For Today Sukiyaki 110 DEGREES IN THE SHADE Loser 4 RUNNER Is It Really Me Road I'm On Cain's Blood 112 Smack Ripples Come See Me So I Need You That Was Him Cupid Ticket To Heaven 42ND STREET Dance With Me Train 42nd Street 4HIM It's Over Now When I'm Gone Basics Of Life Only You (w. Puff Daddy, Ma$e, Notorious When You're Young B.I.G.) 3 OF HEARTS For Future Generations Peaches & Cream Arizona Rain Measure Of A Man U Already Know Love Is Enough Sacred Hideaway 12 GAUGE 30 SECONDS TO MARS Where There Is Faith Dunkie Butt Closer To The Edge Who You Are 12 STONES Kill 5 SECONDS OF SUMMER Crash Rescue Me Amnesia Far Away 311 Don't Stop Way I Feel All Mixed Up Easier 1910 FRUITGUM CO. -

University of Oklahoma Graduate College
UNIVERSITY OF OKLAHOMA GRADUATE COLLEGE WOMEN’S SHAME RESILIENCE: EXAMINING VARIOUS THEORETICAL ASSUMPTIONS OF SHAME RESILIENCE THEORY A DISSERTATION SUBMITTED TO THE GRADUATE FACULTY in partial fulfillment of the requirements for the Degree of DOCTOR OF PHILOSOPHY By JENNY M. BENDURE Norman, Oklahoma 2014 WOMEN’S SHAME RESILIENCE: EXAMINING VARIOUS THEORETICAL ASSUMPTIONS OF SHAME RESILIENCE THEORY A DISSERTATION APPROVED FOR THE DEPARTMENT OF EDUCATIONAL PSYCHOLOGY BY ______________________________ Dr. Melissa Frey, Chair ______________________________ Dr. Denise Beesley ______________________________ Dr. Lara Mayeux ______________________________ Dr. Laurette Taylor ______________________________ Dr. T. H. Lee Williams © Copyright by JENNY M. BENDURE 2014 All Rights Reserved. For Sophia Marie May you always know your worth. May you endeavor to challenge the messages that would threaten to tame your wild heart, stifle your bold creativity, and silence your authentic voice. May you never be afraid to fly on your own wings. And when you grow weary from the struggle, may you always know that your father and I are nearby to lighten your load, champion your cause, and celebrate your imperfections. Acknowledgements Behind every successful woman is herself … and along the way there also are those wholehearted souls who, through their generosity, strength of spirit, and authenticity, make the journey more rewarding than the destination. Michael, your devotion and courage are unequivocal. You enthusiastically paved the road, took up the slack, and set aside your own ambitions to support my aspirations. You are my best friend. Sophia, I am amazed by your self-assured nature, kind heart, and sense of humor. You are the coolest person I know. My worries were always for naught. -

Angel in My Heart 09/14 Revise3 P
09/14 revise3 p. 1 of 69 Angel in my Heart 09/14 revise3 p. 2 of 69 ANGEL IN MY HEART a musical romance The set is divided into two parts: one part suggests the men's departments at various expensive New York department stores; the other area represents a copywriter's office at a fragrance company, with ergonomic chair, desk and computer. Other settings are suggested throughout. ACT ONE - Scene i - THE MENʼS DEPARTMENT OF BERGDORF GOODMAN'S. BRIAN HAYES, early 30ʼs and immaculately handsome, is trying on a designer sport jacket when BERNIE LICHTENBERG, same age, enters in a frazzle. BERNIE [recitative: I know Iʼm late…] I KNOW, I KNOW! IʼM LATE, BUT YOU CAN THANK YOUR LUCKY STARS IʼM HERE AT ALL. I BARELY MADE IT THROUGH THE FRAGRANCE DEPARTMENT. WHAT DʼYA CALLIT — the pretty people with the samples ... BRIAN ATTACK MODELS. STINK BOMBERS… BERNIE YEH. THEM. THEYʼRE ON THE RAMPAGE — Iʼve been spritzed by Ralph, Calvin and three Europeans Iʼve never heard of. If I put my wrist too near my nose, Iʼll pass out from the fumes. BRIAN So donʼt sniff your wrist. BERNIE AND ALL THOSE “CHAYAS” PUSHING AND SHOVING, FIGHTING OVER THE CASHMERE SWEATERS. WHO KNEW YOU COULD GET BLACK AND BLUE FROM CASHMERE? I had to threaten a lawsuit to get at the beige crew neck I had my eye on. Youʼd think people would be more civilized at Bergdorfʼs. BRIAN SOMETIMES YOUʼVE GOTTA BE AGGRESSIVE AND GO AFTER WHAT YOU WANT. THATʼS THE EXCITEMENT OF SHOPPING: THE THRILL OF THE HUNT. -

Jesus Is Love Ruthie Kim, Reality San Francisco
Sermon Transcript from October, 2nd 2016 Jesus Is Love Ruthie Kim, Reality San Francisco Today, I'm going to be talking about Jesus' love and I know sometimes, especially if you've grown up in the church, you hear that and it's kind of like, "Oh. Yeah." But, I feel like this morning, God has a new perspective, a new angle for us. So, we're going to read the Scripture and then we're going to pray and just invite the Holy Spirit to come and give us fresh ears this morning. So, John 8:2: "At dawn he [Jesus] appeared again in the temple courts, where all the people gathered around him, and he sat down to teach them. The teachers of the law and the Pharisees brought in a woman caught in adultery. They made her stand before the group and said to Jesus, 'Teacher, this woman was caught in the act of adultery. In the Law Moses commanded us to stone such women. Now what do you say?' They were asking him this question as a trap, in order to have a basis for accusing him. "But Jesus bent down and started to write on the ground with his finger. When they kept on questioning him, he straightened up and said to them, 'Let any one of you who is without sin be the first to throw a stone at her.' Again he stooped down and wrote on the ground. "At this, those who heard began to go away one at a time, the older ones first, until only Jesus was left, with the woman still standing there. -
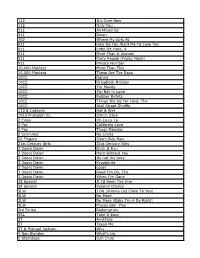
112 It's Over Now 112 Only You 311 All Mixed up 311 Down
112 It's Over Now 112 Only You 311 All Mixed Up 311 Down 702 Where My Girls At 911 How Do You Want Me To Love You 911 Little Bit More, A 911 More Than A Woman 911 Party People (Friday Night) 911 Private Number 10,000 Maniacs More Than This 10,000 Maniacs These Are The Days 10CC Donna 10CC Dreadlock Holiday 10CC I'm Mandy 10CC I'm Not In Love 10CC Rubber Bullets 10CC Things We Do For Love, The 10CC Wall Street Shuffle 112 & Ludacris Hot & Wet 1910 Fruitgum Co. Simon Says 2 Evisa Oh La La La 2 Pac California Love 2 Pac Thugz Mansion 2 Unlimited No Limits 20 Fingers Short Dick Man 21st Century Girls 21st Century Girls 3 Doors Down Duck & Run 3 Doors Down Here Without You 3 Doors Down Its not my time 3 Doors Down Kryptonite 3 Doors Down Loser 3 Doors Down Road I'm On, The 3 Doors Down When I'm Gone 38 Special If I'd Been The One 38 Special Second Chance 3LW I Do (Wanna Get Close To You) 3LW No More 3LW No More (Baby I'm A Do Right) 3LW Playas Gon' Play 3rd Strike Redemption 3SL Take It Easy 3T Anything 3T Tease Me 3T & Michael Jackson Why 4 Non Blondes What's Up 5 Stairsteps Ooh Child 50 Cent Disco Inferno 50 Cent If I Can't 50 Cent In Da Club 50 Cent In Da Club 50 Cent P.I.M.P. (Radio Version) 50 Cent Wanksta 50 Cent & Eminem Patiently Waiting 50 Cent & Nate Dogg 21 Questions 5th Dimension Aquarius_Let the sunshine inB 5th Dimension One less Bell to answer 5th Dimension Stoned Soul Picnic 5th Dimension Up Up & Away 5th Dimension Wedding Blue Bells 5th Dimension, The Last Night I Didn't Get To Sleep At All 69 Boys Tootsie Roll 8 Stops 7 Question -

Songs by Artist
Sound Master Entertianment Songs by Artist smedenver.com Title Title Title .38 Special 2Pac 4 Him Caught Up In You California Love (Original Version) For Future Generations Hold On Loosely Changes 4 Non Blondes If I'd Been The One Dear Mama What's Up Rockin' Onto The Night Thugz Mansion 4 P.M. Second Chance Until The End Of Time Lay Down Your Love Wild Eyed Southern Boys 2Pac & Eminem Sukiyaki 10 Years One Day At A Time 4 Runner Beautiful 2Pac & Notorious B.I.G. Cain's Blood Through The Iris Runnin' Ripples 100 Proof Aged In Soul 3 Doors Down That Was Him (This Is Now) Somebody's Been Sleeping Away From The Sun 4 Seasons 10000 Maniacs Be Like That Rag Doll Because The Night Citizen Soldier 42nd Street Candy Everybody Wants Duck & Run 42nd Street More Than This Here Without You Lullaby Of Broadway These Are Days It's Not My Time We're In The Money Trouble Me Kryptonite 5 Stairsteps 10CC Landing In London Ooh Child Let Me Be Myself I'm Not In Love 50 Cent We Do For Love Let Me Go 21 Questions 112 Loser Disco Inferno Come See Me Road I'm On When I'm Gone In Da Club Dance With Me P.I.M.P. It's Over Now When You're Young 3 Of Hearts Wanksta Only You What Up Gangsta Arizona Rain Peaches & Cream Window Shopper Love Is Enough Right Here For You 50 Cent & Eminem 112 & Ludacris 30 Seconds To Mars Patiently Waiting Kill Hot & Wet 50 Cent & Nate Dogg 112 & Super Cat 311 21 Questions All Mixed Up Na Na Na 50 Cent & Olivia 12 Gauge Amber Beyond The Grey Sky Best Friend Dunkie Butt 5th Dimension 12 Stones Creatures (For A While) Down Aquarius (Let The Sun Shine In) Far Away First Straw AquariusLet The Sun Shine In 1910 Fruitgum Co. -

Songs by Artist
Songs by Artist Title Title (Hed) Planet Earth 2 Live Crew Bartender We Want Some Pussy Blackout 2 Pistols Other Side She Got It +44 You Know Me When Your Heart Stops Beating 20 Fingers 10 Years Short Dick Man Beautiful 21 Demands Through The Iris Give Me A Minute Wasteland 3 Doors Down 10,000 Maniacs Away From The Sun Because The Night Be Like That Candy Everybody Wants Behind Those Eyes More Than This Better Life, The These Are The Days Citizen Soldier Trouble Me Duck & Run 100 Proof Aged In Soul Every Time You Go Somebody's Been Sleeping Here By Me 10CC Here Without You I'm Not In Love It's Not My Time Things We Do For Love, The Kryptonite 112 Landing In London Come See Me Let Me Be Myself Cupid Let Me Go Dance With Me Live For Today Hot & Wet Loser It's Over Now Road I'm On, The Na Na Na So I Need You Peaches & Cream Train Right Here For You When I'm Gone U Already Know When You're Young 12 Gauge 3 Of Hearts Dunkie Butt Arizona Rain 12 Stones Love Is Enough Far Away 30 Seconds To Mars Way I Fell, The Closer To The Edge We Are One Kill, The 1910 Fruitgum Co. Kings And Queens 1, 2, 3 Red Light This Is War Simon Says Up In The Air (Explicit) 2 Chainz Yesterday Birthday Song (Explicit) 311 I'm Different (Explicit) All Mixed Up Spend It Amber 2 Live Crew Beyond The Grey Sky Doo Wah Diddy Creatures (For A While) Me So Horny Don't Tread On Me Song List Generator® Printed 5/12/2021 Page 1 of 334 Licensed to Chris Avis Songs by Artist Title Title 311 4Him First Straw Sacred Hideaway Hey You Where There Is Faith I'll Be Here Awhile Who You Are Love Song 5 Stairsteps, The You Wouldn't Believe O-O-H Child 38 Special 50 Cent Back Where You Belong 21 Questions Caught Up In You Baby By Me Hold On Loosely Best Friend If I'd Been The One Candy Shop Rockin' Into The Night Disco Inferno Second Chance Hustler's Ambition Teacher, Teacher If I Can't Wild-Eyed Southern Boys In Da Club 3LW Just A Lil' Bit I Do (Wanna Get Close To You) Outlaw No More (Baby I'ma Do Right) Outta Control Playas Gon' Play Outta Control (Remix Version) 3OH!3 P.I.M.P. -
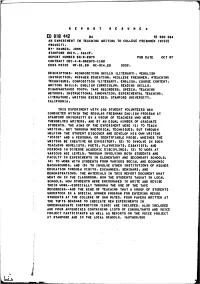
An Experiment in Teaching Writing to College Freshmen (Voice Project)
REPORT RESUMES ED 018 112 24 TE 500 064 AN EXPERIMENT IN TEACHING WRITING TO COLLEGE FRESHMEN (VOICE PROJECT). BY- HAWKES, JOHN STANFORD UNIV., CALIF. REPORT NUMBER BR -6 -2075 PUB DATE OCT 67 CONTRACT OEC-4-6062075-1160 EDRS PRICE MF -$1.50 HC- $14.20 353P. DESCRIPTORS-. *COMPOSITION SKILLS (LITERARY), *ENGLISH INSTRUCTION, *HIGHER EDUCATION, *COLLEGE FRESHMEN, *TEACHING TECHNIQUES, COMPOSITION (LITERARY), ENGLISH, COURSE CONTENT, WRITING SKILLS, ENGLISH CURRICULUM, READING SKILLS, DISADVANTAGED YOUTH, TAPE RECORDERS, SPEECH, TEACHING METHODS, INSTRUCTIONAL INNOVATION, EXPERIMENTAL TEACHING, LITERATURE, WRITING EXERCISES, STANFORD UNIVERSITY, CALIFORNIA, THIS EXPERIMENT WITH 100 STUDENT VOLUNTEERS WAS CONDUCTED WITHIN THE REGULAR FRESHMAN ENGLISH PROGRAM AT STANFORD UNIVERSITY BY A GROUP OF TEACHERS WHO WERE THEMSELVES WRITERS, AND BY AN EQUAL NUMBER OF GRADUATE STUDENTS. THE AIMS OF THE EXPERIMENT WERE (1) TO TEACH WRITING, NOT THROUGH RHETORICAL TECHNIQUES, BUT THROUGH HELPING THE STUDENT DISCOVER AND DEVELOP HIS OWN WRITING "VOICE" AND A PERSONAL OR IDENTIFIABLE PROSE, WHETHER THE WRITING BE CREATIVE OR EXPOSITORY, (2) TO INVOLVE IN SUCH TEACHING NOVELISTS, POETS, PLAYWRIGHTS, ESSAYISTS, AND PERSONS IN DIVERSE ACADEMIC DISCIPLINES, (3) TO WORK AT VARIOUS AGE LEVELS, THROUGH INVOLVING BOTH STUDENTS AND FACULTY IN EXPERIMENTS IN ELEMENTARY AND SECONDARY SCHOOLS, (4) TO WORK WITH STUDENTS FROM VARIOUS SOCIAL AND ECONOMIC BACKGROUNDS, AND (5) TO INVOLVE OTHER INSTITUTIONS OF HIGHER EDUCATION THROUGH VISITS, EXCHANGES, SEMINARS, AND DEMONSTRATIONS. THE MATERIALS IN THIS REPORT DOCUMENT WHAT WENT ON IN THE CLASSROOM, HOW THE STUDENTS TAUGHT IN LOCAL SCHOOLS, HOW STUDENTS WERE ENCOURAGED TO WRITE AND REVISE THEIR WORK -- ESPECIALLY THROUGH THE USE OF THE TAPE RECORDERS- -AND THE KIND OF TEACHING THAT A GROUP OF STUDENTS UNDERTOOK IN A SPECIAL SUMMER PROGRAM FOR ENTERING NEGRO STUDENTS AT THE COLLEGE OF SAN MATEO. -

Steve's Karaoke Songbook
Steve's Karaoke Songbook Artist Song Title Artist Song Title +44 WHEN YOUR HEART STOPS INVISIBLE MAN BEATING WAY YOU WANT ME TO, THE 10 YEARS WASTELAND A*TEENS BOUNCING OFF THE CEILING 10,000 MANIACS CANDY EVERYBODY WANTS A1 CAUGHT IN THE MIDDLE MORE THAN THIS AALIYAH ONE I GAVE MY HEART TO, THE THESE ARE THE DAYS TRY AGAIN TROUBLE ME ABBA DANCING QUEEN 10CC THINGS WE DO FOR LOVE, THE FERNANDO 112 PEACHES & CREAM GIMME GIMME GIMME 2 LIVE CREW DO WAH DIDDY DIDDY I DO I DO I DO I DO I DO ME SO HORNY I HAVE A DREAM WE WANT SOME PUSSY KNOWING ME, KNOWING YOU 2 PAC UNTIL THE END OF TIME LAY ALL YOUR LOVE ON ME 2 PAC & EMINEM ONE DAY AT A TIME MAMMA MIA 2 PAC & ERIC WILLIAMS DO FOR LOVE SOS 21 DEMANDS GIVE ME A MINUTE SUPER TROUPER 3 DOORS DOWN BEHIND THOSE EYES TAKE A CHANCE ON ME HERE WITHOUT YOU THANK YOU FOR THE MUSIC KRYPTONITE WATERLOO LIVE FOR TODAY ABBOTT, GREGORY SHAKE YOU DOWN LOSER ABC POISON ARROW ROAD I'M ON, THE ABDUL, PAULA BLOWING KISSES IN THE WIND WHEN I'M GONE COLD HEARTED 311 ALL MIXED UP FOREVER YOUR GIRL DON'T TREAD ON ME KNOCKED OUT DOWN NEXT TO YOU LOVE SONG OPPOSITES ATTRACT 38 SPECIAL CAUGHT UP IN YOU RUSH RUSH HOLD ON LOOSELY STATE OF ATTRACTION ROCKIN' INTO THE NIGHT STRAIGHT UP SECOND CHANCE WAY THAT YOU LOVE ME, THE TEACHER, TEACHER (IT'S JUST) WILD-EYED SOUTHERN BOYS AC/DC BACK IN BLACK 3T TEASE ME BIG BALLS 4 NON BLONDES WHAT'S UP DIRTY DEEDS DONE DIRT CHEAP 50 CENT AMUSEMENT PARK FOR THOSE ABOUT TO ROCK (WE SALUTE YOU) CANDY SHOP GIRLS GOT RHYTHM DISCO INFERNO HAVE A DRINK ON ME I GET MONEY HELLS BELLS IN DA -

Modern but Not Meaningless: Nonreligious Cultures and Communities in the United States
Modern but Not Meaningless: Nonreligious Cultures and Communities in the United States A Dissertation SUBMITTED TO THE FACULTY OF UNIVERSITY OF MINNESOTA BY Jacqueline Frost IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY Penny Edgell, Advisor June 2020 Modern but Not Meaningless: Nonreligious Cultures and Communities in the United States © 2020 by Jacqueline Frost All rights reserved Acknowledgements This dissertation is the product of support and feedback from numerous mentors, colleagues, friends, family members, and community members. First, I would like to thank the nonreligious people who participated in my project, especially the members of the Minneapolis/St. Paul chapter of the Sunday Assembly. Without their willingness to welcome me into their community, share their stories with me, and provide continuous feedback on my research questions, this project would not have been possible. I am forever grateful to everyone who took time out of their day to sit with me for interviews, who shared their nonreligious narratives with me, and who allowed me to document the often difficult, vulnerable, and emotional process of building community and ritual. Their kindness and openness allowed me to shed new light on the increasingly diverse population of atheists, agnostics, and “nothing in particulars” that make up the growing nonreligious demographic in the United States. I hope this dissertation adequately conveys the passion and dedication with which so many nonreligious people are working to improve their communities and create meaning in our complex world. This dissertation would also not have been possible without my advisor, Penny Edgell. Words cannot fully express what Penny’s mentorship has meant to me and the thousands of ways, both big and small, that her support and guidance have made me a better scholar, teacher, and writer.