Governance in Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MDG Report 2010 WINNING the NUMBERS, LOSING the WAR the Other MDG Report 2010
Winning the Numbers, Losing the War: The Other MDG Report 2010 WINNING THE NUMBERS, LOSING THE WAR The Other MDG Report 2010 Copyright © 2010 SOCIAL WATCH PHILIPPINES and UNITED NATIONS DEVELOPMENT PROGRAMME (UNDP) All rights reserved Social Watch Philippines and the United Nations Development Programme (UNDP) encourage the use, translation, adaptation and copying of this material for non-commercial use, with appropriate credit given to Social Watch and UNDP. Inquiries should be addressed to: Social Watch Philippines Room 140, Alumni Center, University of the Philippines, Diliman, Quezon City, PHILIPPINES 1101 Telefax: +63 02 4366054 Email address: [email protected] Website: http://www.socialwatchphilippines.org The views expressed in this book are those of the authors’ and do not necessarily refl ect the views and policies of the United Nations Development Programme (UNDP). Editorial Board: LEONOR MAGTOLIS BRIONES ISAGANI SERRANO JESSICA CANTOS MARIVIC RAQUIZA RENE RAYA Editorial Team: Editor : ISAGANI SERRANO Copy Editor : SHARON TAYLOR Coordinator : JANET CARANDANG Editorial Assistant : ROJA SALVADOR RESSURECCION BENOZA ERICSON MALONZO Book Design: Cover Design : LEONARD REYES Layout : NANIE GONZALES Photos contributed by: Isagani Serrano, Global Call To Action Against Poverty – Philippines, Medical Action Group, Kaakbay, Alain Pascua, Joe Galvez, Micheal John David, May-I Fabros ACKNOWLEDGEMENT any deserve our thanks for the production of this shadow report. Indeed there are so many of them that Mour attempt to make a list runs the risk of missing names. Social Watch Philippines is particularly grateful to the United Nations Millennium Campaign (UNMC), the United Nations Development Programme (UNDP), the Millennium Development Goals Achievement Fund (MDG-F) and the HD2010 Platform for supporting this project with useful advice and funding. -

DOH Presents Agenda for Health Care Financing
Vol. XVII No. 4 July - August 1999 ISSN 0115-9097 DOH presents agenda for health care financing ajor changes in health and local --- spent P34.1 billion or 38.6 the inequities obtaining in the health care financing policies percent while the National Health In- system. “Only those who can afford to are being pursued and surance Program (NHIP) which re- pay are able to support such a system,” Mshall be implemented as placed the Medicare Program spent he said. part of the Department of Health’s P6.4 billion or 7.1 percent. The rest of (DOH) overall effort to reform the the total health expenditure – P7 bil- Second, financing for public health health sector. lion or 8 percent -- came from various programs is subject to the uncertainties of other sources. the annual budget process. Secretary In a roundtable discussion spon- Romualdez pointed out that national sored recently by the DOH and the Based on these figures, one can = 2 Philippine Institute for Development glean some of the problems associated Studies (PIDS), Health Secretary with the manner by which health care Alberto Romualdez expounded on funds are generated. First, the bulk of EDITOR'S NOTES these reforms in his presentation en- the financial burden is on individual fami- titled “An Agenda in Health Care Fi- lies. As Romualdez noted, this leads to For the past couple of years, health nancing for the 21st Century.” Said care financing has been one of the major agenda is being presented to various topics for research and advocacy being sectors for feedback and further refine- WHAT'S INSIDE jointly addressed by the Department of ments. -

TAMBULI APRIL 2006 Issue 2Nd EDIT
Senator Ralph Recto as Chairperson of the Senate Committee on Ways and Means with Senator Juan Ponce Enrile, held recently a public hearing on the proposed Fiscal Incentives Bill and the Anti- Smuggling Bill, which FPI has been vigorously supporting. FPI on Anti-Smuggling and Fiscal Incentives Bills he Federation of Philippine Industries (FPI) presented its T recommendations to the Senate Ways and Means Committee for possible incorporation on the proposed Anti-Smuggling and Fiscal Incentives Bills. Senator Ralph Recto, with Senators Juan Ponce Enrile and Juan Flavier as members tackling the two essential bills, chairs the Senate Committee on Ways and Means during a well-attended public hearing held recently at the Philippine Senate. FPI Recommendations on the Anti-Smuggling Bill: FPI, through its President, Mr. Jesus L. Arranza, recommended the following for possible incorporation on the proposed Anti- FPI President Jesus L. Arranza joined the round table discussions Smuggling Bill: with President Gloria Macapagal-Arroyo on various issues of • All Inward Foreign Manifests (IFMs) should be published in national concerns, which was aired, live via NBN Channel 4. the Bureau of Customs and/or in the Department of Trade and Industry’s web sites. President Gloria Macapagal- FPI Legal Team to assist BOC • All Import Declarations should follow the Harmonized System Arroyo approved in principle the of 8-digit heading to prevent misclassification. issuance of an Executive Order, President Gloria Macapagal-Arroyo • Every classification by Tariff Heading should have value range requiring all government welcomed the assistance of the and date, which should be published in the BOC and/or DTI agencies and government Federation of Philippine Industries websites and periodically updated. -

(HSRA) Implementation Progress
January 2003 A Review of the Health Sector Reform Agenda (HSRA) Implementation Progress Orville Solon, Carlo Panelo, and Edwin Gumafelix This study was funded by the U.S. Agency for International Development (USAID) under the terms of Contract No. HRN-I-00-98-00033-00 Delivery Order No. 804. The opinions expressed herein are those of the authors and do not necessarily reflect the views of USAID. Contents Contents…………………………………………………………………………………. i Tables……………………………………………………………………………………. ii Box………………………………………………………………………………………. iii Acronyms………………………………………………………………………………... iv Acknowledgments……………………………………………………………………….. vi Overview………………………………………………………………………………... 1 Section 1 HSRA and Its Implementation Strategy……………………………………………… 3 Section 2 Progress in Convergence Site Development………………………………………….. 7 Section 3 Progress in Off-site Reforms…………………………………………………………... 13 1. DOH Hospitals…………………………………………………………………… 13 2. Public Health Programs………………………………………………………….. 16 3. Health Regulation………………………………………………………………... 19 4. National Health Insurance Program ……………………………………………... 21 Section 4 Progress in Crosscutting Reform Activities…………………………………………... 25 Section 5 Summary of the Progress of HSRA Implementation………………………………... 29 Section 6 Recommendations for Future Implementation of Activities………………………… 35 Annex A Summary of HSRA Implementation Progress in the Eight Primary Convergence Sites……………………………………………………………………………………… 39 A Review of the HSRA Implementation Progress i Tables Table 1. Number of convergence sites, by targets and accomplishments……………. 7 Table 2. Desired outcomes and critical activities, by specific concerns, in convergence sites…………………………………………………………… 9 Table 3. Best practices in convergence site development……………………………. 12 Table 4. Accomplishments in DOH hospital reforms………………………………... 14 Table 5. Target and actual number of public health facilities for critical upgrading… 15 Table 6a. DOH budget allocation by type of service (in billion pesos), 1999-2003…. 16 Table 6b. DOH budget share (in per cent), by type of service, 1999-2003…………... 16 Table 7. -

Philippinen: Wahlen in Turbulenter Zeit
Willibold Frehner Philippinen: Wahlen in turbulenter Zeit Am 14. Mai 2001 wurden in den Philippinen Wahlen Die Filipinos haben im Januar 2001 ihren unfähigen durchgeführt, die auch als und korrupten Präsidenten Joseph Estrada aus dem Referendum für oder gegen Amt gejagt. Die neue Variante der People’s Power hat die neue Regierung von den auf sechs Jahre gewählten Präsidenten bereits Präsidentin Arroyo angese- hen wurden. Kandidaten für nach 31 Monaten chaotischer Regierung gezwungen, den Kongress, aber auch den Präsidentenpalast zu verlassen. Gegen den frühe- Gouverneure und Bürger- ren Präsidenten Estrada, gegen eine Reihe seiner Ge- meister wurden gewählt. Mitten im Wahlkampf wur- folgsleute und gegen Begünstigte wurden Anklagen de der frühere Präsident wegen Korruption und Veruntreuung vorbereitet. Estrada verhaftet und es Estrada und sein Sohn Jinggoy wurden verhaftet und kam zu massiven Auseinan- in ein eigens für diese beiden Häftlinge eingerichtetes dersetzungen zwischen Poli- zei, Militär und Demonst- Spezialgefängnis gebracht. ranten. Die Emotionen Die neue Präsidentin Gloria Macapagal-Arroyo schlugen hoch und hundert hat von ihrem Vorgänger ein schweres Erbe über- Tote waren zu beklagen. Die nommen. Insbesondere im wirtschaftlichen und im Wahlen unterstrichen, dass das Land derzeit in zwei politischen Bereich zeigen sich gravierende Pro- Lager gespalten ist. Eine bleme, die sich nicht kurzfristig lösen lassen. Mehrheit der Bevölkerung Am 14. Mai 2001 wurden in den Philippinen unterstützt die Regierung, Wahlen durchgeführt, die auch als Referendum für aber eine – wenn auch be- trächtliche – Minderheit oder gegen die neue Regierung der Präsidentin Ar- votierte für das Lager des royo angesehen wurden. Kandidaten für den Senat gestürzten Estrada. Mit den und den Kongress, aber auch Gouverneure und Bür- Wahlergebnissen kann die Regierung politisch überle- germeister wurden gewählt. -
![THE HUMBLE BEGINNINGS of the INQUIRER LIFESTYLE SERIES: FITNESS FASHION with SAMSUNG July 9, 2014 FASHION SHOW]](https://docslib.b-cdn.net/cover/7828/the-humble-beginnings-of-the-inquirer-lifestyle-series-fitness-fashion-with-samsung-july-9-2014-fashion-show-667828.webp)
THE HUMBLE BEGINNINGS of the INQUIRER LIFESTYLE SERIES: FITNESS FASHION with SAMSUNG July 9, 2014 FASHION SHOW]
1 The Humble Beginnings of “Inquirer Lifestyle Series: Fitness and Fashion with Samsung Show” Contents Presidents of the Republic of the Philippines ................................................................ 8 Vice-Presidents of the Republic of the Philippines ....................................................... 9 Popes .................................................................................................................................. 9 Board Members .............................................................................................................. 15 Inquirer Fitness and Fashion Board ........................................................................... 15 July 1, 2013 - present ............................................................................................... 15 Philippine Daily Inquirer Executives .......................................................................... 16 Fitness.Fashion Show Project Directors ..................................................................... 16 Metro Manila Council................................................................................................. 16 June 30, 2010 to June 30, 2016 .............................................................................. 16 June 30, 2013 to present ........................................................................................ 17 Days to Remember (January 1, AD 1 to June 30, 2013) ........................................... 17 The Philippines under Spain ...................................................................................... -

Papal Visit Philippines 2014 and 2015 2014
This event is dedicated to the Filipino People on the occasion of the five- day pastoral and state visit of Pope Francis here in the Philippines on October 23 to 27, 2014 part of 22- day Asian and Oceanian tour from October 22 to November 13, 2014. Papal Visit Philippines 2014 and 2015 ―Mercy and Compassion‖ a Papal Visit Philippines 2014 and 2015 2014 Contents About the project ............................................................................................... 2 About the Theme of the Apostolic Visit: ‗Mercy and Compassion‘.................................. 4 History of Jesus is Lord Church Worldwide.............................................................................. 6 Executive Branch of the Philippines ....................................................................... 15 Presidents of the Republic of the Philippines ....................................................................... 15 Vice Presidents of the Republic of the Philippines .............................................................. 16 Speaker of the House of Representatives of the Philippines ............................................ 16 Presidents of the Senate of the Philippines .......................................................................... 17 Chief Justice of the Supreme Court of the Philippines ...................................................... 17 Leaders of the Roman Catholic Church ................................................................ 18 Pope (Roman Catholic Bishop of Rome and Worldwide Leader of Roman -

Aligning Healthcare Facilities with KP
www.doh.gov.ph what’s inside Polio Endgame Conference of the EDITORIAL: We’re Message Parties 6 almost there from the Health Secretary p2 p3 p4 p8 VOL. 1 ISSUE 6 OCTOBER 2014 Statement of Acting Health Secretary Janette Aligning healthcare facilities Loreto Garin in the Passing of Secretary Juan with KP Martin Flavier For 2014, HFEP allocates PhP 13.5 B for construction, upgrading of 448 hospitals, QUALITY HEALTHCARE FACILITIES FOR FILIPINOS The development of quality healthcare 1,028 RHU’s facilities, through the Health Facilities Enhancement Program (HFEP), is a vital step in achieving Kalusugan Pangkalahatan. With Health Secretary Enrique Ona at the helm, a more improved quality and 1,365 of life especially in healthcare, is on its way for every Filipinos We are no longer the once BHSs nation- Moreover, these facilities are under 761 LGU PhilHealth enrolment, there are needs to have super-provider of health services. hospitals and other health facilities and 70 DOH health facilities that can respond to their health We are now a servicer of servicers. wide hospitals, 3,395 rural health units (RHUs), and 2,685 care needs at all levels of care,” Sec. Ona said. -Sec. Juan M. Flavier By Gelyka Ruth R. Dumaraos barangay health stations (BHSs). “Through modernization of DOH hospitals in the HFEP for this year funded an amount of PhP 13.5 regions outside NCR, congestion of DOH specialized Dr. Juan Martin Flavier was among THE ACHIEVEMENT of Kalusugan Pangkalahatan billion for the upgrading, rehabilitation, expansion, hospitals in Metro Manila will be reduced,” he added. -

No Pain, No Gain Juan M
26 World Heolth • 48th Year, No. 1, January-February 1995 No pain, no gain Juan M. Flavier aria, a chubby nation, or in the form of and carefree streamers and snacks for Mtwo-year-old, volunteers, and funds for was eagerly awaiting her syringes and vaccines. turn for her patak, her The most important two drops of oral polio support came from the vaccine. She could still frontline health workers. remember how peculiar The vaccinations took the taste was. This is place where people going to be her fourth would usually congre patak. Her Aunt Loleng gate- in schools, was affected by this dis churches, train and bus ease and she goes around stations, airports, piers, with a heavy limp. The waiting-rooms, day-care Or Juan Flavier (second from the left) plays his part in the polio vaccination thought of last month's campaign. centres, shopping malls, scene when some popular restaurants, mu children cried after getting their but today she was trying to be an nicipal and city halls and the houses measles injections made Maria example. "Come on, mother. of vi ll age captains or councillors. somewhat apprehensive. She could Remember, it's just like an ant's bite. One local city mayor even waylaid remember her mother's encourage Remember, no pain, no gain," Maria all incoming provincial buses in ment: "Come on, children. It's all and Clara both said with a laugh. order to persuade the travellers to be right. It 's just like an ant's bite. It's immunized. nothing really. Remember, no pain, The response was overwhelming. -

20 Century Ends
New Year‟s Celebration 2013 20th CENTURY ENDS ANKIND yesterday stood on the threshold of a new millennium, linked by satellite technology for the most closely watched midnight in history. M The millennium watch was kept all over the world, from a sprinkle of South Pacific islands to the skyscrapers of the Americas, across the pyramids, the Parthenon and the temples of Angkor Wat. Manila Archbishop Luis Antonio Cardinal Tagle said Filipinos should greet 2013 with ''great joy'' and ''anticipation.'' ''The year 2013 is not about Y2K, the end of the world or the biggest party of a lifetime,'' he said. ''It is about J2K13, Jesus 2013, the Jubilee 2013 and Joy to the World 2013. It is about 2013 years of Christ's loving presence in the world.'' The world celebration was tempered, however, by unease over Earth's vulnerability to terrorism and its dependence on computer technology. The excitement was typified by the Pacific archipelago nation of Kiribati, so eager to be first to see the millennium that it actually shifted its portion of the international dateline two hours east. The caution was exemplified by Seattle, which canceled its New Year's party for fear of terrorism. In the Philippines, President Benigno Aquino III is bracing for a “tough” new year. At the same time, he called on Filipinos to pray for global peace and brotherhood and to work as one in facing the challenges of the 21st century. Mr. Estrada and at least one Cabinet official said the impending oil price increase, an expected P60- billion budget deficit, and the public opposition to amending the Constitution to allow unbridled foreign investments would make it a difficult time for the Estrada presidency. -

Art of Nation Building
SINING-BAYAN: ART OF NATION BUILDING Social Artistry Fieldbook to Promote Good Citizenship Values for Prosperity and Integrity PHILIPPINE COPYRIGHT 2009 by the United Nations Development Programme Philippines, Makati City, Philippines, UP National College of Public Administration and Governance, Quezon City and Bagong Lumad Artists Foundation, Inc. Edited by Vicente D. Mariano Editorial Assistant: Maricel T. Fernandez Border Design by Alma Quinto Project Director: Alex B. Brillantes Jr. Resident Social Artist: Joey Ayala Project Coordinator: Pauline S. Bautista Siningbayan Pilot Team: Joey Ayala, Pauline Bautista, Jaku Ayala Production Team: Joey Ayala Pauline Bautista Maricel Fernandez Jaku Ayala Ma. Cristina Aguinaldo Mercedita Miranda Vincent Silarde ALL RIGHTS RESERVED Apart from fair dealing for the purpose of research or review, as permitted under the copyright, this book is subject to the condition that it should not, by way of trade or otherwise, be lent, sold, or circulated in any form, without the prior permission in writing of the publisher. The scanning, uploading and distribution of this book via the Internet or via other means without the permission of the publisher is illegal and punishable by applied laws. ALL SONGS COPYRIGHT Joey Ayala PRINTED IN THE PHILIPPINES by JAPI Printzone, Corp. Text Set in Garamond ISBN 978 971 94150 1 5 TABLE OF CONTENTS i MESSAGE Mary Ann Fernandez-Mendoza Commissioner, Civil Service Commission ii FOREWORD Bro. Rolando Dizon, FSC Chair, National Congress on Good Citizenship iv PREFACE: Siningbayan: Art of Nation Building Alex B. Brillantes, Jr. Dean, UP-NCPAG vi ACKNOWLEDGEMENTS vii INTRODUCTION Joey Ayala President, Bagong Lumad Artists Foundation Inc.(BLAFI) 1 Musical Reflection: KUNG KAYA MONG ISIPIN Joey Ayala 2 SININGBAYAN Joey Ayala 5 PART I : PAGSASALOOB (CONTEMPLACY) 9 “BUILDING THE GOOD SOCIETY WE WANT” My Hope as a Teacher in Political and Governance Jose V. -
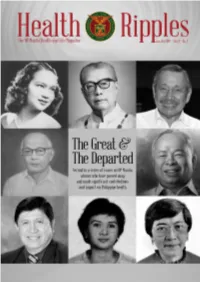
2018 Jan-Jun / Vol. 4 No. 1
The UP Manila Health and Life Magazine i The UP Manila Health Ripples magazine is published bi-annually by the UP Manila Information, Publication, and Public Affairs Office (IPPAO), 8th floor, Philippine General Hospital Central Block, Tel. nos. 554-8400 local 3842. Contributions are welcome. Please email to [email protected] or send to the IPPAO. EDITOR: Cynthia M. Villamor; EDITORIAL CONSULTANT: Dr. Olympia Q. Malanyaon; WRITERS: Cynthia M. Villamor, Fedelynn M. Jemena, January R. Kanindot, Charmaine A. Lingdas; Anne Marie D. Alto LAYOUT ARTIST: Anne Marie D. Alto; PHOTOGRAPHER: Joseph Bautista; CIRCULATION: Sigrid G. Cabiling; Contributing Josephine D. Agapito ii Health Ripples Table of Contents Dr. Florentino B. Herrera, Jr: Humanizing Philippine Medicine 2 Cynthia M. Villamor Dr. Geminiano T. de Ocampo: National Scientist 7 and Father of Modern Philippine Ophthalmology Anne Marie D. Alto Dr. Minda Luz M. Quesada: Passionate Health Champion and Advocate 12 Charmaine A. Lingdas Charlotte A. Floro: Pillar of Rehabilitation Sciences in the Philippines 15 January R. Kanindot Dr. Magdalena C. Cantoria: Advancing Philippine Pharmacy and Botany 19 Fedelynn M. Jemena Dr. Alberto “Quasi” G. Romualdez, Jr.: Crusader for Universal Health Care 22 Charmaine A. Lingdas Dr. Juan M. Flavier: A Doctor for the People 27 Fedelynn M. Jemena Dr. Serafin C. Hilvano: Pillar of Modern Philippine Surgery 32 Cynthia M. Villamor The UP Manila Health and Life Magazine 1 Dr. Florentino B. Herrera, Jr: Humanizing Philippine Medicine By Cynthia M. Villamor “Health must be viewed as both a means to an end and as an end in itself. It is a means insofar as it is a precondition for an individual to harness and maximize his potential as a productive member of the community.