Nonstress Test and Contraction Stress Test - Uptodate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pre-Term Pre-Labour Rupture of Membranes and the Role of Amniocentesis
Fetal and Maternal Medicine Review 2010; 21:2 75–88 C Cambridge University Press 2010 doi:10.1017/S096553951000001X First published online 15 March 2010 PRE-TERM PRE-LABOUR RUPTURE OF MEMBRANES AND THE ROLE OF AMNIOCENTESIS 1,2 ANNA P KENYON, 1,2 KHALIL N ABI-NADER AND 2 PRANAV P PANDYA 1Elizabeth Garrett Anderson Institute for Women’s Health, University College London, 86-96 Chenies Mews, London WCIE 6NX. 2Fetal Medicine Unit, University College London Hospitals NHS Foundation Trust, 235 Euston Rd, London NWI 2BU. INTRODUCTION Pre-labour premature rupture of membranes (PPROM) is defined as rupture of membranes more than 1 hour prior to the onset of labour at <37 weeks gestation. PPROM occurs in approximately 3% of pregnancies and is responsible for a third of all preterm births.1 Once membranes are ruptured prolonging the pregnancy has no maternal physical advantage but fetal morbidity and mortality are improved daily at early gestations: 19% of those infants born <25 weeks develop cerebral palsy (CP) and 28% have severe motor disability.2 Those infants born extremely pre term (<28 weeks) cost the public sector £75835 (95% CI £27906–145508) per live birth3 not to mention the emotional cost to the family. To prolong gestation is therefore the suggested goal: however how and why might we delay birth in those at risk? PPROM is one scenario associated with preterm birth and here we discuss the causative mechanisms, sequelae, latency, strategies to prolong gestation (antibiotics) and consider the role of amniocentesis. We will also discuss novel therapies. PATHOPHYSIOLOGY OF MEMBRANE RUPTURE The membranes, which act to protect and isolate the fetus, are composed of two layers. -

Characteristics of Heart Rate Tracings in Preterm Fetus
medicina Review Characteristics of Heart Rate Tracings in Preterm Fetus Maria F. Hurtado-Sánchez 1, David Pérez-Melero 2, Andrea Pinto-Ibáñez 3 , Ernesto González-Mesa 4 , Juan Mozas-Moreno 1,5,6,7,* and Alberto Puertas-Prieto 1,7 1 Obstetrics and Gynecology Service, Virgen de las Nieves University Hospital, 18014 Granada, Spain; [email protected] (M.F.H.-S.); [email protected] (A.P.-P.) 2 Anesthesiology, Resuscitation and Pain Therapy Service, Virgen de las Nieves University Hospital, 18014 Granada, Spain; [email protected] 3 Obstetrics and Gynecology Service, Poniente Hospital, 04700 El Ejido (Almería), Spain; [email protected] 4 Obstetrics and Gynecology Service, Regional University Hospital of Malaga, 29011 Malaga, Spain; [email protected] 5 Department of Obstetrics and Gynecology, University of Granada, 18016 Granada, Spain 6 Consortium for Biomedical Research in Epidemiology & Public Health (CIBER Epidemiología y Salud Pública-CIBERESP), 28029 Madrid, Spain 7 Biohealth Research Institute (Instituto de Investigación Biosanitaria Ibs.GRANADA), 18014 Granada, Spain * Correspondence: [email protected]; Tel.: +34-958242867 Abstract: Background and Objectives: Prematurity is currently a serious public health issue worldwide, because of its high associated morbidity and mortality. Optimizing the management of these preg- nancies is of high priority to improve perinatal outcomes. One tool frequently used to determine the degree of fetal wellbeing is cardiotocography (CTG). A review of the available literature on fetal heart rate (FHR) monitoring in preterm fetuses shows that studies are scarce, and the evidence thus far is unclear. The lack of reference standards for CTG patterns in preterm fetuses can lead to misinterpretation of the changes observed in electronic fetal monitoring (EFM). -

G Eneral Introduction
Follow-up studies in prenatal medicine Nagel, H.T.C. Citation Nagel, H. T. C. (2007, February 14). Follow-up studies in prenatal medicine. Retrieved from https://hdl.handle.net/1887/9762 Version: Corrected Publisher’s Version Licence agreement concerning inclusion of doctoral thesis in the License: Institutional Repository of the University of Leiden Downloaded from: https://hdl.handle.net/1887/9762 Note: To cite this publication please use the final published version (if applicable). Proefschrift H. Nagel 11-01-2007 13:34 Pagina 11 C H ! T " # $ * eneral introduction 11 Proefschrift H. Nagel 11-01-2007 13:34 Pagina 12 C H ! T " # $ The %etus in prenatal m edicine ccording to M edline de-initions' a conce.tus is an em ,ryo until a .ostconce.tional age o- 9 1 ee2s (or a gestational age o- $* 1 ee2s) and 1 ill then ,e a -etus until ,irth. =- ,orn via,le' the .erson then ,ecom es an in-ant. The -etus is a uni>ue .atient -or several reasons. 6irst' there is a uni>ue relationshi. ,et1 een the m other and her un,orn child. lthough the -etus has his o1 n rights' he or she can only ,e treated via the m other. There-ore the .ur.orted rights o- $ the -etus can never ta2e .recedence over that o- the m other. ;econd' des.ite advances in m edical care there is stri2ing little 2no1 ledge a,out -etal live. ? uestions such as does the -etus [email protected] .ain' does it have a m em ory' are still unans1 ered. -

Prenatal and Preimplantation Genetic Diagnosis for Mps and Related Diseases
PRENATAL AND PREIMPLANTATION GENETIC DIAGNOSIS FOR MPS AND RELATED DISEASES Donna Bernstein, MS Amy Fisher, MS Joyce Fox, MD Families who are concerned about passing on genetic conditions to their children have several options. Two of those options are using prenatal diagnosis and preimplantation genetic diagnosis. Prenatal diagnosis is a method of testing a pregnancy to learn if it is affected with a genetic condition. Preimplantation genetic diagnosis, also called PGD, is a newer technology used to test a fertilized embryo before a pregnancy is established, utilizing in vitro fertilization (IVF). Both methods provide additional reproductive options to parents who are concerned about having a child with a genetic condition. There are two types of prenatal diagnosis; one is called amniocentesis, and the other is called CVS (chorionic villus sampling). Amniocentesis is usually performed between the fifteenth and eighteenth weeks of pregnancy. Amniocentesis involves inserting a fine needle into the uterus through the mother's abdomen and extracting a few tablespoons of amniotic fluid. Skin cells from the fetus are found in the amniotic fluid. These cells contain DNA, which can be tested to see if the fetus carries the same alterations in the genes (called mutations) that cause a genetic condition in an affected family member. If the specific mutation in the affected individual is unknown, it is possible to test the enzyme activity in the cells of the fetus. Although these methods are effective at determining whether a pregnancy is affected or not, they do not generally give information regarding the severity or the course of the condition. -

L&D – Amnioinfusion Guideline and Procedure for Amnioinfusion
L&D – Amnioinfusion Guideline and Procedure for Amnioinfusion. Purpose: Replacing the amniotic fluid with normal saline has been found to be a safe, simple, and very effective way to reduce the occurrence of repetitive variable decelerations. Procedure: Initiation of Amnioinfusion will be ordered and performed by a Certified Nurse Midwife (CNM) or physician (MD). 1. Prepare NS or LR 1000ml with IV tubing in the same fashion as for intravenous infusion. Flush the tubing to clear air. 2. An intrauterine pressure catheter (IUPC) will be placed by the MD/CNM. 3. Elevate the IV bag 3-4 feet above the IUPC tip for rapid infusion. Infuse 250-500ml of solution over a 20-30 minute time frame followed by a 60-180ml/hour maintenance infusion. The total volume infused should not exceed 1000ml unless one has access to ultrasound and can titrate to an amniotic fluid index (AFI) of 8-12 cm to prevent polyhydramnios and hypertonus. 4. If variable decelerations recur or other new non-reassuring FHR patterns develop, notify the MD/CNM. The procedure may be repeated as ordered. 5. Resting tone of the uterus will be increased during infusion but should not increase > 15mmHg from previous baseline. If this occurs, infusion should stop until there is a return to the previous baseline then it can be restarted. An elevated baseline prior to infusion is a contraindication. 6. Monitor for an outflow of infusion. If there is a sudden cessation of outflow fetal head engagement may have occurred increasing the risk of polyhydramnios. Complications are rare but can include iatrogenic polyhydramnios, uterine hypertonus, chorioamnionitis, uterine rupture, placental abruption, and maternal pulmonary embolus. -

Proteomic Biomarkers of Intra-Amniotic Inflammation
0031-3998/07/6103-0318 PEDIATRIC RESEARCH Vol. 61, No. 3, 2007 Copyright © 2007 International Pediatric Research Foundation, Inc. Printed in U.S.A. Proteomic Biomarkers of Intra-amniotic Inflammation: Relationship with Funisitis and Early-onset Sepsis in the Premature Neonate CATALIN S. BUHIMSCHI, IRINA A. BUHIMSCHI, SONYA ABDEL-RAZEQ, VICTOR A. ROSENBERG, STEPHEN F. THUNG, GUOMAO ZHAO, ERICA WANG, AND VINEET BHANDARI Department of Obstetrics, Gynecology and Reproductive Sciences [C.S.B., I.A.B., S.A.-R., V.A.R., S.F.T., G.Z., E.W.], and Department of Pediatrics [V.B.], Division of Perinatal Medicine, Yale University School of Medicine, New Haven, CT 06520 ABSTRACT: Our goal was to determine the relationship between 4 vein inflammatory cytokine levels, but not maternal serum val- amniotic fluid (AF) proteomic biomarkers (human neutrophil de- ues, correlate with the presence and severity of the placental fensins 2 and 1, calgranulins C and A) characteristic of intra-amniotic histologic inflammation and umbilical cord vasculitis (7). inflammation, and funisitis and early-onset sepsis in premature neo- Funisitis is characterized by perivascular infiltrates of in- nates. The mass restricted (MR) score was generated from AF flammatory cells and is considered one of the strongest hall- obtained from women in preterm labor (n ϭ 123). The MR score marks of microbial invasion of the amniotic cavity and fetal ranged from 0–4 (none to all biomarkers present). Funisitis was graded histologically and interpreted in relation to the MR scores. inflammatory syndrome (8,9). While there is some debate with Neonates (n ϭ 97) were evaluated for early-onset sepsis. -
Amniotic Fluid Volume: When and How to Take Action
Amniotic fluid volume: When and how to take action http://contemporaryobgyn.modernmedicine.com/pr... Published on Contemporary OB/GYN (http://contemporaryobgyn.modernmedicine.com) Amniotic fluid volume: When and how to take action Alessandro Ghidini, MD and Marta Schilirò, MD and Anna Locatelli, MD Publish Date: JUN 01,2014 Dr. Ghidini is Professor, Georgetown University, Washington, DC, and Director, Perinatal Diagnostic Center, Inova Alexandria Hospital, Alexandria, Virginia. Dr. Schilirò is Medical Doctor, Obstetrics and Gynecology, University of Milano-Bicocca, Monza, Italy. Dr. Locatelli is Associate Professor, University of Milano-Bicocca, Monza, Italy, and Director, Department of Obstetrics and Gynecology, Carate- Giussano Hospital, AO Vimercate-Desio, Italy. None of the authors has a conflict of interest to report with respect to the content of this article. Assessment of amniotic fluid volume (AFV) is an integral part of antenatal ultrasound evaluation during screening exams, targeted anatomy examinations, and in tests assessing fetal well-being. 1 di 17 18/06/2014 11:10 Amniotic fluid volume: When and how to take action http://contemporaryobgyn.modernmedicine.com/pr... Abnormal AFV has been associated with an increased risk of perinatal mortality and several adverse perinatal outcomes, including premature rupture of membranes (PROM), fetal abnormalities, abnormal birth weight, and increased risk of obstetric interventions.1 A recent systematic review demonstrated associations between oligohydramnios, birthweight <10th percentile, and perinatal mortality, as well as between polyhydramnios, birthweight >90th percentile, and perinatal mortality. The predictive ability of AFV alone, however, was generally poor.2 How to assess AFV Ultrasound (U/S) examination is the only practical method of assessing AFV. -
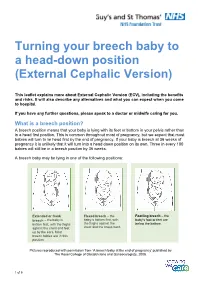
Turning Your Breech Baby to a Head-Down Position (External Cephalic Version)
Turning your breech baby to a head-down position (External Cephalic Version) This leaflet explains more about External Cephalic Version (ECV), including the benefits and risks. It will also describe any alternatives and what you can expect when you come to hospital. If you have any further questions, please speak to a doctor or midwife caring for you. What is a breech position? A breech position means that your baby is lying with its feet or bottom in your pelvis rather than in a head first position. This is common throughout most of pregnancy, but we expect that most babies will turn to lie head first by the end of pregnancy. If your baby is breech at 36 weeks of pregnancy it is unlikely that it will turn into a head down position on its own. Three in every 100 babies will still be in a breech position by 36 weeks. A breech baby may be lying in one of the following positions: Extended or frank Flexed breech – the Footling breech – the breech – the baby is baby is bottom first, with baby’s foot or feet are bottom first, with the thighs the thighs against the below the bottom. against the chest and feet chest and the knees bent. up by the ears. Most breech babies are in this position. Pictures reproduced with permission from ‘A breech baby at the end of pregnancy’ published by The Royal College of Obstetricians and Gynaecologists, 2008. 1 of 5 What causes breech? Breech is more common in women who are expecting twins, or in women who have a differently-shaped womb (uterus). -

Fetal Assement Methods
12/3/2020 Fetal Assement Methods 1 up to 9% of exam 5 to 9 questions 13.00 Adjunct Fetal Surveillance Methods 10%) 13.01 Auscultation (Intermittent Auscultation- IA) 13.02 Fetal movement counting 13.03 Nonstress testing 13.04 Fetal acid base interpretation – will be covered in a separate section 13.05 Biophysical profile 13.06 Fetal Acoustic Stimulation 2 1 12/3/2020 HERE IS ONE FOR YOU!! AWW… Skin to Skin in the OR ☺ 3 Auscultation 4 2 12/3/2020 Benefits of Auscultation • Based on Random Control Trials, neonatal outcomes are comparable to those monitored with EFM • Lower CS rates • Technique is non-invasive • Widespread application is possible • Freedom of movement • Lower cost • Hands on Time and one to one support are facilitated 5 Limitation of Auscultation • Use of the Fetoscope may limit the ability to hear FHR ( obesity, amniotic fluid, pt. movement and uterine contractions) • Certain FHR patterns cannot be detected – variability and some decelerations • Some women may think IA is intrusive • Documentation is not automatic • Potential to increase staff for 1:1 monitoring • Education, practice and skill assessment of staff 6 3 12/3/2020 Auscultation • Non-electronic devices such as a Fetoscope or Stethoscope • No longer common practice in the United States though may be increasing due to patient demand • Allows listening to sounds associated with the opening and closing of ventricular valves via bone conduction • Can hear actual heart sounds 7 Auscultation Fetoscope • A Fetoscope can detect: • FHR baseline • FHR Rhythm • Detect accelerations and decelerations from the baseline • Verify an FHR irregular rhythm • Can clarify double or half counting of EFM • AWHONN, (2015), pp. -

ENT of UATION MEMOR the HUMAN FETUS Cothelijne Van Heter
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/146798 Please be advised that this information was generated on 2021-09-24 and may be subject to change. ENT OF UATION MEMOR THE HUMAN FETUS Cothelijne van Heter • DEVELOPMENT OF HABITUATION AND MEMORY IN THE HUMAN FETUS Van Heteren, Cathelijne Francisca - Development of habituation and memory in the human fetus - 2001 Thesis University Nijmegen - with réf.- with summary m Dutch -136 p. ISBN: 90-9015000-5 Print: Grafisch Bedrijf Ponsen &i Looijen BV Wageningen Graphic Design Marie-Louise Dusée No part of this book may be reproduced in any form without permission of the author. This research project was financially supported by ZorgOnderzoek Nederland and the Hersenstichting Nederland. Publication of this thesis was financially supported by ATL Nederland BV, Ferring BV, GlaxoSmithKline, Hitachi Ultrasound BV, Medical Dynamics, Novo Nordisk Farma BV, Organon Nederland BV, Pie Medical Benelux BV, Sanofi-Synthélabo, Schering Nederland BV. DEVELOPMENT OF HABITUATION AND MEMORY IN THE HUMAN ?-f τ'••<, Een wetenschappelijke proeve op het gebied van de Medische Wetenschappen Proefschrift ter verkrijging van de graad van doctor aan de Katholieke Universiteit Nijmegen, volgens besluit van het College van Decanen in het openbaar te verdedigen op vrijdag 5 oktober 2001 des namiddags om 1.30 uur precies door Cathelijne Francisca van Heteren -

Cutoff Point Amniotic Fluid Index and Pregnancy Prognosis in the Third Trimester of Pregnancy in Shariati Hospital of Bandar Abbas in 2013-14
Available online at www.ijmrhs.com International Journal of Medical Research & ISSN No: 2319-5886 Health Sciences, 2016, 5, 12:212-216 Cutoff point amniotic fluid index and pregnancy prognosis in the third trimester of pregnancy in Shariati Hospital of Bandar Abbas in 2013-14 AzinAlavi 1, Najmesadat Mosallanezhad 1,Hosein Hamadiyan 2, Mohammad Amin Sepehri Oskooe 2 and Keivan Dolati 2* 1Fertility and Infertility Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran 2Student Research Committee, Hormozgan University of Medical Sciences, Bandar Abbas, Iran *CorrespondingEmail:[email protected] _____________________________________________________________________________________________ ABSTRACT Background and purpose of study: Amniotic fluid volume varies according to different stages of fetal growth and its different requirements. Disrupted amniotic fluid volume is associated with an increased risk for the fetus. The present research aims to investigate the effect of cutoff point amniotic fluid index on pregnancy prognosis at the third trimester of pregnancy in Shariati hospital of Bandar Abbas. Materials and methods: In the present analytical, cross-sectional research, AFI ≤ 5 cm was considered as oligohydramnios; AFI 5.1-8 was taken as the cut-off point; AFI ˃ 8.1-24 was regarded as normal; AFI ˃ 24 was considered as polyhydramnios. The data were analyzed via SPSS version 16.0 using Chi-squared test, Fisher’s test, Mann-Whitney U-test and Spearman’s correlation coefficient. P-value was set at ≤ .05 for the significance of data. Findings: Subjects with cut-off point AFI (5.1-8) were 38 (40.4%); those with normal AFI (8.1-24) were 56 (59.6%). The mean score of AFI was 8.85±9.54cm. -

Guidelines for Perinatal Care, 8Th Ed., Pp. 48-49, 198-205 ACOG Practice Bulletin, No 145, July 2014, Reaffirmed 2016 JOGNN, No
Guidelines for Perinatal Care, 8th ed., pp. 48-49, 198-205 ACOG Practice Bulletin, No 145, July 2014, Reaffirmed 2016 JOGNN, No. 44, pp. 683-686, 2015 Terminology and interpretation of electronic fetal monitoring tracings as defined by National Institute of Child Health and Development (NICHD) Maternal Health Competencies - Fetal Assessment & Antenatal Fetal Surveillance Fetal Heart Tones (Beginning at 10 Weeks Gestation with hand-held Doppler) 1. Review provider or standing order 2. Explain procedure and obtains patient's verbal consent 3. Perform hand hygiene prior to engaging with patient 4. Assist patient into semi-recumbent position, expose abdomen 5. Locate the point of loudest fetal heart tones and a. Palpate maternal pulse b. Utilize pulse oximetry (placed on maternal index finger) 6. Monitor maternal pulse and count fetal heart rate for 1 full minute 7. Record findings 8. Demonstrate knowledge of fetal heart rate ranges: a. Normal = 110-160 bpm b. Bradycardia = < 110 bpm c. Tachycardia = > 160 bpm 9. Demonstrate knowledge of criteria for notifying provider of concerns/findings before, during, or after assessment (per clinical policies) Fundal Height (Beginning at 12 to 14 Weeks gestation) 1. Review provider or standing order 2. Explain procedure and obtain patient's verbal consent 3. Perform hand hygiene prior to engaging with patient 4. Assist patient to semi-recumbent position, expose abdomen 5. Ensure the abdomen is soft and palpates with 2 hands to locate the uterine fundus 6. Measure from top of fundus to top of symphysis pubis using a pliable, non-elastic tape measure, keeping the tape measure in contact with the skin, and measuring along the longitudinal axis without correcting to the abdominal midline 7.