A Comparative Pilot Study of Bacterial and Fungal Dysbiosis In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ustilago: Habitat, Symptoms and Reproduction | Teliomycetes
Ustilago: Habitat, Symptoms and Reproduction | Teliomycetes For B.Sc. Botany 1st By Dr. Meenu Gupta Assistant Professor Botany J.D.W.C. Patna 1. Habit and Habitat of Ustilago: Ustilago, the largest genus of the family Ustilaginaceae is represented by more than 400 cosmopolitan species. Butler and Bisby (1958) reported 108 species from India. All species are parasitic and infect the floral parts of wheat, barley, oat, maize, sugarcane, Bajra, rye and wild grasses. The name Ustilago has been derived from a Latin word ustus meaning ‘burnt’ because the members of the genus produce black, sooty powdery mass of spores on the host plant parts imparting them a ‘burnt’ appearance. This black dusty mass of spores resembles soot or smut, therefore, commonly it is also known as smut fungus. The fungus is of much economic importance, because it causes heavy loss to various economically important plants. This genus is very common in U.P., Bihar, Punjab and Madhya Pradesh. 2. Symptoms of Ustilago: The symptoms appear only on the floral parts. The floral spikes turn black and remain filled with the smut spores. Ustilago produces two main types of symptoms: 1. The blackish powder of spores is easily blown away by the wind, leaving a bare stalk of inflorescence (Fig. 1 B). Species showing such symptoms are called loose smuts e.g., (a) Loose smut of oat caused by U. avenae (b) Loose smut of barley caused by U. nuda (c) Loose smut of wheat caused by U. nuda var. tritici. (Fig. 13A, B). (d) Loose smut of doob grass caused by U. -

Gut Microbiota Beyond Bacteria—Mycobiome, Virome, Archaeome, and Eukaryotic Parasites in IBD
International Journal of Molecular Sciences Review Gut Microbiota beyond Bacteria—Mycobiome, Virome, Archaeome, and Eukaryotic Parasites in IBD Mario Matijaši´c 1,* , Tomislav Meštrovi´c 2, Hana Cipˇci´cPaljetakˇ 1, Mihaela Peri´c 1, Anja Bareši´c 3 and Donatella Verbanac 4 1 Center for Translational and Clinical Research, University of Zagreb School of Medicine, 10000 Zagreb, Croatia; [email protected] (H.C.P.);ˇ [email protected] (M.P.) 2 University Centre Varaždin, University North, 42000 Varaždin, Croatia; [email protected] 3 Division of Electronics, Ruđer Boškovi´cInstitute, 10000 Zagreb, Croatia; [email protected] 4 Faculty of Pharmacy and Biochemistry, University of Zagreb, 10000 Zagreb, Croatia; [email protected] * Correspondence: [email protected]; Tel.: +385-01-4590-070 Received: 30 January 2020; Accepted: 7 April 2020; Published: 11 April 2020 Abstract: The human microbiota is a diverse microbial ecosystem associated with many beneficial physiological functions as well as numerous disease etiologies. Dominated by bacteria, the microbiota also includes commensal populations of fungi, viruses, archaea, and protists. Unlike bacterial microbiota, which was extensively studied in the past two decades, these non-bacterial microorganisms, their functional roles, and their interaction with one another or with host immune system have not been as widely explored. This review covers the recent findings on the non-bacterial communities of the human gastrointestinal microbiota and their involvement in health and disease, with particular focus on the pathophysiology of inflammatory bowel disease. Keywords: gut microbiota; inflammatory bowel disease (IBD); mycobiome; virome; archaeome; eukaryotic parasites 1. Introduction Trillions of microbes colonize the human body, forming the microbial community collectively referred to as the human microbiota. -

The Ustilaginales (Smut Fungi) of Ohio*
THE USTILAGINALES (SMUT FUNGI) OF OHIO* C. W. ELLETT Department of Botany and Plant Pathology, The Ohio State University, Columbus 10 The smut fungi are in the order Ustilaginales with one family, the Ustilaginaceae, recognized. They are all plant parasites. In recent monographs 276 species in 22 genera are reported in North America and more than 1000 species have been reported from the world (Fischer, 1953; Zundel, 1953; Fischer and Holton, 1957). More than one half of the known smut fungi are pathogens of species in the Gramineae. Most of the smut fungi are recognized by the black or brown spore masses or sori forming in the inflorescences, the leaves, or the stems of their hosts. The sori may involve the entire inflorescence as Ustilago nuda on Hordeum vulgare (fig. 2) and U. residua on Danthonia spicata (fig. 7). Tilletia foetida, the cause of bunt of wheat in Ohio, sporulates in the ovularies only and Ustilago violacea which has been found in Ohio on Silene sp. forms spores only in the anthers of its host. The sori of Schizonella melanogramma on Carex (fig. 5) and of Urocystis anemones on Hepatica (fig. 4) are found in leaves. Ustilago striiformis (fig. 6) which causes stripe smut of many grasses has sori which are mostly in the leaves. Ustilago parlatorei, found in Ohio on Rumex (fig. 3), forms sori in stems, and in petioles and midveins of the leaves. In a few smut fungi the spore masses are not conspicuous but remain buried in the host tissues. Most of the species in the genera Entyloma and Doassansia are of this type. -

Fungal Evolution: Major Ecological Adaptations and Evolutionary Transitions
Biol. Rev. (2019), pp. 000–000. 1 doi: 10.1111/brv.12510 Fungal evolution: major ecological adaptations and evolutionary transitions Miguel A. Naranjo-Ortiz1 and Toni Gabaldon´ 1,2,3∗ 1Department of Genomics and Bioinformatics, Centre for Genomic Regulation (CRG), The Barcelona Institute of Science and Technology, Dr. Aiguader 88, Barcelona 08003, Spain 2 Department of Experimental and Health Sciences, Universitat Pompeu Fabra (UPF), 08003 Barcelona, Spain 3ICREA, Pg. Lluís Companys 23, 08010 Barcelona, Spain ABSTRACT Fungi are a highly diverse group of heterotrophic eukaryotes characterized by the absence of phagotrophy and the presence of a chitinous cell wall. While unicellular fungi are far from rare, part of the evolutionary success of the group resides in their ability to grow indefinitely as a cylindrical multinucleated cell (hypha). Armed with these morphological traits and with an extremely high metabolical diversity, fungi have conquered numerous ecological niches and have shaped a whole world of interactions with other living organisms. Herein we survey the main evolutionary and ecological processes that have guided fungal diversity. We will first review the ecology and evolution of the zoosporic lineages and the process of terrestrialization, as one of the major evolutionary transitions in this kingdom. Several plausible scenarios have been proposed for fungal terrestralization and we here propose a new scenario, which considers icy environments as a transitory niche between water and emerged land. We then focus on exploring the main ecological relationships of Fungi with other organisms (other fungi, protozoans, animals and plants), as well as the origin of adaptations to certain specialized ecological niches within the group (lichens, black fungi and yeasts). -

Plant Life MagillS Encyclopedia of Science
MAGILLS ENCYCLOPEDIA OF SCIENCE PLANT LIFE MAGILLS ENCYCLOPEDIA OF SCIENCE PLANT LIFE Volume 4 Sustainable Forestry–Zygomycetes Indexes Editor Bryan D. Ness, Ph.D. Pacific Union College, Department of Biology Project Editor Christina J. Moose Salem Press, Inc. Pasadena, California Hackensack, New Jersey Editor in Chief: Dawn P. Dawson Managing Editor: Christina J. Moose Photograph Editor: Philip Bader Manuscript Editor: Elizabeth Ferry Slocum Production Editor: Joyce I. Buchea Assistant Editor: Andrea E. Miller Page Design and Graphics: James Hutson Research Supervisor: Jeffry Jensen Layout: William Zimmerman Acquisitions Editor: Mark Rehn Illustrator: Kimberly L. Dawson Kurnizki Copyright © 2003, by Salem Press, Inc. All rights in this book are reserved. No part of this work may be used or reproduced in any manner what- soever or transmitted in any form or by any means, electronic or mechanical, including photocopy,recording, or any information storage and retrieval system, without written permission from the copyright owner except in the case of brief quotations embodied in critical articles and reviews. For information address the publisher, Salem Press, Inc., P.O. Box 50062, Pasadena, California 91115. Some of the updated and revised essays in this work originally appeared in Magill’s Survey of Science: Life Science (1991), Magill’s Survey of Science: Life Science, Supplement (1998), Natural Resources (1998), Encyclopedia of Genetics (1999), Encyclopedia of Environmental Issues (2000), World Geography (2001), and Earth Science (2001). ∞ The paper used in these volumes conforms to the American National Standard for Permanence of Paper for Printed Library Materials, Z39.48-1992 (R1997). Library of Congress Cataloging-in-Publication Data Magill’s encyclopedia of science : plant life / edited by Bryan D. -

How Mycobiome/Bacteriome Work Together Personal Story!!!
5/15/2017 Cooperative Evolutionary Strategies: Personal Story!!! How Mycobiome/Bacteriome Work • In 1974 my PHD advisor handed me a paper showing that rabbits treated with antibiotics or anti-inflammatory steroids Together developed the fungal infection candidiasis • It made me realize that not only could fungi in the environment negatively impact our health, but fungal species also inhabit the mammalian body, alongside diverse commensal bacteria. • When one microbial community is knocked out, another can Mahmoud A Ghannoum, Ph.D., MBA, FIDSA cause illness. Professor and Director, Center for Medical Mycology, Case Western Reserve University • If the communities are undisturbed, however, the fungal Cleveland, OH inhabitants appear to be harmless or perhaps even beneficial. This realization happened 42 Years Ago!!! Researching the Mycobiome • As of November 2015, only 269 of more than 6,000 Web of Science search results for the term “microbiome” even mention “fungus” • The scientific search engine returns only 55 papers pertaining to the Opined: “mycobiome” - That future human microbiome studies should be expanded beyond bacteria to include fungi, viruses, and other microbes in the same samples. - Such studies will allow a better understanding of the role of these communities in health and disease Ghannoum & Mukherjee (2010). Microbe 5(11) The Scientist. 02.2016. 35 1 5/15/2017 The Human Mycobiome Time for a New Perspective Regarding the Role of Fungi in Health and Disease ORAL CAVITY LUNGS GASTRO- SKIN INTESTINAL • Historically, fungi were considered passive colonizers of the microbial community that could become pathogenic • Alternaria • Candida • Aspergillus • Cryptococcus as the result of a change in the environment. -
9B Taxonomy to Genus
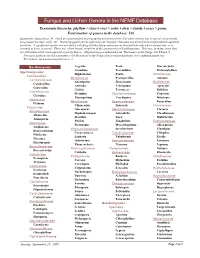
Fungus and Lichen Genera in the NEMF Database Taxonomic hierarchy: phyllum > class (-etes) > order (-ales) > family (-ceae) > genus. Total number of genera in the database: 526 Anamorphic fungi (see p. 4), which are disseminated by propagules not formed from cells where meiosis has occurred, are presently not grouped by class, order, etc. Most propagules can be referred to as "conidia," but some are derived from unspecialized vegetative mycelium. A significant number are correlated with fungal states that produce spores derived from cells where meiosis has, or is assumed to have, occurred. These are, where known, members of the ascomycetes or basidiomycetes. However, in many cases, they are still undescribed, unrecognized or poorly known. (Explanation paraphrased from "Dictionary of the Fungi, 9th Edition.") Principal authority for this taxonomy is the Dictionary of the Fungi and its online database, www.indexfungorum.org. For lichens, see Lecanoromycetes on p. 3. Basidiomycota Aegerita Poria Macrolepiota Grandinia Poronidulus Melanophyllum Agaricomycetes Hyphoderma Postia Amanitaceae Cantharellales Meripilaceae Pycnoporellus Amanita Cantharellaceae Abortiporus Skeletocutis Bolbitiaceae Cantharellus Antrodia Trichaptum Agrocybe Craterellus Grifola Tyromyces Bolbitius Clavulinaceae Meripilus Sistotremataceae Conocybe Clavulina Physisporinus Trechispora Hebeloma Hydnaceae Meruliaceae Sparassidaceae Panaeolina Hydnum Climacodon Sparassis Clavariaceae Polyporales Gloeoporus Steccherinaceae Clavaria Albatrellaceae Hyphodermopsis Antrodiella -

The Gut-Lung Axis in Health and Respiratory Diseases: a Place for Inter-Organ and Inter-Kingdom Crosstalks
MINI REVIEW published: 19 February 2020 doi: 10.3389/fcimb.2020.00009 The Gut-Lung Axis in Health and Respiratory Diseases: A Place for Inter-Organ and Inter-Kingdom Crosstalks Raphaël Enaud 1,2,3*†, Renaud Prevel 2,3,4†, Eleonora Ciarlo 5, Fabien Beaufils 2,3,6, Gregoire Wieërs 7, Benoit Guery 5 and Laurence Delhaes 2,3,8 1 CHU de Bordeaux, CRCM Pédiatrique, CIC 1401, Bordeaux, France, 2 Univ. Bordeaux, Centre de Recherche Cardio-Thoracique de Bordeaux, U1045, Bordeaux, France, 3 CHU de Bordeaux, Univ. Bordeaux, FHU ACRONIM, Bordeaux, France, 4 CHU de Bordeaux, Médecine Intensive Réanimation, Bordeaux, France, 5 Infectious Diseases Service, Department of Medicine, Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland, 6 CHU de Bordeaux, Service d’Explorations Fonctionnelles Respiratoires, Bordeaux, France, 7 Clinique Saint Pierre, Department of Internal Medicine, Ottignies, Belgium, 8 CHU de Bordeaux: Laboratoire de Parasitologie-Mycologie, Univ. Bordeaux, Bordeaux, France Edited by: Yongqun Oliver He, The gut and lungs are anatomically distinct, but potential anatomic communications and University of Michigan, United States complex pathways involving their respective microbiota have reinforced the existence of a Reviewed by: Xingmin Sun, gut–lung axis (GLA). Compared to the better-studied gut microbiota, the lung microbiota, University of South Florida, only considered in recent years, represents a more discreet part of the whole microbiota United States Gyanendra Prakash Dubey, associated to human hosts. While the vast majority of studies focused on the bacterial Institut Pasteur, France component of the microbiota in healthy and pathological conditions, recent works have Hong Yu, highlighted the contribution of fungal and viral kingdoms at both digestive and respiratory Guizhou Provincial People’s Hospital, China levels. -

<I>Ustilago-Sporisorium-Macalpinomyces</I>
Persoonia 29, 2012: 55–62 www.ingentaconnect.com/content/nhn/pimj REVIEW ARTICLE http://dx.doi.org/10.3767/003158512X660283 A review of the Ustilago-Sporisorium-Macalpinomyces complex A.R. McTaggart1,2,3,5, R.G. Shivas1,2, A.D.W. Geering1,2,5, K. Vánky4, T. Scharaschkin1,3 Key words Abstract The fungal genera Ustilago, Sporisorium and Macalpinomyces represent an unresolved complex. Taxa within the complex often possess characters that occur in more than one genus, creating uncertainty for species smut fungi placement. Previous studies have indicated that the genera cannot be separated based on morphology alone. systematics Here we chronologically review the history of the Ustilago-Sporisorium-Macalpinomyces complex, argue for its Ustilaginaceae resolution and suggest methods to accomplish a stable taxonomy. A combined molecular and morphological ap- proach is required to identify synapomorphic characters that underpin a new classification. Ustilago, Sporisorium and Macalpinomyces require explicit re-description and new genera, based on monophyletic groups, are needed to accommodate taxa that no longer fit the emended descriptions. A resolved classification will end the taxonomic confusion that surrounds generic placement of these smut fungi. Article info Received: 18 May 2012; Accepted: 3 October 2012; Published: 27 November 2012. INTRODUCTION TAXONOMIC HISTORY Three genera of smut fungi (Ustilaginomycotina), Ustilago, Ustilago Spo ri sorium and Macalpinomyces, contain about 540 described Ustilago, derived from the Latin ustilare (to burn), was named species (Vánky 2011b). These three genera belong to the by Persoon (1801) for the blackened appearance of the inflores- family Ustilaginaceae, which mostly infect grasses (Begerow cence in infected plants, as seen in the type species U. -

Lecanicillium Fungicola 150-1, the Causal Agent of Dry Bubble Disease Downloaded From
GENOME SEQUENCES crossm Genome Sequence of Lecanicillium fungicola 150-1, the Causal Agent of Dry Bubble Disease Downloaded from Alice M. Banks,a* Farhana Aminuddin,a Katherine Williams,a Thomas Batstone,a Gary L. A. Barker,a Gary D. Foster,a Andy M. Baileya aSchool of Biological Sciences, University of Bristol, Bristol, United Kingdom ABSTRACT The fungus Lecanicillium fungicola causes dry bubble disease in the http://mra.asm.org/ white button mushroom Agaricus bisporus. Control strategies are limited, as both the host and pathogen are fungi, and there is limited understanding of the interac- tions in this pathosystem. Here, we present the genome sequence of Lecanicillium fungicola strain 150-1. ecanicillium fungicola (Preuss) Zare & Gams [synonym: Verticillium fungicola (Preuss) LHassebrauk] (1), an ascomycete fungus of the order Hypocreales, is the causal agent of dry bubble disease of the white button mushroom Agaricus bisporus, as well as of on September 18, 2020 at Imperial College London other commercially cultivated basidiomycetes (2). Dry bubble disease presents symp- toms that include necrotic lesions on mushroom caps, stipe blowout, and undifferen- tiated tissue masses (2). Some factors involved in this interaction have been proposed based on suppression subtractive hybridization (SSH) and expressed sequence tag (EST) data (3). This disease is of economic importance, causing significant yield/quality losses in the mushroom industry (4). Control methods rely on rigorous hygiene procedures and targeted fungicide treatments; however, increased resistance against these fungi- cides has been reported (5, 6). Recent taxonomic revisions place L. fungicola close to several arthropod- and nematode-pathogenic fungi rather than to plant-pathogenic Verticillium spp. -

The Forgotten World of Mycobiome in the Skin of Dogs
ADVERTIMENT. Lʼaccés als continguts dʼaquesta tesi queda condicionat a lʼacceptació de les condicions dʼús establertes per la següent llicència Creative Commons: http://cat.creativecommons.org/?page_id=184 ADVERTENCIA. El acceso a los contenidos de esta tesis queda condicionado a la aceptación de las condiciones de uso establecidas por la siguiente licencia Creative Commons: http://es.creativecommons.org/blog/licencias/ WARNING. The access to the contents of this doctoral thesis it is limited to the acceptance of the use conditions set by the following Creative Commons license: https://creativecommons.org/licenses/?lang=en THE FORGOTTEN WORLD OF MYCOBIOME IN THE SKIN OF DOGS Thesis submitted for the degree of Doctor (PhD) Sara D’Andreano Departament de Ciència Animal i dels Aliments Facultat de Veterinària, Universitat Autònoma de Barcelona Bellaterra, 2020 Director: Dr. Olga Francino Martí Tutor: Dr. Armand Sánchez Bonastre 1 2 La Dra. Olga Francino Martí, investigadora del Departament de Ciència animal I dels Aliments de la Universitat Autònoma de Barcelona i el Dr. Armand Sánchez Bonastre, catedràtic de Genètica Animal de la Universitat Autònoma de Barcelona CERTIFIQUEN Que la Tesi Doctoral amb títol “The forgotten world of mycobiome in the skin of dogs”, presentada per a Sara D’Andreano, s’ha dut a terme sota les seves direccions i s’ha realitzat al Departament de Ciència Animal i dels Aliments de la Facultat Veterinària de la Universitat Autònoma de Barcelona (UAB). Bellaterra, juliol 2020 Firmado Armand digitalmente por Armand Sanchez Sanchez Bonastre Fecha: 2020.06.26 Bonastre 11:10:32 +02'00' Dra. Olga Francino Martí Dr. Armand Sánchez Bonastre (Director de tesi) (Tutor de tesi) Sara D’Andreano (doctoranda) 3 4 This work was supported by a grant awarded by Pla de Doctorats Industrial (2015 DI 044) provided by the Agencia de Gestió d’Ajuts Universitaris i de Recerca (AGAUR); Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement de la Generalitat de Catalunya. -

Culture Inventory
For queries, contact the SFA leader: John Dunbar - [email protected] Fungal collection Putative ID Count Ascomycota Incertae sedis 4 Ascomycota Incertae sedis 3 Pseudogymnoascus 1 Basidiomycota Incertae sedis 1 Basidiomycota Incertae sedis 1 Capnodiales 29 Cladosporium 27 Mycosphaerella 1 Penidiella 1 Chaetothyriales 2 Exophiala 2 Coniochaetales 75 Coniochaeta 56 Lecythophora 19 Diaporthales 1 Prosthecium sp 1 Dothideales 16 Aureobasidium 16 Dothideomycetes incertae sedis 3 Dothideomycetes incertae sedis 3 Entylomatales 1 Entyloma 1 Eurotiales 393 Arthrinium 2 Aspergillus 172 Eladia 2 Emericella 5 Eurotiales 2 Neosartorya 1 Paecilomyces 13 Penicillium 176 Talaromyces 16 Thermomyces 4 Exobasidiomycetes incertae sedis 7 Tilletiopsis 7 Filobasidiales 53 Cryptococcus 53 Fungi incertae sedis 13 Fungi incertae sedis 12 Veroneae 1 Glomerellales 1 Glomerella 1 Helotiales 34 Geomyces 32 Helotiales 1 Phialocephala 1 Hypocreales 338 Acremonium 20 Bionectria 15 Cosmospora 1 Cylindrocarpon 2 Fusarium 45 Gibberella 1 Hypocrea 12 Ilyonectria 13 Lecanicillium 5 Myrothecium 9 Nectria 1 Pochonia 29 Purpureocillium 3 Sporothrix 1 Stachybotrys 3 Stanjemonium 2 Tolypocladium 1 Tolypocladium 2 Trichocladium 2 Trichoderma 171 Incertae sedis 20 Oidiodendron 20 Mortierellales 97 Massarineae 2 Mortierella 92 Mortierellales 3 Mortiererallales 2 Mortierella 2 Mucorales 109 Absidia 4 Backusella 1 Gongronella 1 Mucor 25 RhiZopus 13 Umbelopsis 60 Zygorhynchus 5 Myrmecridium 2 Myrmecridium 2 Onygenales 4 Auxarthron 3 Myceliophthora 1 Pezizales 2 PeZiZales 1 TerfeZia 1