Smart Synthetic Biomaterials for Therapeutic Applications Tianxin Miao University of Vermont
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lipid Rafts and Caveolae
46 Scaffolding SCAFFOLDING 1 NANOCELLBIOLOGY: CELL SURFACE PORTALS – CLATHRIN-COATED PITS, LIPID RAFTS, CAVEOLAE, AND POROSOMES A new field in biology, nanocellbiology (nano cell biol- About 280 years later, the transmission electron micro- ogy), has emerged from the successful use of atomic force scope was invented. Hence, on July 6, 1944 in Rockefeller microscopy, in combination with electron microscopy and Institute for Medical Research, New York, NY, Albert Claude other methods, in understanding the structure and dynamics made the first 13 micrographs taken from (cultured) cells. of cells and biomolecules at nanoscale resolution (1-3) (Fig- Thirty years later, in 1974, Albert Claude, Christian de Duve ure 1). and George Palade shared the Nobel Prize for Physiology or Human “love to knowledge” (from Bulgarian “lyuboz- Medicine. For the discovery of a new cell world, revealing nanie” - “lyubov”, love, “znanie”, knowledge) led to the membrane-bound organelles (mitochondria, endoplasmic re- whish to “see inside” the body of organisms. Initially, this ticulum, Golgi complex, lysosomes, caveolae) and cytoskel- was achieved by the dissection of human cadavers performed etal elements (filaments and microtubules). by the pioneer anatomist Andreas Vesalius. Later on the mi- The plasma membrane (plasmalemma, cell surface) is a croscope was invented. In 1609, Galileo was among the first complex lipoprotein structure surrounding the cells in all to use a telescope as an instrument to observe stars and plan- living organisms. Cells have constant need for the build- ets. The names „telescope“ and „microscope“ were coined for ing components of life: amino acids, lipids, carbohydrates, Galileo‘s instrument, in 1611. Illustrations of insects made and nucleic acids. -

Cell Secretion and Membrane Fusion: Highly Significant Phenomena in the Life of a Cell
DISCOVERIES 2014, Jul -Sep, 2(3): e30 DOI: 10.15190/d.2014.22 Cell Secretion and Membrane Fusion EDITORIAL Cell secretion and membrane fusion: highly significant phenomena in the life of a cell Mircea Leabu 1,2,3,*, Garth L. Nicolson 4,* 1University of Medicine and Pharmacy “Carol Davila”, Department of Cellular and Molecular Medicine, 8, Eroilor Sanitari Blvd., 050474, Bucharest, Romania 2 “Victor Babes” National Institute of Pathology, 99101, Splaiul Independentei, 050096, Bucharest, Romania 3University of Bucharest, Research Center for Applied Ethics, 204, Splaiul Independentei, 060024, Bucharest, Romania 4Department of Molecular Pathology, Institute for Molecular Medicine, Huntington Beach, California, 92647 USA *Corresponding authors: Mircea Leabu, PhD , “Victor Babes” National Institute of Pathology, 99-101, Splaiul Independentei, 050096, Bucharest, Romania; E-mail: [email protected]; Garth L. Nicolson, Ph.D , The Institute for Molecular Medicine, P.O. Box 9355, S. Laguna Beach, CA 92652 USA. Email: [email protected] Submitted: Sept. 10, 2014; Revised: Sept. 14, 2014; Accepted: Sept. 17, 2014; Published: Sept. 18, 2014; Citation : Leabu M, Nicolson GL. Cell Secretion and membrane fusion: highly significant phenomena in the life of a cell. Discoveries 2014, Jul-Sep; 2(3): e30. DOI: 10.15190/d.2014.22 Keywords : cell secretion, membrane fusion, every cell’s existence, and they must be very well porosome, exosomes, electron microscopy, cancer, coordinated and controlled. Membrane trafficking, mathematical approach, secretory vesicle, science which involves vesicular budding of the source history membrane, directed transport and eventually fusion with the target membrane is a very specific process. All of these processes depend, in particular, on Introduction basic principals of biological membrane structure Is there any cell that does not secrete something and dynamics, a topic that was reviewed recently in necessary for maintenance of the organism? this journal 1. -

Ams 3 2009.Qxp
Review paper Cholesterol-lowering therapy and cell membranes. Stable plaque at the expense of unstable membranes? Glyn Wainwright1, Luca Mascitelli2, Mark R. Goldstein3 1Independent Reader of Research, Leeds, United Kingdom Corresponding author: 2Medical Service, Comando Brigata Alpina “Julia”, Udine, Italy Luca Mascitelli, MD 3Fountain Medical Court, Bonita Springs, FL, USA Comando Brigata Alpina “Julia” Medical Service Submitted: 15 April 2009 8 Via S. Agostino Accepted: 4 May 2009 Udine 33100, Italy Phone: +39 0432584044 Arch Med Sci 2009; 5, 3: 289-295 Fax: +390432584053 Copyright © 2009 Termedia & Banach E-mail: [email protected] Abstract Current guidelines encourage ambitious long term cholesterol lowering with statins, in order to decrease cardiovascular disease events. However, by regulating the biosynthesis of cholesterol we potentially change the form and function of every cell membrane from the head to the toe. As research into cell morphology and membrane function realises more dependencies upon cholesterol rich lipid membranes, our clinical understanding of long term inhibition of cholesterol biosynthesis is also changing. This review of non- cardiovascular research concerning such membrane effects raises important new issues concerning the clinical advantages and disadvantages of the long term use, and broadening criteria, of cholesterol reductions. Key words: cholesterol, exocytosis, lipid, membrane, statin. Introduction The undoubted commercial success story in modern medicine has been the creation of that infamous household dietary and medical obsession: ‘Cholesterol’. Over the past decade researchers have achieved new insight into the regulatory relationship between cholesterol and the world of lipid transport. A persuasive association of statistics about cardiovascular outcomes and levels of blood plasma lipids has created a sophisticated range of therapeutic targets for cholesterol lowering therapies [1]. -
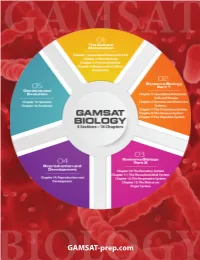
BIOLOGYGAMSAT-Prep.Com
GAMSAT C M Y CM MY CY CMY K BIOLOGYGAMSAT-prep.com GENERALISED EUKARYOTIC CELL Chapter 1 Memorise Understand Importance * Structure/function: cell/components * 1st year university level info* High level: 15% of GAMSAT Biology * Components and function: cytoskeleton * Membrane transport questions released by ACER are related to * DNA structure and function * Hyper/hypotonic solutions content in this chapter (in our estimation). * Transmission of genetic information * Saturation kinetics: graphs * Note that approximately of the * Mitosis, events of the cell cycle * Unique features of eukaryotes 75% questions in GAMSAT Biology are related * Basics: Cell junctions, microscopy to just 7 chapters: 1, 2, 3, 4, 7, 12, and 15. Introduction Cells are the basic organisational unit of living organisms. They are contained by a plasma membrane and/or cell wall. Eukaryotic cells (eu = true; karyote refers to nucleus) are cells with a true nucleus found in all multicel- lular and nonbacterial unicellular organisms including animal, fungal and plant cells. The nucleus contains ge- netic information, DNA, which can divide into 2 cells by mitosis. Get ready to waste some time! Glad to have your attention! Our experience is that most students ‘overstudy’ Biol- ogy and underperform in Biology when they see the types of questions that are asked on the GAMSAT. Please do not get trapped in details. We’ll guide you as much as we can but in the end, it’s up to you: colour-coded table of contents, yellow highlighter, underline, foundational and GAMSAT-level practice questions at the end of the chapter, etc. For now, enjoy the story that you are expected to be exposed to for the GAMSAT, but generally the content will likely be more helpful to you in medical school. -

Reconstituted Fusion Pore
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biophysical Journal Volume 85 September 2003 2035–2043 2035 Reconstituted Fusion Pore Aleksandar Jeremic,* Marie Kelly,* Sang-Joon Cho,* Marvin H. Stromer,y and Bhanu P. Jena* *Department of Physiology, Wayne State University School of Medicine, Detroit, Michigan 48201; and yDepartment of Animal Science, Biochemistry, Biophysics, and Molecular Biology, Iowa State University, Ames, Iowa 50011 ABSTRACT Fusion pores or porosomes are basket-like structures at the cell plasma membrane, at the base of which, membrane-bound secretory vesicles dock and fuse to release vesicular contents. Earlier studies using atomic force microscopy (AFM) demonstrated the presence of fusion pores at the cell plasma membrane in a number of live secretory cells, revealing their morphology and dynamics at nm resolution and in real time. ImmunoAFM studies demonstrated the release of vesicular contents through the pores. Transmission electron microscopy (TEM) further confirmed the presence of fusion pores, and immunoAFM, and immunochemical studies demonstrated t-SNAREs to localize at the base of the fusion pore. In the present study, the morphology, function, and composition of the immunoisolated fusion pore was investigated. TEM studies reveal in further detail the structure of the fusion pore. Immunoblot analysis of the immunoisolated fusion pore reveals the presence of several isoforms of the proteins, identified earlier in addition to the association of chloride channels. TEM and AFM micrographs of the immunoisolated fusion pore complex were superimposable, revealing its detail structure. Fusion pore reconstituted into liposomes and examined by TEM, revealed a cup-shaped basket-like morphology, and were functional, as demonstrated by their ability to fuse with isolated secretory vesicles. -

Gaspar Banfalvi.Pdf
Gaspar Banfalvi Permeability of Biological Membranes Permeability of Biological Membranes Gaspar Banfalvi Permeability of Biological Membranes Gaspar Banfalvi University of Debrecen Debrecen , Hungary ISBN 978-3-319-28096-7 ISBN 978-3-319-28098-1 (eBook) DOI 10.1007/978-3-319-28098-1 Library of Congress Control Number: 2016932313 © Springer International Publishing Switzerland 2016 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. Printed on acid-free paper This Springer imprint is published by SpringerNature The registered company is Springer International Publishing AG Switzerland. Summ ary The ultimate energy source for life on Earth is the solar energy of Sun. -

REVIEW Fusion Pore Or Porosome
169 REVIEW Fusion pore or porosome: structure and dynamics B P Jena Department of Physiology, Wayne State University School of Medicine, 5239 Scott Hall, 540 E. Canfield Avenue, Detroit, Michigan 48201–4177, USA (Requests for offprints should be addressed toBPJena; Email: [email protected]) Abstract Electrophysiological measurements on live secretory cells microscopy on live exocrine and neuroendocrine cells almost a decade ago suggested the presence of fusion pores demonstrate the presence of such plasma membrane pores, at the cell plasma membrane. Membrane-bound secretory revealing their morphology and dynamics at near nm vesicles were hypothesized to dock and fuse at these sites, resolution and in real time. to release their contents. Our studies using atomic force Journal of Endocrinology (2003) 176, 169–174 Introduction pattern using a xyz piezo tube to scan the surface of the sample (Fig. 1) (Binnig et al. 1986). The deflection of the Hormone release, neurotransmission, and enzyme secre- cantilever measured optically is used to generate an tion are fundamental physiological processes resulting from isoforce relief of the sample (Alexander et al. 1989). Force the fusion of membrane-bound secretory vesicles at the is thus used to image surface profiles of objects by the cell plasma membrane and consequent expulsion of ves- AFM, allowing imaging of live cells and subcellular icular contents. Membrane-bound secretory vesicles dock structures submerged in physiological buffer solutions. To and fuse at specific plasma membrane locations following image live cells, the scanning probe of the AFM operates secretory stimulus. Earlier electrophysiological studies sug- in physiological or near physiological buffers, and may do gested the existence of ‘fusion pores’ at the cell plasma so under two modes: contact or tapping. -

C. Elegans Intestinal Cells
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Science and Technology 1571 Systemic RNAi Relies on the Endomembrane System in Caenorhabditis elegans YANI ZHAO ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6214 ISBN 978-91-513-0093-1 UPPSALA urn:nbn:se:uu:diva-330894 2017 Dissertation presented at Uppsala University to be publicly examined in B42, Uppsala Biomedical central, Husagatan 3, Uppsala, Thursday, 23 November 2017 at 13:00 for the degree of Doctor of Philosophy. The examination will be conducted in English. Faculty examiner: Professor Simon Tuck (Centre for Molecular Medicine, Umeå University). Abstract Zhao, Y. 2017. Systemic RNAi Relies on the Endomembrane System in Caenorhabditis elegans. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Science and Technology 1571. 60 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-513-0093-1. The membrane system of a eukaryotic cell is a large and complex system handling the transport, exchange and degradation of many kinds of material. Recent research shows that double- stranded RNA (dsRNA) mediated gene silencing (RNA interference) is a membrane related process. After long dsRNA is processed to small interfering RNA (siRNA) by Dicer, the guide strand and passenger strand are separated in the RNA induced silencing complex (RISC) by Argonaute. The process of loading siRNA into RISC has been suggested to occur at the rough Endoplasmic Reticulum (rER).The components of RISC also associate with late endosomes/ multivesicular bodies -

Porosome: the Universal Molecular Machinery for Cell Secretion
Mol. Cells OS, 517-529, December 31, 2008 Molecules Minireview and Cells ©2008 KSMCB Porosome: the Universal Molecular Machinery for Cell Secretion Bhanu P. Jena* Porosomes are supramolecular, lipoprotein structures at vesicles following secretion. The journey leading to the discov- the cell plasma membrane, where membrane-bound secre- ery of the ‘éçêçëçãÉ’, a nanometer-size structure at the cell tory vesicles transiently dock and fuse to release inrave- plasma membrane -the universal secretory machinery, and its sicular contents to the outside during cell secretion. The structure, function, isolation, chemistry, and reconstitution into mouth of the porosome opening to the outside, range in lipid membrane, the molecular mechanism of secretory vesicle size from 150 nm in diameter in acinar cells of the exocrine swelling and fusion at the base of porosomes, is discussed. pancreas, to 12 nm in neurons, which dilates during cell The isolation of the porosome, and the determination of its secretion, returning to its resting size following completion biochemical composition, its structure and dynamics at nm of the process. In the past decade, the composition of the resolution and in real time, and its functional reconstitution into porosome, its structure and dynamics at nm resolution architecture lipid membrane (Cho et al., 2002a; 2002b; 2004; and in real time, and its functional reconstitution into artifi- 2007; Jena, 2005; 2007; Jena et al., 2003; Jeremic et al., 2003; cial lipid membrane, have all been elucidated. In this mini Schneider et al., 1997), has greatly advanced our understand- review, the discovery of the porosome, its structure, func- ing of the secretory process in cells. -

THÈSE L’Obtention De Du Strasbourg Grade De
ÉcoleU DoctoraleNIVERSITÉ des Sciences DE STRASBOURG de la Vie et de la Santé INCI – CNRS UPR 3212 DocteurPrésentée de Pour l’UniversitéTHÈSE l’obtention de du Strasbourg grade de : Discipline : Sciences du Vivant Spécialité : Aspects moléculaires et cellulaires de la biologie Q ili P WANGar Interaction entre la sous unité V0 de la V-ATPase et le facteur d'échange ARNO et son implication fonctionnelle dans l'exocytose régulée SoutenueDr. SIMONNEAUX mecredi le Valérie 18 septembre 2019 , devant Présidente le jury compos du juré dey : Dr. EL FAR Oussama Rapporteur externe Pr. OLIVIER Jean-Luc Rapporteur externe Dr. VITALE Nicolas Directeur de thèse Remerciements Dr. SIMONNEAUX JeValérie souhaiterais, Dr. EL toutFAR d’abordOussama remercier et Pr. OLIVIER les membres Jean de-Luc mon jury de thèse, , qui m’ont fait le grand honneur d’avoir accepté de lire, commenter et juger mon travail de thèse. Dr. VITALE Nicolas Je voudrais également remercier mon directeur de thèse . Tu m’as encadré pendant 4 ans et tu m’as suivi pas a pas dans mon apprentissage de la recherche avec tes qualités scientifiques et humaines. Je veux bien profiter de cette occasion pour t’exprimer mes sincères remerciements pour ta confiance et les libértés que tu m’as données dans la recherche. Merci pour tout. MesDr. Marieremerciements France vontBADER également à tous les membres de l’équipe pour leur aide : , pour m’avoir accueillie à l’INCI alors qu’elle en était la directrice.Dr. Stéphane GASMAN , co-responsable de l’équipe, pour tes remarques constructives et saDr. bonne Stéphane humeur ORY. -

Molecules 2011, 16, 3618-3635; Doi:10.3390/Molecules16053618
Molecules 2011, 16, 3618-3635; doi:10.3390/molecules16053618 OPEN ACCESS molecules ISSN 1420-3049 www.mdpi.com/journal/molecules Review Molecular Morphology of Pituitary Cells, from Conventional Immunohistochemistry to Fluorescence Imaging Akira Matsuno 1,*, Akiko Mizutani 1,2, Hiroko Okinaga 2, Koji Takano 3, So Yamada 1, Shoko M. Yamada 1, Hiroshi Nakaguchi 1, Katsumi Hoya 1, Mineko Murakami 1, Masato Takeuchi 4, Mutsumi Sugaya 4, Johbu Itoh 5, Susumu Takekoshi 6 and R. Yoshiyuki Osamura 7 1 Department of Neurosurgery, Teikyo University Chiba Medical Center, Chiba 299-0111, Japan; E-Mails: [email protected] (A.M.); [email protected] (S.Y.); [email protected] (S.M.Y.); [email protected] (H.N.); [email protected] (K.H.); [email protected] (M.M.) 2 Teikyo Heisei University, Tokyo 170-8445, Japan; E-Mail: [email protected] 3 Department of Nephrology and Endocrinology, University of Tokyo Hospital, Tokyo 113-0033, Japan; E-Mail: [email protected] 4 Department of Rehabilitation, Teikyo University Chiba Medical Center, Chiba 299-0111, Japan; E-Mails: [email protected] (M.T.); [email protected] 5 Teaching and Research Support Center, Tokai University School of Medicine, Kanagawa 259-1100, Japan; E-Mail: [email protected] 6 Department of Pathology, Tokai University School of Medicine, Kanagawa 259-1100, Japan; E-Mail: [email protected] 7 Pathology Diagnosis Center, International University of Health and Welfare, Tokyo 108-8329, Japan; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +81-436-62-1211; Fax: +81-436-62-1357. -

Cell Secretion: Current Structural and Biochemical Insights
Review TheScientificWorldJOURNAL (2010) 10, 2054–2069 ISSN 1537-744X; DOI 10.1100/tsw.2010.193 Cell Secretion: Current Structural and Biochemical Insights Saurabh Trikha, Elizabeth C. Lee, and Aleksandar M. Jeremic* Department of Biological Sciences, The George Washington University, Washington, D.C. E-mail: [email protected]; [email protected]; [email protected] Received April 8, 2010; Revised July 20, 2010, Accepted September 21, 2010; Published October 12, 2010 Essential physiological functions in eukaryotic cells, such as release of hormones and digestive enzymes, neurotransmission, and intercellular signaling, are all achieved by cell secretion. In regulated (calcium-dependent) secretion, membrane-bound secretory vesicles dock and transiently fuse with specialized, permanent, plasma membrane structures, called porosomes or fusion pores. Porosomes are supramolecular, cup- shaped lipoprotein structures at the cell plasma membrane that mediate and control the release of vesicle cargo to the outside of the cell. The sizes of porosomes range from 150 nm in diameter in acinar cells of the exocrine pancreas to 12 nm in neurons. In recent years, significant progress has been made in our understanding of the porosome and the cellular activities required for cell secretion, such as membrane fusion and swelling of secretory vesicles. The discovery of the porosome complex and the molecular mechanism of cell secretion are summarized in this article. KEYWORDS: fusion pore-porosome, soluble N-ethylmaleimide-sensitive factor (NSF)- attachment