Cardiovascular Effects of Marijuana and Synthetic Cannabinoids: the Good, the Bad, and the Ugly
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Targeting the Endocannabinoid System to Reduce Nociception
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2011 Targeting the endocannabinoid system to reduce nociception Lamont Booker Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Medical Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2419 This Dissertation is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. Targeting the Endocannabinoid System to Reduce Nociception A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy at Virginia Commonwealth University. By Lamont Booker Bachelor’s of Science, Fayetteville State University 2003 Master’s of Toxicology, North Carolina State University 2005 Director: Dr. Aron H. Lichtman, Professor, Pharmacology & Toxicology Virginia Commonwealth University Richmond, Virginia April 2011 Acknowledgements The author wishes to thank several people. I like to thank my advisor Dr. Aron Lichtman for taking a chance and allowing me to work under his guidance. He has been a great influence not only with project and research direction, but as an excellent example of what a mentor should be (always willing to listen, understanding the needs of each student/technician, and willing to provide a hand when available). Additionally, I like to thank all of my committee members (Drs. Galya Abdrakmanova, Francine Cabral, Sandra Welch, Mike Grotewiel) for your patience and willingness to participate as a member. Our term together has truly been memorable! I owe a special thanks to Sheryol Cox, and Dr. -

Marijuana: Drug of Abuse Or Therapeutic Option? Learning Objectives
Handout for the Neuroscience Education Institute (NEI) online activity: Marijuana: Drug of Abuse or Therapeutic Option? Learning Objectives • Explain how cannabinoids affect the body and the brain • Educate patients about: – Evidence of efficacy for mental health and other conditions – Potential risks of cannabis use Timeline 1989? 90?: Discovery of ~2000 BC: binding site 2015: Elimination of Chinese 1943: Marijuana for THC— 1992: US Public Health emperors removed from CB1 Endogenous Service oversight cannabinoid recommend listing as a 1963: 1964: THC receptor for obtaining anandamide marijuana as medication in US Cannabidiol isolated marijuana for discovered medicine Pharmacopeia isolated research purposes 1995: 1851: Marijuana 1961: United 1970: Marijuana is Endogenous Aug 11 2016: listed as a Nations Single labeled Schedule I cannabinoid 2-AG DEA declines to medication in US Convention on by the US discovered reschedule Pharmacopeia Narcotic Drugs: Substance Abuse marijuana marijuana said to Act; this restricts be dangerous with both personal use no medical value and access for research purposes THE INTERSECTION OF THE HEALTHCARE AND CANNABIS INDUSTRIES What is Cannabis? 500 chemicals 100 cannabinoids Best understood: THC and CBD Scheduling of Controlled Substances No medicinal value, high Moderate to Lower High potential Low potential potential for low potential potential for for abuse for abuse abuse for abuse abuse Schedule I Schedule II Schedule III Schedule IV Schedule V Marijuana Cocaine Tylenol w/ Tramadol Robitussin AC Heroin -

Cannabinoid As Potential Aromatase Inhibitor Through Molecular Modeling and Screening for Anti-Cancer Activity
Cannabinoid as Potential Aromatase Inhibitor Through Molecular Modeling and Screening for Anti-Cancer Activity Sudipta Baroi1, Achintya Saha2, Ritesh Bachar3 and Sitesh C Bachar4 1Department of Pharmaceutical Technology, Faculty of Pharmacy, University of Dhaka Dhaka-1000, Bangladesh 2Department of Chemical Technology, Pharmaceutical & Fine Chemical Technology Division University of Calcutta, India 3Department of Pharmacy, School of Science and Engineering, University of Information Technology and Sciences (UITS), Dhaka-1212, Bangladesh 4Department of Pharmacy, Faculty of Pharmacy, University of Dhaka, Dhaka-1000, Bangladesh (Received: April 15, 2020; Accepted: June 2, 2020; Published (web): June 28, 2020) ABSTRACT: Inhibition of aromatase (CYTP450), a key enzyme in the estrogen biosynthesis, could result in regression of estrogen-dependent tumors and even prevent the promotion of breast cancer. The present research has been designed for searching a potent chemical moiety from natural sources to inhibit aromatase enzyme, the over- functionality of which causes the breast cancer. Cannabis sativa contains a very much promising group of cannabinoids with more than 66 compounds with reported anticancer property and for the search of a target specific potent aromatase inhibitor, 61 cannabinoids from C. sativa were selected. The Structures Data File (SDF) of these ligand molecules were subjected to docking studies at the binding site of aromatase X-ray crystallographic structure based on lower resolution of the protein crystal structure and higher docking accuracy, predicted by calculating the correlation between experimental activities and Glide dock scores and compared with the standard aromatase ligand androstenedione and aromatase inhibitor fadrozole with existing drug for breast cancer treatment. The best docked pose of each ligand was selected on the basis of the highest dock score related to the binding free energies of the internal dataset compounds as compared to their observed activities. -

Cannabinoid Receptor and Inflammation
Cannabinoid Receptor and Inflammation Newman Osafo1, Oduro Yeboah1, Aaron Antwi1, and George Ainooson1 1Kwame Nkrumah University of Science and Technology September 11, 2020 Abstract The eventual discovery of endogenous cannabinoid receptors CB1 and CB2 and their endogenous ligands has generated interest with regards to finally understanding the endocannabinoid system. Its role in the normal physiology of the body and its implication in pathological states such as cardiovascular diseases, neoplasm, depression and pain have been subjects of scientific interest. In this review the authors focus on the endogenous cannabinoid pathway, the critical role of cannabinoid receptors in signaling and mediation of neurodegeneration and other inflammatory responses as well as its potential as a drug target in the amelioration of some inflammatory conditions. Though the exact role of the endocannabinoid system is not fully understood, the evidence found leans heavily towards a great potential in exploiting both its central and peripheral pathways in disease management. Cannabinoid therapy has already shown great promise in several preclinical and clinical trials. 1.0 Introduction Ethnopharmacological studies have shown the use of Cannabis sativa in traditional medicine for over a thousand years, with its widespread use promoted by its psychotropic effects (McCoy, 2016; Turcotte et al., 2016). The discovery of a receptor within human body, that is selectively activated by cannabinoids suggested the presence of at least one endogenous ligand for this receptor. This is confirmed by the discovery of two endogenously synthesized lipid mediators, 2-arachidonoyl-glycerol and arachidonoylethanolamide, which function as high-affinity ligands for a subfamily of cannabinoid receptors ubiquitously distributed in the central nervous system, known as the CB1 receptors (Turcotte et al., 2016). -

) (51) International Patent Classification: Columbia V5G 1G3
) ( (51) International Patent Classification: Columbia V5G 1G3 (CA). PANDEY, Nihar R.; 10209 A 61K 31/4525 (2006.01) C07C 39/23 (2006.01) 128A St, Surrey, British Columbia V3T 3E7 (CA). A61K 31/05 (2006.01) C07D 405/06 (2006.01) (74) Agent: ZIESCHE, Sonia et al.; Gowling WLG (Canada) A61P25/22 (2006.01) LLP, 2300 - 550 Burrard Street, Vancouver, British Colum¬ (21) International Application Number: bia V6C 2B5 (CA). PCT/CA2020/050165 (81) Designated States (unless otherwise indicated, for every (22) International Filing Date: kind of national protection av ailable) . AE, AG, AL, AM, 07 February 2020 (07.02.2020) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, (25) Filing Language: English DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, (26) Publication Language: English HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (30) Priority Data: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, 16/270,389 07 February 2019 (07.02.2019) US OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (63) Related by continuation (CON) or continuation-in-part SC, SD, SE, SG, SK, SL, ST, SV, SY, TH, TJ, TM, TN, TR, (CIP) to earlier application: TT, TZ, UA, UG, US, UZ, VC, VN, WS, ZA, ZM, ZW. US 16/270,389 (CON) (84) Designated States (unless otherwise indicated, for every Filed on 07 Februaiy 2019 (07.02.2019) kind of regional protection available) . -

NIDA's Drug Facts on Synthetic Cannabinoids (K2/Spice)
Synthetic Cannabinoids (K2/Spice) Revised February 2018 What are synthetic cannabinoids? Synthetic cannabinoids are human-made mind-altering chemicals that are either sprayed on dried, shredded plant material so they can be smoked or sold as liquids to be vaporized and inhaled in e-cigarettes and other devices. These products are also known as herbal or liquid incense. These chemicals are called cannabinoids because they are similar to chemicals found in the marijuana plant. Because of this similarity, synthetic cannabinoids are sometimes misleadingly called "synthetic marijuana" (or "fake weed"), and they are often marketed as safe, legal alternatives to that drug. In fact, they are not safe and may affect the brain much more powerfully than marijuana; their actual effects can be unpredictable and, in some cases, more dangerous or even life-threatening. Synthetic cannabinoids are part of a group of drugs called new psychoactive substances (NPS). NPS are unregulated mind-altering substances that have become newly available on the market and are intended to produce the same effects as illegal drugs. Some of these substances may have been around for years but have reentered the market in altered chemical forms, or due to renewed popularity. False Advertising Synthetic cannabinoid products are often labeled "not for human consumption." Labels also often claim that they contain "natural" material taken from a variety of plants. However, the only parts of these products that are natural are the dried plant materials. Chemical tests show that the active, mind-altering ingredients are cannabinoid compounds made in laboratories. Synthetic Cannabinoids • February 2018 • Page 1 Manufacturers sell these products in colorful foil packages and plastic bottles to attract consumers. -
Recommended Methods for the Identification and Analysis of Synthetic Cannabinoid Receptor Agonists in Seized Materials (Revised and Updated)
Recommended methods for the Identification and Analysis of Synthetic Cannabinoid Receptor Agonists in Seized Materials (Revised and updated) MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Photo credits: UNODC Photo Library; UNODC/Ioulia Kondratovitch; Alessandro Scotti. Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Synthetic Cannabinoid Receptor Agonists in Seized Materials (Revised and updated) MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2020 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases, but any modification has to be validated before it is integrated into laboratory routines. Mention of names of firms and commercial products does not imply theendorsement of the United Nations. ST/NAR/48/REV.1 © United Nations, July 2020. All rights reserved, worldwide The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Services of the United Nations Office on Drugs and Crime (UNODC) (LSS, headed by Dr. -

Frequently Asked Questions About Synthetic Drugs
FREQUENTLY ASKED QUESTIONS ABOUT SYNTHETIC DRUGS WHAT ARE SYNTHETIC DRUGS? WHAT DOES THE PACKAGING OF SYNTHETIC CANNABINOIDS LOOK LIKE? A SYNTHETIC DRUG, ALSO REFERRED TO AS A Many of the products are sold in colorful packets with names DESIGNER DRUG, IS A CHEMICAL INTENDED TO that appeal to adolescents and young adults. Manufacturers IMITATE THE PROPERTIES AND EFFECTS OF A label the packages as “not for human consumption” and KNOWN HALLUCINOGEN OR NARCOTIC AND market the products as incense or potpourri to mask the MAY HAVE UNKNOWN SIDE EFFECTS OR CAUSE intended purpose and to avoid regulatory oversight of AN ADVERSE REACTION. THESE DRUGS ARE the manufacturing process. You can view examples of the packaging on page 3. CREATED IN ORDER TO EVADE RESTRICTIONS AGAINST ILLEGAL SUBSTANCES. ARE SYNTHETIC CANNABINOIDS ARE SYNTHETIC DRUGS LEGAL IN TEXAS? DANGEROUS? No. Under state law, it is a crime to manufacture, deliver or Synthetic cannabinoids possess a synthetic drug. are illegal, dangerous, highly addictive and WHAT ARE SYNTHETIC CANNABINOIDS? potentially deadly. One Synthetic cannabinoids are commonly referred to as K2, of the original chemists Kush, Spice, synthetic marijuana and fake weed. They are who designed synthetic a mix of plant matter sprayed with chemicals in sometimes cannabis for research purposes, John Huffman, Ph.D., likened dangerously high proportions, falsely marketed as “legal recreational use of synthetic drugs to playing Russian highs” and smoked like marijuana. roulette. The contents and effects of synthetic cannabinoids WHERE ARE SYNTHETIC CANNABINOIDS SOLD? are unpredictable due to a constantly changing variety of Synthetic cannabinoids are relatively inexpensive and sold chemicals used in manufacturing processes devoid of quality in convenience stores, smoke shops, novelty stores, on the controls and government regulatory oversight. -

Potential Cannabis Antagonists for Marijuana Intoxication
Central Journal of Pharmacology & Clinical Toxicology Bringing Excellence in Open Access Review Article *Corresponding author Matthew Kagan, M.D., Cedars-Sinai Medical Center, 8730 Alden Drive, Los Angeles, CA 90048, USA, Tel: 310- Potential Cannabis Antagonists 423-3465; Fax: 310.423.8397; Email: Matthew.Kagan@ cshs.org Submitted: 11 October 2018 for Marijuana Intoxication Accepted: 23 October 2018 William W. Ishak, Jonathan Dang, Steven Clevenger, Shaina Published: 25 October 2018 Ganjian, Samantha Cohen, and Matthew Kagan* ISSN: 2333-7079 Cedars-Sinai Medical Center, USA Copyright © 2018 Kagan et al. Abstract OPEN ACCESS Keywords Cannabis use is on the rise leading to the need to address the medical, psychosocial, • Cannabis and economic effects of cannabis intoxication. While effective agents have not yet been • Cannabinoids implemented for the treatment of acute marijuana intoxication, a number of compounds • Antagonist continue to hold promise for treatment of cannabinoid intoxication. Potential therapeutic • Marijuana agents are reviewed with advantages and side effects. Three agents appear to merit • Intoxication further inquiry; most notably Cannabidiol with some evidence of antipsychotic activity • THC and in addition Virodhamine and Tetrahydrocannabivarin with a similar mixed receptor profile. Given the results of this research, continued development of agents acting on cannabinoid receptors with and without peripheral selectivity may lead to an effective treatment for acute cannabinoid intoxication. Much work still remains to develop strategies that will interrupt and reverse the effects of acute marijuana intoxication. ABBREVIATIONS Therapeutic uses of cannabis include chronic pain, loss of appetite, spasticity, and chemotherapy-associated nausea and CBD: Cannabidiol; CBG: Cannabigerol; THCV: vomiting [8]. Recreational cannabis use is on the rise with more Tetrahydrocannabivarin; THC: Tetrahydrocannabinol states approving its use and it is viewed as no different from INTRODUCTION recreational use of alcohol or tobacco [9]. -

Cannabinoid Interventions for PTSD: Where to Next?
Accepted Manuscript Cannabinoid interventions for PTSD: Where to next? Luke Ney, Allison Matthews, Raimondo Bruno, Kim Felmingham PII: S0278-5846(19)30034-X DOI: https://doi.org/10.1016/j.pnpbp.2019.03.017 Reference: PNP 9622 To appear in: Progress in Neuropsychopharmacology & Biological Psychiatry Received date: 14 January 2019 Revised date: 20 March 2019 Accepted date: 29 March 2019 Please cite this article as: L. Ney, A. Matthews, R. Bruno, et al., Cannabinoid interventions for PTSD: Where to next?, Progress in Neuropsychopharmacology & Biological Psychiatry, https://doi.org/10.1016/j.pnpbp.2019.03.017 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. ACCEPTED MANUSCRIPT 1 Cannabinoid interventions for PTSD: Where to next? Luke Ney1, Allison Matthews1, Raimondo Bruno1 and Kim Felmingham2 1School of Psychology, University of Tasmania, Australia 2School of Psychological Sciences, University of Melbourne, Australia ACCEPTED MANUSCRIPT ACCEPTED MANUSCRIPT 2 Abstract Cannabinoids are a promising method for pharmacological treatment of post- traumatic stress disorder (PTSD). Despite considerable research devoted to the effect of cannabinoid modulation on PTSD symptomology, there is not a currently agreed way by which the cannabinoid system should be targeted in humans. In this review, we present an overview of recent research identifying neurological pathways by which different cannabinoid-based treatments may exert their effects on PTSD symptomology. -
Synthetic Cannabinoids (60 Substances) A) Classical Cannabinoid
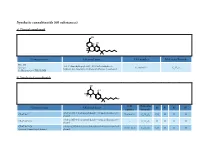
Synthetic cannabinoids (60 substances) a) Classical cannabinoid OH H OH H O Common name Chemical name CAS number Molecular Formula HU-210 3-(1,1’-dimethylheptyl)-6aR,7,10,10aR-tetrahydro-1- Synonym: 112830-95-2 C H O hydroxy-6,6-dimethyl-6H-dibenzo[b,d]pyran-9-methanol 25 38 3 11-Hydroxy-Δ-8-THC-DMH b) Nonclassical cannabinoids OH OH R2 R3 R4 R1 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyloctan- 2- yl) CP-47,497 70434-82-1 C H O CH H H H phenol 21 34 2 3 rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylheptan- 2- yl) CP-47,497-C6 - C H O H H H H phenol 20 32 2 CP-47,497-C8 rel-2- [(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylnonan- 2- yl) 70434-92-3 C H O C H H H H Synonym: Cannabicyclohexanol phenol 22 36 2 2 5 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyldecan- 2- yl) CP-47,497-C9 - C H O C H H H H phenol 23 38 2 3 7 rel-2- ((1 R,2 R,5 R)-5- hydroxy- 2- (3- hydroxypropyl)cyclohexyl)- 3-hydroxy CP-55,940 83003-12-7 C H O CH H H 5-(2- methyloctan- 2- yl)phenol 24 40 3 3 propyl rel-2- [(1 S,3 R)-3- hydroxy-5,5-dimethylcyclohexyl]- 5- (2- Dimethyl CP-47,497-C8 - C H O C H CH CH H methylnonan-2- yl)phenol 24 40 2 2 5 3 3 c) Aminoalkylindoles i) Naphthoylindoles 1' R R3' R2' O N CAS Molecular Common name Chemical name R1’ R2’ R3’ number Formula [1-[(1- methyl- 2- piperidinyl)methyl]- 1 H-indol- 3- yl]- 1- 1-methyl-2- AM-1220 137642-54-7 C H N O H H naphthalenyl-methanone 26 26 2 piperidinyl -

Endocannabinoid System: the Direct and Indirect Involvement in the Memory and Learning Processes—A Short Review
Mol Neurobiol DOI 10.1007/s12035-016-0313-5 Endocannabinoid System: the Direct and Indirect Involvement in the Memory and Learning Processes—a Short Review Marta Kruk-Slomka1 & Agnieszka Dzik1 & Barbara Budzynska1 & Grazyna Biala1 Received: 30 September 2016 /Accepted: 21 November 2016 # The Author(s) 2016. This article is published with open access at Springerlink.com Abstract The endocannabinoid system via cannabinoid Ca 2+ Calcium ions (CB: CB1 and CB2) receptors and their endogenous ligands CB Cannabinoid is directly and indirectly involved in many physiological func- CB1KOS CB1 receptor genetic knockout mice tions, especially in memory and learning processes. Extensive CB2KOS CB2 receptor genetic knockout mice studies reported that this system strictly modulates cognition- CFC Contextual fear conditioning related processes evaluated in various animal models. CNS Central nervous system However, the effects of cannabinoids on the cognition have ECS Endocannabinoid system been contradictory. The cannabinoid compounds were able to ETM Elevated T-maze both impair or improve different phases of memory processes FAAH Fattyacidamidhydrolase through direct (receptor related) or indirect (non-receptor GABA Gamma-aminobutyric acid related) mechanism. The memory-related effects induced by IA Inhibitory avoidance the cannabinoids can be depended on the kind of cannabinoid Intra-BLA Intra-basolateral amygdala compound used, dosage, and route of administration as well as Intra-PLC Intra-prelimbic on the memory task chosen. Therefore, the objectives of this i.p. Intra-peritoneally paper are to review and summarize the results describing the MAGL Monoacylglycerol lipase role of endocannabinoid system in cognition, including NADA N-arachidonoyl dopamine various stages of memory. NAGly N-arachidonylglycine OEA Oleoylethanolamine Keywords Endocannabinoid system .