Yangon University of Economics Master of Development Studies Programme
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Projects to Boost Supply of Irrigation Water Maung Maung Myo (Bago)
Established 1914 Volume XVIII, Number 79 13th Waning of First Waso 1372 ME Friday, 9 July, 2010 Four political objectives * Stability of the State, community peace and tranquillity, Golden deer, star turtles handed prevalence of law and order * National reconsolidation * Emergence of a new enduring State Constitution over to ZPO, Thailand * Building of a new modern developed nation in accord with the new State Constitution Four economic objectives * Development of agriculture as the base and all-round develop- NAY P YI T AW, 8 July—A ceremony to handover Chairman of Thai-Myanmar Friendship As- ment of other sectors of the economy as well * Proper evolution of the market-oriented economic system two pairs of golden deer and five pairs of star turtles sociation General Lertrat Ratanavanich spoke words * Development of the economy inviting participation in terms by the Ministry of Forestry to Zoological Park Or- of technical know-how and investments from sources inside of thanks, presented gift to the Minister. Then, those the country and abroad ganization (ZPO, Thailand) took place at Forest present had documentary photo taken. * The initiative to shape the national economy must be kept in the Department (head office), here, today. It was also attended by departmental heads of hands of the State and the national peoples At the ceremony, Minister for Forestry the Enterprises and Departments under the ministry, Four social objectives * Uplift of the morale and morality of the entire nation U Thein Aung made a speech. rector, deputy directors-general, pro-rectors, direc- * Uplift of national prestige and integrity and preserva- After that, acting Director-General U Aye tors, Second Secretary Mr Roongruk Chanprasert tion and safeguarding of cultural heritage and national Myint Maung of Forest Department handed over character from Thai Embassy, Thai delegation members and * Uplift of dynamism of patriotic spirit documents related to the animals to Director-Gen- guests. -

February Chronology 2018
FEBRUARY CHRONOLOGY 2018 Summary of the Current Situation: There are 240 individuals oppressed in Burma due to political activities, 44 political prisoners are serving prison sentences, 75 are awaiting trial inside prison, 121 are awaiting trial outside prison. Picture from Naing Naing Tun Facebook © 2018 Accessed February 2018 FEBRUARY 2018 1 Table of Contents POLITICAL PRISONERS ................................................................................................... 3 . TRIAL…..……………………………………………………………………………………….3 . CHARGES….…………………………………………………………………………………..5 . SENTENCES…………………………………………………………………………………..6 . RELEASES…………………………………………………………………………………......7 RESTRICTIONS ON CIVIL AND POLITICAL RIGHTS ................................................. 8 LEGISLATION AND POLICY DEVELOPMENTS ........................................................ 14 INSTITUTIONAL REFORM………………………………………………………………………...16 REFERENCES……………………………………………………………………………………………18 FEBRUARY 2018 2 POLITICAL PRISONERS . TRIAL VOA/Burmese) (6 February 2017 - Mizzima/Burmese) (6 February 2017 - Eleven/Burmese) (7 February 2017 - The Trial Continues for Journalists, Wa Lone Voice/Burmese) (7 February 2017 - 7 Day and Kyaw Soe Oo Daily/Burmese) (7 February 2017 - At their February 1 hearing, Reuters Irrawaddy/Burmese) (7 February 2018 - Journalists, Wa Lone and Kyaw Soe Oo, Myanmar Times) (7 February 2018 - were denied bail. Arrested in Arakan State Irrawaddy) (13 February 2018 - under the Official Secrets Act, their ongoing Reuters) (14 February 2018 - DVB) (14 trial has -
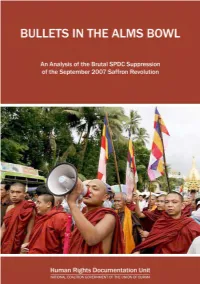
Bullets in the Alms Bowl
BULLETS IN THE ALMS BOWL An Analysis of the Brutal SPDC Suppression of the September 2007 Saffron Revolution March 2008 This report is dedicated to the memory of all those who lost their lives for their part in the September 2007 pro-democracy protests in the struggle for justice and democracy in Burma. May that memory not fade May your death not be in vain May our voices never be silenced Bullets in the Alms Bowl An Analysis of the Brutal SPDC Suppression of the September 2007 Saffron Revolution Written, edited and published by the Human Rights Documentation Unit March 2008 © Copyright March 2008 by the Human Rights Documentation Unit The Human Rights Documentation Unit (HRDU) is indebted to all those who had the courage to not only participate in the September protests, but also to share their stories with us and in doing so made this report possible. The HRDU would like to thank those individuals and organizations who provided us with information and helped to confirm many of the reports that we received. Though we cannot mention many of you by name, we are grateful for your support. The HRDU would also like to thank the Irish Government who funded the publication of this report through its Department of Foreign Affairs. Front Cover: A procession of Buddhist monks marching through downtown Rangoon on 27 September 2007. Despite the peaceful nature of the demonstrations, the SPDC cracked down on protestors with disproportionate lethal force [© EPA]. Rear Cover (clockwise from top): An assembly of Buddhist monks stage a peaceful protest before a police barricade near Shwedagon Pagoda in Rangoon on 26 September 2007 [© Reuters]; Security personnel stepped up security at key locations around Rangoon on 28 September 2007 in preparation for further protests [© Reuters]; A Buddhist monk holding a placard which carried the message on the minds of all protestors, Sangha and civilian alike. -

August Newsletter 2017
AUGUST NEWSLETTER 2017 TRAININGS Human Rights, Human Rights Documentation and Transitional Justice Training in Arakan State and Magwe Division As a part of the series of regular Trainings on Transitional Justice, AAPP held two long Training's in the month of August. A 12-day Training from August 3-14 was organized in Thandwe Town in Arakan State, and an 11-day Training from August 16-26 was held in Salin Township, Magwe Division. In Thandwe Town, Human Rights Trainer Ko Nay Transitional Justice Training in Wun and Human Rights Documentation and Thandwe Township, Arakan State Transitional Justice Trainer Ko Sai Myint Thu led the training. A total of 24 participants attended, including 22 people from Catholic Youth Network and two Catholic monks from Chin, Khume, Karen, HUMAN RIGHTS LECTURES Myo, and Asho backgrounds. Thirty-Five Lectures on Human Rights In Salin Township, the Training's was Provided to Students and Community administered by AAPP’s Human Rights Trainer Ko Saw Than Hlaing and Human Rights In August, the Assistance Association for Political Documentation and Transitional Justice Trainer Prisoners (AAPP_ provided a total of 35 lectures Ko Kyaw Oo. 25 people participated in the in four townships in Bago Division, one township training, including members of the NLD, the Salin in Rangoon Division, 33 lectures in 29 schools in Farmer Group, farmers union, youth organization Pyay, Paungde, Zigon, and Tharyarwaddy and village development groups, from both Chin Townships, one lecture at Phyu Sin A Lin Yaung and Burmese backgrounds. Free Education School in Paungde Township, and one lecture in Htantabin Township in Rangoon The regions faced challenges, so a set of issues Division. -

The 4Th ASEAN Rural Development and Poverty Eradication Leadership Awards: Profiles of the Awardees
The 4 Profiles of the Awardees Profiles th th The 4 ASEAN Rural Development ASEAN Rural Development and Poverty Eradication Leadership Awards: and Poverty Eradication Leadership Awards: Profiles of the Awardees The 4th ASEAN Rural Development and Poverty Eradication The 4th ASEAN Rural Development and Poverty Eradication PB Leadership Awards: Profiles of the Awardees Leadership Awards: Profiles of the Awardees A The 4th ASEAN Rural Development and Poverty Eradication B Leadership Awards: Profiles of the Awardees The 4th ASEAN Rural Development and Poverty Eradication Leadership Awards: Profiles of the Awardees The ASEAN Secretariat Jakarta The 4th ASEAN Rural Development and Poverty Eradication Leadership Awards: Profiles of the Awardees i The Association of Southeast Asian Nations (ASEAN) was established on 8 August 1967. The Member States of the Association are Brunei Darussalam, Cambodia, Indonesia, Lao PDR, Malaysia, Myanmar, Philippines, Singapore, Thailand and Viet Nam. The ASEAN Secretariat is based in Jakarta, Indonesia. For inquiries, contact: The ASEAN Secretariat Public Outreach and Civil Society Division 70A Jalan Sisingamangaraja Jakarta 12110 Indonesia Phone : (62 21) 724-3372, 726-2991 Fax : (62 21) 739-8234, 724-3504 E-mail : [email protected] Catalogue-in-Publication Data The 4th ASEAN Rural Development and Poverty Eradication Leadership Awards: Profiles of the Awardees Jakarta: ASEAN Secretariat, December 2020 307.7259 1. ASEAN – Rural Community – Poverty Reduction 2. Social Protection – Social Community ISBN 978-623-6945-07-0 ASEAN: A Community of Opportunities for All Photo credits: All photos are provided by ASEAN Member States The text of this publication may be freely quoted or reprinted, provided proper acknowledgement is given and a copy containing the reprinted material is sent to the Community Relations Division (CRD) of the ASEAN Secretariat, Jakarta. -

(A) Kachin State (1) Permitted Areas A. Bhamo Township B. Shwegu
Permitted Areas (a) Kachin State (1) Permitted Areas a. Bhamo Township b. Shwegu Township c. Mogaung Township d. Mohnyin Township e. Myit-kyi-na Township (2) Permitted only in the Downtown Areas a. Putao Township b. Machanbaw Township c. Mansi Township d. Momauk Township e. Waingmaw Township (3) The Areas which need to get the Prior Permission a. Naung-mon Township b. Kawng-lan-hpu Township c. Sumprabum Township d. Hpakant Township e. Tanai Township f. Injangyang Township g. Chipwi Township h. Tsawlaw Township (b) Kayah State (1) Permitted Areas a. Loi-kaw Township b. Demoso Township . Dawkaladu and Taneelalae Village in Dawkalawdu Village Group . Ngwetaung Village in Ngwetaung Village Group . Panpetrwanku, Panpetsaunglu, Panpetpemasaung . Panpetkateku and Panpetdawke Villages (Except these, other areas need to get permission) c. Hpasawng Township . Uptown Quarters in Hpasaung, Bawlakheand Mese . Towns on the bordering- trade way with Thailand . (Except these, other areas need to get permission) d. Bawlakhe Township . Uptown Quarters in Hpasaung, Bawlakheand Mese . Towns on the bordering- trade way with Thailand . (Except these, other areas need to get permission) e. Mese Township . Uptown Quarters in Hpasaung, Bawlakheand Mese . Towns on the bordering- trade way with Thailand . (Except these, other areas need to get permission) (2) Permitted only in the Downtown Areas a. Hpruso Township (3) The Areas which need to get the Prior Permission a. Shadaw Township (c) Kayin State (1) Permitted Areas a. Hpa-an Township b. Mya-wady Township . Su-kali Sub-Township . Wal-lae Sub-Township (2) Permitted only in the Downtown Areas a. Kaw-ka-reik Township . Kyone-doe Sub-Township b. -

Awaiting Trial Outside Prison
Awaiting Trial Outside Prison No. Name Sex Father's name Section of law Plaintiff Date of Arrested STAGE IN LEGAL PROCESS Detained Organization Address Remark Managing Director Kyaw Soe Chief Editor of Eleven Media Rangoon Division 1 Wai Phyo M Unknown Penal Code 500, Telecommunication Law 66(d) 00-00-14 Under trial (Outside) R/B on 6 Jan 17 Defamation the Ministry of Information of Ministry of Information Group Managing Director Kyaw Soe Chief Executive Director of Rangoon Division 2 Doctor Than Htut Aung M Unknown Penal Code 500 00-00-14 Under trial (Outside) R/B Defamation the Ministry of Information of Ministry of Information Eleven Media Group Managing Director Kyaw Soe Managing Director of Eleven Rangoon Division 3 Doctor Thein Myint M Unknown Penal Code 500 00-00-14 Under trial (Outside) R/B Defamation the Ministry of Information of Ministry of Information Media Group Managing Director Kyaw Soe Deputy Chief Editor of Rangoon Division 4 Myat Thit M Unknown Penal Code 500 00-00-14 Under trial (Outside) R/B Defamation the Ministry of Information of Ministry of Information Eleven Media Group Managing Director Kyaw Soe Editor In charge of Eleven Rangoon Division 5 Nay Tun Naing M Unknown Penal Code 500 00-00-14 Under trial (Outside) R/B Defamation the Ministry of Information of Ministry of Information Media Group U Zay Zay Aung (Former Nan Nwin Grat Village, Kangyi Daunt Destruction of land 6 U Phoee Penal Code 427, 447 _ Under trial (Outside) R/B Farmer M U Chit Hla Military Captain'son) Tsp, Irrawaddy Division U Zay Zay Aung (Former -

State Administration Council Chairman Senior General Min Aung Hlaing Attends Sales of Pearl and Gems Lots for First Day
SUMMER BENEFITS GENEROUS PEOPLE TO HAVE CHANCE OF SUPPLYING DRINKING WATER PAGE-8 (OPINION) Vol. VII, No. 351, 6th Waning of Tabaung 1382 ME www.gnlm.com.mm Friday, 2 April 2021 State Administration Council Chairman Senior General Min Aung Hlaing attends sales of pearl and gems lots for first day SALES of pearl and gems lots for April 2021 in Myanmar kyat took place at Mani Yadana Jade Hall in Nay Pyi Taw for the first day yesterday morning, attended by Chairman of the State Admin- istration Council Command- er-in-Chief of Defence Services Senior General Min Aung Hlaing. Also present at the ceremony were Council members Lt-Gen Soe Htut and Lt-Gen Moe Myint Tun, Joint-Secretary Lt-Gen Ye Win Oo, Patron of the Central Committee for Holding the My- anmar Gems Emporium Union Minister U Khin Maung Yi, Union ministers U Win Shein, U Chit Naing, U Myint Kyaing, Dr Pwint Hsan and U Maung Maung Ohn, Governor of the Central Bank of Myanmar U Than Nyein, Chair- man of Nay Pyi Taw Council Dr Maung Maung Naing, Command- er of Nay Pyi Taw Command Maj-Gen Zaw Myo Tin, deputy ministers, Nay Pyi Taw Council members, members of the cen- tral emporium committee, gems entrepreneurs and officials. State Administration Council Chairman Senior General Min Aung Hlaing is looking around the pearl lots displayed at the Mani Yadana Jade Hall in Nay Pyi Taw yesterday. Officials presented a video presentation on preparation to The Senior General and gem lots, finished gems products the hall. -

Awaiting Trial Outside Prison
Awaiting Trial Outside Prison No. Name Sex Father's name Section of law Plaintiff Date of Arrested STAGE IN LEGAL PROCESS Detained Organization Address Remark Managing Director Kyaw Soe Chief Editor of Eleven Media Rangoon Division 1 Wai Phyo M Unknown Penal Code 500, Telecommunication Law 66(d) 00-00-14 Under trial (Outside) R/B on 6 Jan 17 Defamation the Ministry of Information of Ministry of Information Group Managing Director Kyaw Soe Chief Executive Director of Rangoon Division 2 Doctor Than Htut Aung M Unknown Penal Code 500 00-00-14 Under trial (Outside) R/B Defamation the Ministry of Information of Ministry of Information Eleven Media Group Managing Director Kyaw Soe Managing Director of Eleven Rangoon Division 3 Doctor Thein Myint M Unknown Penal Code 500 00-00-14 Under trial (Outside) R/B Defamation the Ministry of Information of Ministry of Information Media Group Managing Director Kyaw Soe Deputy Chief Editor of Rangoon Division 4 Myat Thit M Unknown Penal Code 500 00-00-14 Under trial (Outside) R/B Defamation the Ministry of Information of Ministry of Information Eleven Media Group Managing Director Kyaw Soe Editor In charge of Eleven Rangoon Division 5 Nay Tun Naing M Unknown Penal Code 500 00-00-14 Under trial (Outside) R/B Defamation the Ministry of Information of Ministry of Information Media Group U Zay Zay Aung (Former Nan Nwin Grat Village, Kangyi Daunt Destruction of land 6 U Phoee Penal Code 427, 447 _ Under trial (Outside) R/B Farmer M U Chit Hla Military Captain'son) Tsp, Irrawaddy Division U Zay Zay Aung (Former -
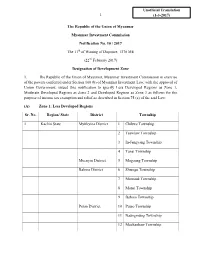
Zone Notification
Unofficial Translation 1 (1-3-2017) The Republic of the Union of Myanmar Myanmar Investment Commission Notification No. 10 / 2017 The 11th of Waning of Dapotwe, 1378 ME (22nd February 2017) Designation of Development Zone 1. The Republic of the Union of Myanmar, Myanmar Investment Commission in exercise of the powers conferred under Section 100 (b) of Myanmar Investment Law, with the approval of Union Government, issued this notification to specify Less Developed Regions as Zone 1, Moderate Developed Regions as Zone 2 and Developed Regions as Zone 3 as follows for the purpose of income tax exemption and relief as described in Section 75 (a) of the said Law: (A) Zone 1: Less Developed Regions Sr. No. Region/ State District Township 1 Kachin State Myitkyina District 1 Chibwe Township 2 Tsawlaw Township 3 In-Jangyang Township 4 Tanai Township Moenyin District 5 Mogaung Township Bahmo District 6 Shwegu Township 7 Momauk Township 8 Mansi Township 9 Bahmo Township Putao District 10 Putao Township 11 Naungmung Township 12 Machanbaw Township 2 13 Sumprabum Township 14 Kaunglanhpu Township 2 Kayah State Bawlakhe District 1 BawlakheTownship 2 Hpasaung Township 3 Mese Township Loikaw District 4 Loikaw Township 5 Demawso Township 6 Hpruso Township 7 Shataw Township 3 Kayin State Hpa-an District 1 Hpa-an Township 2 Hlaignbwe Township 3 Papun Township 4 Thandaunggyi Township Kawkareik District 5 Kawkareik Township 6 Kyain Seikkyi Township Myawady District 7 Myawady Township 4 Chin State Falam District 1 Falam Township 2 Tiddim Township 3 Hton Zan Township -

List of Townships of Burma
State/ Region Name of District Township Central Burma Magway Region Gangaw District Gangaw Township Central Burma Magway Region Gangaw District Tilin Township Central Burma Magway Region Gangaw District Saw Township Central Burma Magway Region Magway District Magway Township Central Burma Magway Region Magway District Yenangyaung Township Central Burma Magway Region Magway District Chauck Township Central Burma Magway Region Magway District Taungdwingyi Township Central Burma Magway Region Magway District Myothit Township Central Burma Magway Region Magway District Natmauk Township Central Burma Magway Region Minbu District Minbu Township Central Burma Magway Region Minbu District Pwintbyu Township Central Burma Magway Region Minbu District Ngape Township Central Burma Magway Region Minbu District Salin Township Central Burma Magway Region Minbu District Sidoktaya Township Central Burma Magway Region Pakokku District Myaing Township Central Burma Magway Region Pakokku District Pakokku Township Central Burma Magway Region Pakokku District Pauk Township Central Burma Magway Region Pakokku District Seikphyu Township Central Burma Magway Region Pakokku District Yesagyo Township Central Burma Magway Region Thayet District Aunglan Township Central Burma Magway Region Thayet District Kamma Township Central Burma Magway Region Thayet District Mindon Township Central Burma Magway Region Thayet District Minhla Township Central Burma Magway Region Thayet District Sinbaungwe Township Central Burma Magway Region Thayet District Thayet Township Central -

Lt-Gen Maung Bo on Inspection Tour of Taninthayi Division Sufficiency of Edible Oil Discussed
Established 1914 Volume XV, Number 119 15th Waning of Second Waso 1369 ME Monday, 13 August, 2007 Four political objectives Four economic objectives Four social objectives * Stability of the State, community peace * Development of agriculture as the base and all-round * Uplift of the morale and morality of development of other sectors of the economy as well and tranquillity, prevalence of law and the entire nation * Proper evolution of the market-oriented economic order * Uplift of national prestige and integ- system * National reconsolidation rity and preservation and safeguard- * Development of the economy inviting participation in * Emergence of a new enduring State ing of cultural heritage and national terms of technical know-how and investments from Constitution character sources inside the country and abroad * Building of a new modern developed * Uplift of dynamism of patriotic spirit * The initiative to shape the national economy must be kept * Uplift of health, fitness and education nation in accord with the new State in the hands of the State and the national peoples Constitution standards of the entire nation Lt-Gen Maung Bo on inspection tour of Taninthayi Division Sufficiency of edible oil discussed NAY PYI TAW, 12 Aug versity of computer stud- — Member of the State ies were opened in Peace and Development Taninthayi Division. Council Lt-Gen Maung He urged the faculty Bo of the Ministry of De- members to nurture fence, Chairman of younger generation at the Taninthayi Division Peace university to become good and Development Coun- citizens. cil Commander of Coastal He also spoke on Region Command Maj- maintenance of teaching Gen Khin Zaw Oo and aids and participation in officials left Dawei by air the tasks for greening of and arrived in Myeik on the university and its en- 10 August.