Whole Exome Sequencing of a Single Osteosarcoma Case—Integrative Analysis with Whole Transcriptome RNA-Seq Data
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

View a Copy of This Licence, Visit
Robertson et al. BMC Biology (2020) 18:103 https://doi.org/10.1186/s12915-020-00826-z RESEARCH ARTICLE Open Access Large-scale discovery of male reproductive tract-specific genes through analysis of RNA-seq datasets Matthew J. Robertson1,2, Katarzyna Kent3,4,5, Nathan Tharp3,4,5, Kaori Nozawa3,5, Laura Dean3,4,5, Michelle Mathew3,4,5, Sandra L. Grimm2,6, Zhifeng Yu3,5, Christine Légaré7,8, Yoshitaka Fujihara3,5,9,10, Masahito Ikawa9, Robert Sullivan7,8, Cristian Coarfa1,2,6*, Martin M. Matzuk1,3,5,6 and Thomas X. Garcia3,4,5* Abstract Background: The development of a safe, effective, reversible, non-hormonal contraceptive method for men has been an ongoing effort for the past few decades. However, despite significant progress on elucidating the function of key proteins involved in reproduction, understanding male reproductive physiology is limited by incomplete information on the genes expressed in reproductive tissues, and no contraceptive targets have so far reached clinical trials. To advance product development, further identification of novel reproductive tract-specific genes leading to potentially druggable protein targets is imperative. Results: In this study, we expand on previous single tissue, single species studies by integrating analysis of publicly available human and mouse RNA-seq datasets whose initial published purpose was not focused on identifying male reproductive tract-specific targets. We also incorporate analysis of additional newly acquired human and mouse testis and epididymis samples to increase the number of targets identified. We detected a combined total of 1178 genes for which no previous evidence of male reproductive tract-specific expression was annotated, many of which are potentially druggable targets. -

Proteome-Wide Onco-Proteogenomic Somatic Variant Identification in ER
Clinical Biochemistry 66 (2019) 63–75 Contents lists available at ScienceDirect Clinical Biochemistry journal homepage: www.elsevier.com/locate/clinbiochem Proteome-wide onco-proteogenomic somatic variant identification in ER- positive breast cancer T Lampros Dimitrakopoulosa,b,c,1, Ioannis Prassasb,c,1, Anieta M. Sieuwertsd, ⁎⁎ ⁎ Eleftherios P. Diamandisa,b,c,e, John W.M. Martensd, , George S. Charamesa,b,c, a Department of Laboratory Medicine and Pathobiology, University of Toronto, 1 King's College Circle, Toronto, ON M5S 1A8, Canada b Department of Pathology and Laboratory Medicine, Mount Sinai Hospital, Joseph and Wolf Lebovic Health Complex, 600 University Avenue, Toronto, ON M5G 1X5, Canada c Lunenfeld-Tanenbaum Research Institute, Sinai Health System, 600 University Avenue, Toronto, ON M5G 1X5, Canada d Department of Medical Oncology and Cancer Genomics Netherlands, Erasmus MC Cancer Institute, Erasmus University Medical Center, Wytemaweg 80, 3015CN Rotterdam, The Netherlands e Department of Clinical Biochemistry, University Health Network, 190 Elizabeth Street, Toronto, ON M5G 2C4, Canada ARTICLE INFO ABSTRACT Keywords: Background: Recent advances in mass spectrometric instrumentation and bioinformatics have critically con- Onco-proteogenomics tributed to the field of proteogenomics. Nonetheless, whether that integrative approach has reached the point of Variant peptides maturity to effectively reveal the flow of genetic variants from DNA to proteins still remains elusive. The ob- Somatic mutations jective of this study was to detect somatically acquired protein variants in breast cancer specimens for which full Breast cancer genome and transcriptome data was already available (BASIS cohort). LC-MS/MS Methods: LC-MS/MS shotgun proteomic results of 21 breast cancer tissues were coupled to DNA sequencing data to identify variants at the protein level and finally were used to associate protein expression with gene expression levels. -

A Genome-Wide Association Scan in Admixed Latin Americans Identifies Loci Influencing Facial and Scalp Hair Features
The University of Bradford Institutional Repository http://bradscholars.brad.ac.uk This work is made available online in accordance with publisher policies. Please refer to the repository record for this item and our Policy Document available from the repository home page for further information. To see the final version of this work please visit the publisher’s website. Available access to the published online version may require a subscription. Link to publisher’s version: http://dx.doi.org/10.1038/ncomms10815 Citation: Adhikari K, Fontanil T, Cal S, et al. (2016) A genome-wide association scan in admixed Latin Americans identifies loci influencing facial and scalp hair features. Nature Communications, 7, Article No. 10815. Copyright statement: © 2016 The Authors. Published by Nature. This work is licensed under a Creative Commons Attribution 4.0 International License. http://creativecommons.org/licenses/by/4.0/ ARTICLE Received 13 Jul 2015 | Accepted 25 Jan 2016 | Published 1 Mar 2016 DOI: 10.1038/ncomms10815 OPEN A genome-wide association scan in admixed Latin Americans identifies loci influencing facial and scalp hair features Kaustubh Adhikari1, Tania Fontanil2, Santiago Cal2, Javier Mendoza-Revilla1,3, Macarena Fuentes-Guajardo1,4, Juan-Camilo Chaco´n-Duque1, Farah Al-Saadi1, Jeanette A. Johansson5, Mirsha Quinto-Sanchez6, Victor Acun˜a-Alonzo1,7, Claudia Jaramillo8, William Arias8, Rodrigo Barquera Lozano7,9, Gasto´n Macı´nPe´rez7,9, Jorge Go´mez-Valde´s10, Hugo Villamil-Ramı´rez9,Ta´bita Hunemeier11,w, Virginia Ramallo6,11, Caio C. Silva de Cerqueira6,11, Malena Hurtado3, Valeria Villegas3, Vanessa Granja3, Carla Gallo3, Giovanni Poletti3, Lavinia Schuler-Faccini11, Francisco M. -

SUPPORTING INFORMATION for Regulation of Gene Expression By
SUPPORTING INFORMATION for Regulation of gene expression by the BLM helicase correlates with the presence of G4 motifs Giang Huong Nguyen1,2, Weiliang Tang3, Ana I. Robles1, Richard P. Beyer4, Lucas T. Gray5, Judith A. Welsh1, Aaron J. Schetter1, Kensuke Kumamoto1,6, Xin Wei Wang1, Ian D. Hickson2,7, Nancy Maizels5, 3,8 1 Raymond J. Monnat, Jr. and Curtis C. Harris 1Laboratory of Human Carcinogenesis, National Cancer Institute, National Institutes of Health, Bethesda, Maryland, U.S.A; 2Department of Medical Oncology, Weatherall Institute of Molecular Medicine, John Radcliffe Hospital, University of Oxford, Oxford, U.K.; 3Department of Pathology, University of Washington, Seattle, WA U.S.A.; 4 Center for Ecogenetics and Environmental Health, University of Washington, Seattle, WA U.S.A.; 5Department of Immunology and Department of Biochemistry, University of Washington, Seattle, WA U.S.A.; 6Department of Organ Regulatory Surgery, Fukushima Medical University, Fukushima, Japan; 7Cellular and Molecular Medicine, Nordea Center for Healthy Aging, University of Copenhagen, Denmark; 8Department of Genome Sciences, University of WA, Seattle, WA U.S.A. SI Index: Supporting Information for this manuscript includes the following 19 items. A more detailed Materials and Methods section is followed by 18 Tables and Figures in order of their appearance in the manuscript text: 1) SI Materials and Methods 2) Figure S1. Study design and experimental workflow. 3) Figure S2. Immunoblot verification of BLM depletion from human fibroblasts. 4) Figure S3. PCA of mRNA and miRNA expression in BLM-depleted human fibroblasts. 5) Figure S4. qPCR confirmation of mRNA array data. 6) Table S1. BS patient and control detail. -

Transcriptional Characterization and Functional Analysis of Long Non-Coding RNA/Protein-Coding Gene Pairs Encoded in the Human Genome
Transcriptional characterization and functional analysis of long non-coding RNA/protein-coding gene pairs encoded in the human genome Inaugural-Dissertation to obtain the academic degree Doctor rerum naturalium (Dr. rer. nat.) submitted to the Department of Biology, Chemistry and Pharmacy of Freie Universität Berlin by Anne-Susann Musahl from Berlin Berlin, 2015 ii The present work was carried out from March 2012 until April 2015 at the Max Planck Institute for Molecular Genetics under the supervision of Dr. Ulf Andersson Ørom. 1st Reviewer: Dr. Ulf Andersson Ørom 2nd Reviewer:Prof. Dr. Markus Wahl Date of Defence: 10.07.2015 iii Für Küsschen und das Entchen. iv v Acknowledgements I would like to thank my PhD advisor Dr. Ulf Ørom for giving me the opportunity to work in his lab and on this exciting project. Ulf provided me with guidance and support but also gave me the freedom to develop and follow own research ideas. I also want to thank Prof. Dr. Markus Wahl for reviewing this PhD thesis. Many thanks goes to my friends and colleagues in the lab: Dubravka Vučićević, Thomas Conrad, Evgenia Ntini, Annita Louloupi, Alexander Kiefer, Julia Liz, Maja Gehre, An- tonia Hilbig and Masha Kenda, you guys provided such a friendly and helpful working environment that enabled me to finish this PhD work. Special thanks goes to Dusa, Thomas and Evgenia for many insightful scientific discussions and their endless technical and moral support to pass all big and small problems that emerged in the last three years. Also, this work would never have been possible without the help of my co-authors at the Max Planck Institute and in Paris and Villejuif (France), therefore I would like to thank Annalisa Marsico, Ruping Sun, Marcus W. -

Lupus Nephritis Supp Table 5
Supplementary Table 5 : Transcripts and DAVID pathways correlating with the expression of CD4 in lupus kidney biopsies Positive correlation Negative correlation Transcripts Pathways Transcripts Pathways Identifier Gene Symbol Correlation coefficient with CD4 Annotation Cluster 1 Enrichment Score: 26.47 Count P_Value Benjamini Identifier Gene Symbol Correlation coefficient with CD4 Annotation Cluster 1 Enrichment Score: 3.16 Count P_Value Benjamini ILMN_1727284 CD4 1 GOTERM_BP_FAT translational elongation 74 2.50E-42 1.00E-38 ILMN_1681389 C2H2 zinc finger protein-0.40001984 INTERPRO Ubiquitin-conjugating enzyme/RWD-like 17 2.00E-05 4.20E-02 ILMN_1772218 HLA-DPA1 0.934229063 SP_PIR_KEYWORDS ribosome 60 2.00E-41 4.60E-39 ILMN_1768954 RIBC1 -0.400186083 SMART UBCc 14 1.00E-04 3.50E-02 ILMN_1778977 TYROBP 0.933302249 KEGG_PATHWAY Ribosome 65 3.80E-35 6.60E-33 ILMN_1699190 SORCS1 -0.400223681 SP_PIR_KEYWORDS ubl conjugation pathway 81 1.30E-04 2.30E-02 ILMN_1689655 HLA-DRA 0.915891173 SP_PIR_KEYWORDS protein biosynthesis 91 4.10E-34 7.20E-32 ILMN_3249088 LOC93432 -0.400285215 GOTERM_MF_FAT small conjugating protein ligase activity 35 1.40E-04 4.40E-02 ILMN_3228688 HLA-DRB1 0.906190291 SP_PIR_KEYWORDS ribonucleoprotein 114 4.80E-34 6.70E-32 ILMN_1680436 CSH2 -0.400299744 SP_PIR_KEYWORDS ligase 54 1.50E-04 2.00E-02 ILMN_2157441 HLA-DRA 0.902996561 GOTERM_CC_FAT cytosolic ribosome 59 3.20E-33 2.30E-30 ILMN_1722755 KRTAP6-2 -0.400334007 GOTERM_MF_FAT acid-amino acid ligase activity 40 1.60E-04 4.00E-02 ILMN_2066066 HLA-DRB6 0.901531942 SP_PIR_KEYWORDS -
WO 2016/070129 Al 6 May 2016 (06.05.2016) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/070129 Al 6 May 2016 (06.05.2016) W P O P C T (51) International Patent Classification: (74) Agent: BAKER, C , Hunter; Wolf, Greenfield & Sacks, A61K 9/00 (2006.01) C07K 14/435 (2006.01) P.C., 600 Atlantic Avenue, Boston, MA 02210-2206 (US). (21) International Application Number: (81) Designated States (unless otherwise indicated, for every PCT/US20 15/058479 kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (22) International Filing Date: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, 30 October 2015 (30.10.201 5) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (25) Filing Language: English HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (26) Publication Language: English MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (30) Priority Data: PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, 14/529,010 30 October 2014 (30. 10.2014) US SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (71) Applicant: PRESIDENT AND FELLOWS OF HAR¬ VARD COLLEGE [US/US]; 17 Quincy Street, Cam (84) Designated States (unless otherwise indicated, for every bridge, MA 02138 (US). -

Fátima Lopes Mscthesis VERSÃO FINAL IMPRESSÃO ANÓNIMO
Universidade de Aveiro Departamento de Química Ano 2011 Fátima Daniela Alterações de dosagem no genoma de doentes com Teixeira Lopes atraso mental Genomic imbalances in patients with intellectual disability Universidade de Aveiro Departamento de Química Ano 2011 Fátima Daniela Alterações de dosagem no genoma de doentes Teixeira Lopes com atraso mental Genomic imbalances in patients with intellectual disability Dissertação apresentada à Universidade de Aveiro para cumprimento dos requisitos necessários à obtenção do grau de Mestre em Biotecnologia , realizada sob a orientação científica da Doutor a Patrícia Espinheira de Sá Maciel, Professora A uxiliar da Escola de Ciências da Saúde da Universidade do Minho, e da Doutora Odete Cruz e Silva, Professora A uxiliar do Departamento de Biologia da Universidade de Aveiro. Apoio financeiro da FCT (PIC/IC/83026/2007) no âmbito do III Quadro Comunitário de Apoio. “Sooner or later we will find the cause, and it will be in exactly the same way as we have found genes for other disorders - by lucky coincidence. (…)There isn't anything unique about not having discovered it yet." John Marius Opitz, 1997 Por este motivo, este pequeno contributo é dedicado aos pais das crianças envolvidas neste estudo. o júri presidente Professor Doutor Jorge Manuel Alexandre Saraiva Investigador Auxiliar do Departamento de Química da Universidade de Aveiro Professora Doutora Filipa Abreu Gomes de Carvalho Professora Associada com Agregação da Faculdade de Medicina da Universidade do Porto Professora Doutora Patrícia Espinheira de Sá Maciel Professora Auxiliar da Escola de Ciências da Saúde da Universidade do Minho Professora Doutora Odete Cruz e Silva Professora Auxiliar do Departamento de Biologia da Universidade de Aveiro. -

WO 2016/004387 Al 7 January 2016 (07.01.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/004387 Al 7 January 2016 (07.01.2016) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61P 35/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/US20 15/039 108 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 2 July 2015 (02.07.2015) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (25) Filing Language: English PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 62/020,3 10 2 July 2014 (02.07.2014) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: H. LEE MOFFITT CANCER CENTER GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, AND RESEARCH INSTITUTE, INC. [US/US]; 12902 TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, Magnolia Dr., Tampa, FL 336 12-9497 (US). -

Genome-Wide Gene-Diabetes and Gene-Obesity Interaction Scan In
Author Manuscript Published OnlineFirst on June 16, 2020; DOI: 10.1158/1055-9965.EPI-20-0275 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Genome-wide gene-diabetes and gene-obesity interaction scan in 8,255 cases and 11,900 controls from Pancreatic Cancer Cohort Consortium and Pancreatic Cancer Case Control Consortium Hongwei Tang*1, Lai Jiang*2, Rachael Z. Stolzenberg-Solomon3, Alan A. Arslan4,5,6,, Laura E. Beane Freeman3, Paige M. Bracci7, Paul Brennan8, Federico Canzian9, Mengmeng Du10, Steven Gallinger11, Graham G. Giles12,13,14, Phyllis J. Goodman15, Charles Kooperberg16, Loic Le Marchand17, Rachel E. Neale18, Xiao-Ou Shu19, Kala Visvanathan20,21, Emily White22, Wei Zheng19, Demetrius Albanes3, Gabriella Andreotti3, Ana Babic23, William R. Bamlet24, Sonja I. Berndt3, Amanda Blackford21, Bas Bueno-de-Mesquita25,26,27,28, Julie E. Buring2,29, Daniele Campa30, Stephen J. Chanock3, Erica Childs21, Eric J. Duell31, Charles Fuchs32,33,34, J. Michael Gaziano29,35, Michael Goggins36, Patricia Hartge3, Manal H Hassam1, Elizabeth A. Holly7, Robert N. Hoover3, Rayjean J. Hung11, Robert C. Kurtz37, I-Min Lee2,29, Núria Malats38, Roger L. Milne12,13,14, Kimmie Ng23, Ann L. Oberg24, Irene Orlow10, Ulrike Peters22, Miquel Porta39,40, Kari G. Rabe24 , Nathaniel Rothman3, Ghislaine Scelo8, Howard D. Sesso2,29, Debra T. Silverman3, Ian M. Thompson, Jr41, Anne Tjønneland42, Antonia Trichopoulou43, Jean Wactawski-Wende44, Nicolas Wentzensen3, Lynne R. Wilkens17, Herbert Yu17, Anne Zeleniuch- Jacquotte5,6, Laufey T. Amundadottir3, Eric J. Jacobs42, Gloria M. Petersen24, Brian M. Wolpin23, Harvey A. Risch45, Nilanjan Chatterjee46, Alison P. Klein21,36 Donghui Li#1, Peter Kraft#2,47, Peng Wei#48. -

Genome-Wide Dna Methylation and Imprinted Gene Analysis In
GENOME-WIDE DNA METHYLATION AND IMPRINTED GENE ANALYSIS IN BABIES CONCEIVED BY ART by LUKE DAVID GOODING B.Sc., The University of British Columbia, 2014 A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE in THE FACULTY OF GRADUATE AND POSTDOCTORAL STUDIES (Reproductive and Developmental Sciences) THE UNIVERSITY OF BRITISH COLUMBIA (Vancouver) October 2019 © Luke David Gooding, 2019 The following individuals certify that they have read, and recommend to the Faculty of Graduate and Postdoctoral Studies for acceptance, a thesis entitled: Genome-wide DNA methylation and imprinted gene analysis in babies conceived by ART submitted by Luke David Gooding in partial fulfillment of the requirements for the degree of Master of Science in Reproductive and Developmental Sciences Examining Committee: Dr. Paul Yong Supervisor Dr. Patrice Eydoux Supervisory Committee Member Dr. Wan Lam Supervisory Committee Member Dr. Angela Devlin Additional Examiner Additional Supervisory Committee Members: Dr. Dan Rurak Supervisory Committee Member ii Abstract Assisted reproductive technologies (ARTs) are associated with a number of adverse pregnancy, neonatal, and long-term outcomes. One plausible explanation is that ART procedures may be causing alterations in epigenetic mechanisms, including the regulation of imprinted genes, that persist during development. Therefore, I investigated gene expression of the imprinted genes PLAGL1, CDKN1C, KCNQ1OT1, and H19 in cord blood from 24 IVF, 18 ICSI, 9 IUI, and 26 naturally conceived babies as well as genome-wide DNA methylation using Illumina’s EPIC methylation array in cord blood from 10 IVF, 9 ICSI, and 10 naturally conceived babies. All the samples were procured from healthy newborn singletons. -
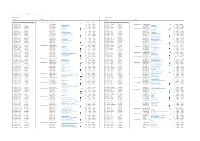
Lupus Nephritis Supp Table 7
Supplementary Table 7 : Transcripts and DAVID pathways correlating with expression of CD3 in lupus kidney biopsies Positive correlation Negative correlation Transcripts Pathways Transcripts Pathways Identifier Gene Symbol Correlation coefficient with CD3 Annotation Cluster 1 Enrichment Score: 11.22 Count P_Value Benjamini Identifier Gene Symbol Correlation coefficient with CD3 ILMN_2325837 CD3D 1 SP_PIR_KEYWORDS ribosome 42 5.40E-21 1.20E-18 ILMN_1726667 LOC728758 -0.40000032 Annotation Cluster 1 Enrichment Score: 8.3 Count P_Value Benjamini ILMN_2061043 CD48 0.905183649 GOTERM_BP_FAT translational elongation 49 2.00E-18 8.60E-15 ILMN_1767032 DDI1 -0.400066325 SP_PIR_KEYWORDS oxidoreductase 98 1.10E-11 3.90E-09 ILMN_2261416 CD3D 0.880984568 GOTERM_CC_FAT cytosolic ribosome 42 3.50E-17 2.30E-14 ILMN_3307863 TAOK3 -0.400088253 GOTERM_BP_FAT oxidation reduction 105 3.70E-10 1.40E-06 ILMN_1886655 TCRVB 0.875380574 SP_PIR_KEYWORDS protein biosynthesis 64 1.10E-16 1.00E-14 ILMN_1840934 AJ420430 -0.400098378 GOTERM_MF_FAT electron carrier activity 40 3.10E-05 5.90E-03 ILMN_1659800 BCL11A 0.861258356 KEGG_PATHWAY Ribosome 44 6.90E-15 1.10E-12 ILMN_3235584 TRIM66 -0.400113232 Annotation Cluster 2 Enrichment Score: 7.1 Count P_Value Benjamini ILMN_2098126 CCL5 0.853134526 GOTERM_CC_FAT cytosolic part 55 8.50E-14 1.80E-11 ILMN_2145760 YIPF4 -0.400116748 SP_PIR_KEYWORDS mitochondrion 143 3.20E-16 2.30E-13 ILMN_1716651 RUNX2 0.839003672 GOTERM_CC_FAT ribosomal subunit 48 8.70E-13 1.40E-10 ILMN_2146648 PRB3 -0.400169733 GOTERM_CC_FAT mitochondrion 176