Metabolic Parameters in Patients with Suspected Reactive Hypoglycemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
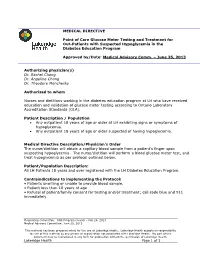
MEDICAL DIRECTIVE Point of Care Glucose Meter Testing And
MEDICAL DIRECTIVE Point of Care Glucose Meter Testing and Treatment for Out-Patients with Suspected Hypoglycemia in the Diabetes Education Program Approved by/Date: Medical Advisory Comm. – June 25, 2013 Authorizing physician(s) Dr. Rachel Chong Dr. Angeline Chong Dr. Theodore Monchesky Authorized to whom Nurses and dietitians working in the diabetes education program at LH who have received education and validation of glucose meter testing according to Ontario Laboratory Accreditation Standards (OLA). Patient Description / Population Any outpatient 18 years of age or older at LH exhibiting signs or symptoms of hypoglycemia. Any outpatient 18 years of age or older suspected of having hypoglycemia. Medical Directive Description/Physician’s Order The nurse/dietitian will obtain a capillary blood sample from a patient’s finger upon suspecting hypoglycemia. The nurse/dietitian will perform a blood glucose meter test, and treat hypoglycemia as per protocol outlined below. Patient/Population Description: All LH Patients 18 years and over registered with the LH Diabetes Education Program. Contraindications to implementing the Protocol: • Patients unwilling or unable to provide blood sample. • Patient less than 18 years of age • Refusal of patient/family consent for testing and/or treatment; call code blue and 911 immediately Originating Committee: RNS Program Council – Feb 26, 2013 Medical Advisory Committee: June 25, 2013 This material has been prepared solely for the use at Lakeridge Health. Lakeridge Health accepts no responsibility for use of this material by any person or organization not associated with Lakeridge Health. No part of this document may be reproduced in any form for publication without the permission of Lakeridge Health. -

Diabetes Control in Thyroid Disease
In Brief Thyroid disease is commonly found in most types of diabetes. This article defines the prevalence of thyroid disease in diabetes and elucidates through case studies the assessment, diagnosis, and clinical management of thyroid disease in diabetes. Diabetes Control in Thyroid Disease Thyroid disease is a pathological state abnormality. Several studies, including that can adversely affect diabetes con- the Colorado study, have documented trol and has the potential to negative- a higher prevalence of thyroid disease Jennal L. Johnson, MS, RNC, FNP, ly affect patient outcomes. Thyroid in women, with prevalence rates rang- BC-ADM, CDE disease is found commonly in most ing from 4 to 21%, whereas the rate in forms of diabetes and is associated men ranges from 2.8 to 16%.1 with advanced age, particularly in Thyroid disease increases with age. In type 2 diabetes and underlying the Colorado study, the 18-year-olds autoimmune disease in type 1 dia- had a prevalence rate of 3.5% com- betes. This article defines the preva- pared with a rate of 18.5% for those lence of thyroid disease in diabetes, ≥ 65 years of age. discusses normal physiology and The prevalence of thyroid disease in screening recommendations for thy- diabetes has been estimated at 10.8%,2 roid disease, and elucidates through with the majority of cases occurring as case studies the assessment, diagnosis, hypothyroidism (~ 30%) and subclini- and clinical management of thyroid cal hypothyroidism (~ 50%).2 Hyper- disease and its impact on diabetes. thyroidism accounts for 12%, and postpartum thyroiditis accounts for Thyroid Disease Prevalence 11%.2 Of the female patients with The prevalence of thyroid disease in type 1 diabetes, 30% have thyroid dis- the general population is estimated to ease, with a rate of postpartum thy- be 6.6%, with hypothyroidism the roid disease three times that of the most common malady.1 Participants normal population. -

Refractory Hypoglycemia in T-Cell Lymphoma
Open Access Austin Oncology Case Reports Case Report Refractory Hypoglycemia in T-Cell Lymphoma Buyukaydina B1*, Tunca M1, Alayb M2, Kazanciogluc R3 and Reha E3 Abstract 1Bezmialem Vakif University, Department of Internal Hypoglycemia is commonly seen in diabetes mellitus patients; whereas it Medicine, Turkey is rarely seen in a healthy person. In this case, we reported a male patient 2Yuzuncu Yil University, Department of Endocrinology, with a treatment-resistant hypoglycemia. A 53 years old male patient admitted Turkey to our clinic with debility, nausea and vomiting. Physical examination revealed 3Bezmialem Vakif University, Department of Nephology, lymphadenopathies in the left axilla and inguinal regions; and presence of right Turkey upper quadrant tenderness. Biochemical results revealed severe hypoglycemia, *Corresponding author: Banu Buyukaydin, azotemia and elevation of liver enzymes. Histological result of the excisional Bezmialem Vakif University, Department of Internal lymph node biopsy was compatible with peripheral T cell lymphoma. In ward, Medicine, Turkey the patient has repeated recurrent hypoglycemia, which did not resolve with all treatment given. His general condition deteriorated and he died due to sepsis. Received: June 01, 2016; Accepted: July 10, 2016; This case highlighted the need to rule out hematologic malignancies; precisely Published: July 13, 2016 T-cell lymphoma in a patient who presented with resistant hypoglycemia in the presence of lymphadenopathy. Keywords: Hypoglycemia, Lymphoma, IGF-II Introduction approximately fifty percent of proliferation index. CD3 was positive. This finding was compatible to histological diagnosis of peripheral Hypoglycemia is defined as the occurrence of a variety of T-cell lymphoma with partial involvement of lymph ganglia. symptoms in association with plasma glucose concentration of 50mg/dl or less. -

An Educational Booklet for Patients with Familial Hypercholesterolemia
Illustrations > Jean Lambert Illustrations graphic design > www.mine-de-rien.net graphic Chol/29/P030/01-01/10 NLA An educational booklet for patients with familial hypercholesterolemia This brochure was provided by Genzyme Corporation for use by the Foundation of the National Lipid Association. DR. LEIV OSE www.learnyourlipids.com CONTENTS PART 1 What will you learn from this booklet? 02 FAMILIAL HYPERCHOLESTEROLEMIA PART 1: FAMILIAL HYPERCHOLESTEROLEMIA 03 1 - What is Familial Hypercholesterolemia? 03 WHAT WILL YOU 2 - What is LDL-Cholesterol? 04 3 - What are the causes of FH? 05 LEARN FROM THIS GREAT GRANDMOTHER GREAT GRANDFATHER 4 - When should FH be suspected? 07 FH NON FH BOOKLET? 5 - How is FH diagnosed? 09 6 - How early can FH be diagnosed? 09 Woman You will learn about Familial PART 2: TREATMENT 10 GRANDMOTHER GRANDFATHER Hypercholesterolemia, NON FH FH Woman with FH 1 - How can LDL-Cholesterol be reduced? 10 its cause, and the potential 2 - Step 1: Dietary management of FH 11 Man consequences of this a) How does diet affect LDL-Cholesterol? 11 disease. You will learn b) What sort of diet? 11 Man with FH about high cholesterol 3 - Step 2: Using medication 12 AUNT MOTHER FATHER UNCLE and what this might mean a) How does medication affect LDL-Cholesterol? 12 NON FH FH NON FH FH for your heart and blood b) Which drug treatments reduce LDL-Cholesterol and how? 13 FIGURE 1: 4 - Why is lifelong treatment important? vessels. Most importantly 15 FH is an inherited disease, you will learn how to find PART 3: CARDIOVASCULAR DISEASE AND LIPOPROTEINS 16 which can usually be traced out whether someone in 1 - What is cardiovascular disease? 16 DAUGTER SON over several generations. -

CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E
Peer Reviewed PRACTICAL ONCOLOGY CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E. Burgess, DVM, Diplomate ACVIM (Oncology) Tufts University An insulinoma is a malignant pancreatic tumor that DIAGNOSIS inappropriately secretes excessive insulin, resulting in Aside from a histologic confirmation of insulinoma, profound hypoglycemia.1 no currently available diagnostic test provides a de- Pancreatic tumors are classified as: finitive diagnosis of insulinoma. Existing techniques • Exocrine, which includes adenocarcinomas of may help increase suspicion for an insulin-secreting ductular or acinar origin tumor but, with most diagnostic testing, it is im- • Endocrine, which arise from the islets of perative to interpret all results in the context of the Langerhans. coexisting clinical signs. Insulinomas are functional neuroendocrine tumors that originate in the beta cells of the islets Differential Diagnosis of Langerhans.1 A complete work-up, including careful patient history, physical examination, bloodwork, and PRESENTATION diagnostic imaging tests, should be performed to Signalment rule out other causes of hypoglycemia, such as Any breed of dog can be affected, but large sepsis, hepatic failure, adrenal cortical insufficiency, breeds tend to be overrepresented.1 While, in toxin ingestion, and other forms of neoplasia. humans, insulinomas affect females far more frequently than males, there is no apparent sex Laboratory Tests predilection in dogs.1-3 Dogs also commonly Blood Glucose present with a malignant variant, while humans A simple fasting blood glucose level of less than often have a benign adenoma (80%).1 Insulino- 40 mg/dL can suggest hyperinsulinemia, although ma is rare in cats.4 careful monitoring of a fasted dog with suspected insulinoma is strongly recommended due to high Clinical Signs risk for seizure activity. -

Reactive Hypoglycemia from Metformin Immediate-Release Monotherapy Resolved by a Switch to Metformin Extended-Release: Conceptualizing Their Concentration-Time Curves
Open Access Case Report DOI: 10.7759/cureus.16112 Reactive Hypoglycemia From Metformin Immediate-Release Monotherapy Resolved by a Switch to Metformin Extended-Release: Conceptualizing Their Concentration-Time Curves Ayesha Akram 1, 2 1. Internal Medicine, Combined Military Hospital, Rawalpindi, PAK 2. Internal Medicine, Rawalpindi Medical University, Rawalpindi, PAK Corresponding author: Ayesha Akram, [email protected] Abstract Metformin rarely, if ever, causes hypoglycemia when it is used as labeled. A 55-year-old woman presented to the medicine ward with an altered level of consciousness. She had been reviewed in an outpatient department three days earlier and prescribed 500 mg two times per day of metformin immediate-release (Met IR) for newly diagnosed type 2 diabetes mellitus (T2DM), to which she had been adherent; however, she had been experiencing intermittent episodes of hypoglycemia after taking the medication prescribed to treat her T2DM. On physical examination, she was diaphoretic and disoriented but responsive to sensory stimuli. In the ward, she received 25 ml of intravenous dextrose as the initial blood glucose reading was low at 54 mg/dl, and 4 ounces of apple juice additionally two hours later as her blood glucose level fell below 70 mg/dl again. She was no longer hypoglycemic a few hours later, and there was a significant neurological improvement. The remainder of the laboratory results, including serum renal and liver function tests, were normal. Met IR was discontinued, and metformin extended-release (Met XR) 500 mg/day was initiated at discharge. The patient's hypoglycemic episodes resolved within days after the initiation of Met XR. -

Core Laboratory
Performance of the vast majority of Hematology, Coagulation, Urinalysis, Clinical Chemistry and Toxicology testing procedures is conducted in the CORE LABORATORY - an advanced, highly automated area where whole blood, serum, plasma, urine and other biological fluid specimens are tested for a comprehensive menu of state-of-the-art laboratory procedures. Significant testing procedures for Clinical Chemistry and Toxicology includes panels currently approved by the Centers for Medicare and Medicaid Services: Basic Metabolic Panel; Comprehensive Metabolic Panel; Liver Function Panel; Renal Function Panel; and Electrolyte Panel. Other key tests include the Lipid Profile (Cholesterol, Triglyceride, HDL- Cholesterol and LDL-Cholesterol), major markers of cardiovascular disease and risk [such as Troponin I, Myoglobin and Beta-type natriuretic peptide (commonly referred to as BNAT or BNP)], critical care analytes, beta-HCG, and significant therapeutic drug levels. Urinary toxicology screens for major drugs of abuse (and/or key metabolites) are also performed. The cornerstones of Hematology testing are analyses of the complete blood count (CBC) and the differential (DIFF). These include evaluation of: (1) white blood cell count and differential with percentage and absolute value given for the leukocyte components; (2) circulating erythrocytes by means of hemoglobin, hematocrit, red blood cell count, and red blood cell indices; and (3) measurement of platelet concentration by count and/or estimation. Morphological variations and changes of cellular constituents are reported. Alteration of any aspect of the hemostatic mechanism may cause abnormal bleeding in a wide variety of familial and acquired disorders. These defects may be differentiated by a profile of significant Coagulation laboratory tests that includes PT, PTT, Fibrinogen, FDP, and D-Dimer for monitoring anticoagulant therapy. -

Glucose Regulation in Diabetes
Glucose Regulation in Diabetes Samantha Lozada Advised by Charles S. Peskin and Thomas Fai Glucose 1 Abstract Complicated and extensive models of glucose regulation, involving several variables, have been developed over the years. Our research specifically focuses on the feedback loop between insulin and glucagon. Although our model is simpler than a model including state variables such as non-esterified fatty acids concentration in the blood plasma, β-cell mass, TAG content of lipocytes, and/or leptin concentrations in the blood plasma, we are still able to simulate most of the key effects of diabetes and other health problems on glucose regulation; such as, hyperglycemia, hyperinsulinism, and insulin shock (hypoglycemia). We are even able to simulate eating a bowl of vanilla ice cream! 2 Introduction For most of our qualitative and quantitative experimentations we worked with MATLAB, a computer programming language and data visualization software, which offers a rich set of tools for solving problems in engineering, scientific, computing, and mathematical disciplines, such as a graphical user interface. Our model is a refinement of a realistic model developed by Cobelli et al. (1982). Despite the fact that the paper is nearly 28 years old, the experimental data of diagnostic tests used by medical professionals, such as the Intravenous Glucose Tolerance Test (IVGTT), correlates with our simulated graphs. From a Biological Perspective Regulation in a Healthy System In order for us to model any biological system, we need to first understand exactly what is happening within a human body. We need to ask what causes this effect and why. To answer these questions we need to identify the key organs and hormones, and then see how they interact within our bodies. -

Genetic Testing for Familial Hypercholesterolemia AHS – M2137
Corporate Medical Policy Genetic Testing for Familial Hypercholesterolemia AHS – M2137 File Name: genetic_testing_for_familial_hypercholesterolemia Origination: 01/01/2019 Last CAP Review: 07/2021 Next CAP Review: 07/2022 Last Review: 07/2021 Description of Procedure or Service Definitions Familial hypercholesterolemia (FH) is a genetic condition that results in premature atherosclerotic cardiovascular disease due to lifelong exposure to elevated low-density lipoprotein cholesterol (LDL-C) levels (Sturm et al., 2018). FH encompasses multiple clinical phenotypes associated with distinct molecular etiologies. The most common is an autosomal dominant disorder caused by mutations in one of three genes, low-density lipoprotein receptor (LDLR), apolipoprotein B-100 (APOB), and proprotein convertase subtilisin-like kexin type 9 (PCSK9) (Ahmad et al., 2016; Goldberg et al., 2011). Rare autosomal recessive disease results from mutation in low-density lipoprotein receptor adaptor protein (LDLRAP) (Garcia et al., 2001). Related Policies Cardiovascular Disease Risk Assessment AHS – G2050 ***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician. Policy BCBSNC will provide coverage for genetic testing for familial hypercholesterolemia when it is determined the medical criteria or reimbursement guidelines below are met. Benefits Application This medical policy relates only to the services or supplies described herein. Please refer to the Member's Benefit Booklet for availability of benefits. Member's benefits may vary according to benefit design; therefore member benefit language should be reviewed before applying the terms of this medical policy. When Genetic Testing for Familial Hypercholesterolemia is covered 1. Genetic testing to establish a molecular diagnosis of Familial Hypercholesterolemia is considered medically necessary when BOTH of the following criteria are met: A. -

Religious Fasting, Ramadan and Hypoglycemia in People with Diabetes
VOLUME 7 > ISSUE 01 > JUNE 30 2014 SPOTLIGHT ARTICLE Diabetic Hypoglycemia June 2014, Volume 7, Issue 1: page 15-19 Religious fasting, Ramadan and hypoglycemia in people with diabetes Alia Gilani1, Melanie Davies2, Kamlesh Khunti2 1 NHS Glasgow, United Kingdom 2 Leicester Diabetes Centre, Leicester General Hospital, Leicester, United Kingdom Abstract Most Muslims with diabetes will take part in Ramadan even though they may be exempt from doing so. In some countries a religious fast can last between 10 and 21 hours. The main risk of fasting to people with diabetes is hypoglycemia. People with diabetes who fast may have to alter the dose of their medications or modify their therapeutic regimen to avoid hypoglycemia, which can have adverse effects on glycemic control. Therapies which pose a high risk of hypoglycemia when used during fasting are sulfonylureas and insulin therapy. Metformin, incretin therapies and the newer sodium glucose co-transporter 2 inhibitor class have a low risk of hypoglycemia. The practice of fasting during Ramadan is advocated for all healthy individuals. If deemed detrimental to health then a person can be considered exempt from fasting; this includes frail and elderly people, pregnant and breast feeding women, children and people with multi-morbidities. Keywords: diabetes, hypoglycemia, Ramadan, religious fasting Introduction the Islamic calendar, the risks associated with prolonged fasting and how it should be managed. Living in a diverse society, it is important that healthcare professionals are kept informed about cultural and religious Fasting during Ramadan practices, which can affect the control of diabetes. The practice of fasting by Muslims has implications for Muslim What does fasting entail? people with diabetes, in particular an increased risk of Ramadan in Arabic is translated as “sawm”, literally hypoglycemia during the period of Ramadan and at other meaning “abstention from”. -

Table of Contents
DISCLAIMER The information contained within this document is restricted to and intended for professional use by licensed health care providers. The statements made should not be construed as a claim, nor does it represent any particular product procedure or advice as constituting a specific cure, whether palliative or ameliorative. Procedures and products mentioned are designed to support the client’s health and may be considered as support for other procedures deemed necessary by the practitioner. Although specific manufacturers make the supplements, herbs and homeopathies referenced in this document, the opinions expressed are those of the author and are not those of any of the manufacturers. This document is not designed to replace medical advice or medical treatments, but to be used adjunctively in the care and support of health and vitality. 9 © Copyright 2005 Return to Table of Contents . CHAPTER II: SUGAR HANDLING BLOOD SUGAR STABILIZATION RELATED CONDITIONS • Hypoglycemia PROTOCOL AT A GLANCE • Reactive Hypoglycemia • Low blood sugar Primary Supplemental Support • Syndrome X Bio-Glycozyme Forte • Triglycerides high Biomega-3 • Carbohydrate sensitivity Secondary Supplemental Support • Pre-diabetic Whey Protein Isolate • B vitamin deficiency Amino Acid Quick Sorb • Sugar sensitivity Beta-TCP • Food cravings ADHS Cytozyme-PAN • Carbohydrate cravings Cytozyme-LV Cytozyme-AD PHYSIOLOGIC CONSIDERATIONS Tri-Chol Blood sugar problems begin in childhood with excess use of sugary snacks and drinks. This is extremely common today. The U.S. Department of Agriculture estimates that the average American consumes from 150 to 180 pounds of sugar each year––an unbelievable amount compared to two or three hundred years ago when normal sugar consumption was one to five pounds per year. -

Inflammatory Mechanisms Affecting the Lipid Profile in Patients with Systemic Lupus Erythematosus CECILIA P
Inflammatory Mechanisms Affecting the Lipid Profile in Patients with Systemic Lupus Erythematosus CECILIA P. CHUNG, ANNETTE OESER, JOSEPH SOLUS, INGRID AVALOS, TEBEB GEBRETSADIK, AYUMI SHINTANI, MacRAE F. LINTON, SERGIO FAZIO, and C. MICHAEL STEIN ABSTRACT. Objective. Increased low density lipoprotein (LDL) cholesterol and triglycerides, and decreased high density lipoprotein (HDL) cholesterol concentrations are associated with adverse cardiovascular risk in the general population. Patients with systemic lupus erythematosus (SLE) have an altered lipid profile characterized by increased triglycerides and decreased HDL cholesterol concentrations. We examined the relationships between lipid concentrations, cytokines, and inflammatory markers in patients with SLE. Methods. Fasting lipid concentrations, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) were measured in 110 patients with SLE. Disease activity was quantified by the SLE Disease Activity Index (SLEDAI), and disease damage by the Systemic Lupus International Collaborating Clinics (SLICC) score. Concentrations of circulating tumor necrosis factor-α (TNF-α), interleukin 6 (IL-6), and insulin were measured and insulin sensitivity calculated. Results. Lower concentrations of HDL cholesterol were independently associated with higher ESR (p < 0.001), IL-6 (p = 0.02), SLEDAI (p = 0.04), and TNF-α (p = 0.04) after adjustment for age, sex, race, body mass index, insulin sensitivity, and current use of corticosteroids or hydroxychloroquine. Triglyceride concentrations were