District Health Action Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![THE JAMMU and KASHMIR CONDUCT of ELECTION RULES, 1965 Notification SRO 133, Dated 14Th June, 1965, Law Department] [As Amended by SRO 391, Dated 29.9.2014]](https://docslib.b-cdn.net/cover/9916/the-jammu-and-kashmir-conduct-of-election-rules-1965-notification-sro-133-dated-14th-june-1965-law-department-as-amended-by-sro-391-dated-29-9-2014-19916.webp)
THE JAMMU and KASHMIR CONDUCT of ELECTION RULES, 1965 Notification SRO 133, Dated 14Th June, 1965, Law Department] [As Amended by SRO 391, Dated 29.9.2014]
THE JAMMU AND KASHMIR CONDUCT OF ELECTION RULES, 1965 Notification SRO 133, dated 14th June, 1965, Law Department] [As Amended by SRO 391, dated 29.9.2014] In exercise of the powers conferredCONDUCT by section OF ELECTION 168C of theRULES, Jammu 1965 and Kashmir Representation of the People Act, 1957 and in supersession of the Jammu and Kashmir Representation of the People (Conduct of Elections and Election Petitions) Rules, 1957, the Government, after consulting the Election Commission, hereby makes the following rules, namely:- PART I PRELIMINARY 1. Short title and commencement (1) These rules may be called the Jammu and Kashmir ConductRule of 1 Election Rules, 1965. (2) They shall come into force at once. 2. Interpretation (1) In these rules, unless the context otherwise requires,— Rule 2 (a) "Act" means the Jammu and Kashmir Representation of the People Act, 1957; (b) "ballot box" includes any box, bag or other receptacle used for the insertion of ballot paper by voters; 1[(bb) "counterfoil" means the counterfoil attached to a ballot paper printed under the provisions of these rules]; (c) "election by assembly members" means an election to the Legislative Council by the members of the Legislative Assembly; (d) "elector" in relation to an election by Assembly Members, means any person entitled to vote at that election; (e) "electoral roll" in relation to an election by Assembly Members, means the list maintained under section 154 by the Returning Officer for that election; 1 Inserted vide SRO-5 dated 8-1-1972. 186 Rule 2 CONDUCT OF -

Page1 Final.Qxd (Page 2)
daily Follow us: Daily Excelsior JAMMU, WEDNESDAY, OCTOBER 7, 2020 REGD. NO. JK-71/18-20 Vol No. 56 12 Pages ` 5.00 ExcelsiorRNI No. 28547/65 No. 278 Pharmacists' issue resolved; Municipalities to have Ward Committees 10 die of COVID in Kashmir LG pays surprise visit to GMC Fayaz Bukhari MHA notifies adaptation of 11 more Central SRINAGAR, Oct 6: Ten 448 test +ve COVID-19 positive patients after he was admitted there. Jammu, enquires patient care today succumbed in Kashmir A 26-year-old man from Excelsior Correspondent sibility. He directed the con- gen as on date. Laws, 10 amended State Acts in J&K UT taking the death toll in Jammu Kargil died at SKIMS Soura cerned officers to rationalise the During the visit, the Lt and Kashmir to 1272 while where he was admitted today. JAMMU, Oct 6: resources and resolve the preva- Governor was accompanied by 448 people tested positive in Lieutenant Governor, Manoj Mohinder Verma for interpretation of laws in Union Territory. Among others, the other vic- lent issues. He also directed that, Chief Secretary, BVR the Valley taking the number tims from the Valley include a Sinha paid a surprise visit to 'senior doctors should attend to Subrahmanyam; Financial force in the territory of India. The 11 Central Laws which of such cases in J&K to 80,476. Government JAMMU, Oct 6: Union have been adapted are the 75-year-old man from The provisions of these A 70-year-old woman, a 33- Medical College Ministry of Home Affairs Pharmacy Act, 1948; the Alochibagh area of Srinagar, a orders shall not render invalid year-old man and mother and Jammu today and (MHA) has issued orders for Banning of Unregulated Deposit 65-year-old woman from Mir any notification, order, commit- son duo from Dalgate area of took stock of the adaptation of 11 more Central Schemes Act, 2019; the Danter and an 82-year-old from ment, attachment, bye-law, rule Srinagar died of COVID-19 in medicare services Laws and 10 amended Acts of Building and Other Construction Chogul Handwara in district or regulation duly made or SMHS hospital today. -

Jammu & Kashmir Reorganisation Act 2019
jftLVªh lañ Mhñ ,yñ—(,u)04@0007@2003—19 REGISTERED NO. DL—(N)04/0007/2003—19 vlk/kkj.k EXTRAORDINARY Hkkx II — [k.M 1 PART II — Section 1 izkf/kdkj ls izdkf'kr PUBLISHED BY AUTHORITY lañ 53] ubZ fnYyh] 'kqØokj] vxLr 9] [email protected] 18] 1941 ¼'kd½ No. 53] NEW DELHI, FRIDAY, AUGUST 9, 2019/SHRAVANA 18, 1941 (SAKA) bl Hkkx esa fHkUu i`"B la[;k nh tkrh gS ftlls fd ;g vyx ladyu ds :i esa j[kk tk ldsA Separate paging is given to this Part in order that it may be filed as a separate compilation. MINISTRY OF LAW AND JUSTICE (Legislative Department) New Delhi, the 9th August, 2019/Shravana 18, 1941 (Saka) The following Act of Parliament received the assent of the President on the 9th August, 2019, and is hereby published for general information:— THE JAMMU AND KASHMIR REORGANISATION ACT, 2019 NO. 34 OF 2019 [9th August, 2019.] An Act to provide for the reorganisation of the existing State of Jammu and Kashmir and for matters connected therewith or incidental thereto. BE it enacted by Parliament in the Seventieth Year of the Republic of India as follows:— PART-I PRELIMINARY 1. This Act may be called the Jammu and Kashmir Reorganisation Act, 2019. Short title. 2. In this Act, unless the context otherwise requires,— Definitions. (a) “appointed day” means the day which the Central Government may, by notification in the Official Gazette, appoint; (b) “article” means an article of the Constitution; (c) “assembly constituency” and “parliamentary constituency” have the same 43 of 1950. -

Directory Establishment
DIRECTORY ESTABLISHMENT SECTOR :URBAN STATE : JAMMU & KASHMIR DISTRICT : Anantnag Year of start of Employment Sl No Name of Establishment Address / Telephone / Fax / E-mail Operation Class (1) (2) (3) (4) (5) NIC 2004 : 0121-Farming of cattle, sheep, goats, horses, asses, mules and hinnies; dairy farming [includes stud farming and the provision of feed lot services for such animals] 1 DEPARTMENT OF ANIMAL HUSBANDRY NAZ BASTI ANTNTNAG OPPOSITE TO SADDAR POLICE STATION ANANTNAG PIN CODE: 2000 10 - 50 192102, STD CODE: NA , TEL NO: NA , FAX NO: NA, E-MAIL : N.A. NIC 2004 : 0122-Other animal farming; production of animal products n.e.c. 2 ASSTSTANT SERICULTURE OFFICER NAGDANDY , PIN CODE: 192201, STD CODE: NA , TEL NO: NA , FAX NO: NA, E-MAIL : N.A. 1985 10 - 50 3 INTENSIVE POULTRY PROJECT MATTAN DTSTT. ANANTNAG , PIN CODE: 192125, STD CODE: NA , TEL NO: NA , FAX NO: 1988 10 - 50 NA, E-MAIL : N.A. NIC 2004 : 0140-Agricultural and animal husbandry service activities, except veterinary activities. 4 DEPTT, OF HORTICULTURE KULGAM TEH KULGAM DISTT. ANANTNAG KASHMIR , PIN CODE: 192231, STD CODE: NA , 1969 10 - 50 TEL NO: NA , FAX NO: NA, E-MAIL : N.A. 5 DEPTT, OF AGRICULTURE KULGAM ANANTNAG NEAR AND BUS STAND KULGAM , PIN CODE: 192231, STD CODE: NA , 1970 10 - 50 TEL NO: NA , FAX NO: NA, E-MAIL : N.A. NIC 2004 : 0200-Forestry, logging and related service activities 6 SADU NAGDANDI PIJNAN , PIN CODE: 192201, STD CODE: NA , TEL NO: NA , FAX NO: NA, E-MAIL : 1960 10 - 50 N.A. 7 CONSERVATOR LIDDER FOREST CONSERVATOR LIDDER FOREST DIVISION GORIWAN BIJEHARA PIN CODE: 192124, STD CODE: 1970 10 - 50 DIVISION NA , TEL NO: NA , FAX NO: NA, E-MAIL : N.A. -

Characterization of Wastewater in Rajouri Town, Jammu and Kashmir, India
Zishan Aslam et al. Int. Journal of Engineering Research and Applications www.ijera.com ISSN: 2248-9622, Vol. 5, Issue 10, (Part - 2) October 2015, pp.69-79 RESEARCH ARTICLE OPEN ACCESS Characterization of Wastewater in Rajouri Town, Jammu And Kashmir, India Zishan Aslam*, Yawar Mushtaq Raina**, Irfan Mohiuddin*** *(Assistant Professor, Department of Civil Engineering, CoET, BGSB University Rajouri, J & K) ** (Junior Engineer, Public Works (R & B) Department, Government of Jammu & Kashmir, India) *** (B-Tech Civil engineering, BGSB University Rajouri, J & K) ABSTRACT Water exaggerated physically, chemically as well as biologically is known as wastewater. Thrown away process of solid waste and its treatment has been the foremost environmental setback for most of the cities in India especially in rural area. To make people aware about the level of contaminants in wastewater and to suggest the ways of treatment of wastewater which will result in disposing off of domestic effluents without any danger to human health, a study on characteristics of wastewater in Rajouri town in Jammu and Kashmir was conducted. Concentrations of various physicochemical parameters like Total dissolved solids (TDS), pH, Turbidity, Biochemical Oxygen Demand (BOD), Chemical Oxygen Demand(COD), Alkalinity, Hardness Chloride Content, Nitrogen, Ammonium, Phosphorous, Iron and E-coli bacteria were determined. Study was done on five different sampling locations. All the parameters were found to be generally exceeding the limits set by W.H.O except for few sampling locations. The sampling site which was found to be the most polluted was Muradpur (SL 5) thus affecting the population there because of being on the downstream side and the least affected site was Kheora (SL2). -

The Jammu and Kashmir Reorganisation Bill, 2019
1 AS PASSED BY THE RAJYA SABHA ON THE 5TH A UGUST, 2019 Bill No. XXIX-C of 2019 THE JAMMU AND KASHMIR REORGANISATION BILL, 2019 (AS PASSED BY THE RAJYA SABHA) A BILL to provide for the reorganisation of the existing State of Jammu and Kashmir and for matters connected therewith or incidental thereto. BE it enacted by Parliament in the Seventieth Year of the Republic of India as follows:— PART-I PRELIMINARY 1. This Act may be called the Jammu and Kashmir Reorganisation Act, 2019. Short title. 5 2. In this Act, unless the context otherwise requires,— Definitions. (a) “appointed day” means the day which the Central Government may, by notification in the Official Gazette, appoint; (b) “article” means an article of the Constitution; (c) “assembly constituency” and “parliamentary constituency” have the same 43 of 1950. 10 meanings as in the Representation of the People Act, 1950 (43 of 1950); (d) “Election Commission” means the Election Commission appointed by the President under article 324; (e) “existing State of Jammu and Kashmir” means the State of Jammu and Kashmir as existing immediately before the appointed day, comprising the territory which 2 immediately before the commencement of the Constitution of India in the Indian State of Jammu and Kashmir; (f) “law” includes any enactment, ordinance, regulation, order, bye-law, rule, scheme, notification or other instrument having, immediately before the appointed day, the force of law in the whole or in any part of the existing State of Jammu and Kashmir; 5 (g) “Legislative Assembly” means -
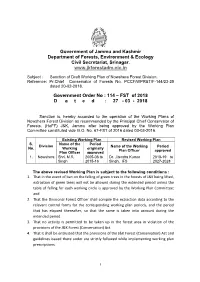
Sanction of Draft Working Plan of Nowshera Forest Division. Reference: Pr.Chief Conservator of Forests No
Government of Jammu and Kashmir Department of Forests, Environment & Ecology Civil Secretariat, Srinagar. www.jkforestadm.nic.in Subject : Sanction of Draft Working Plan of Nowshera Forest Division. Reference: Pr.Chief Conservator of Forests No. PCCF/WPR&T/F-144/23-25 dated 20-02-2018. Government Order No : 114 – FST of 2018 D a t e d : 27 - 03 - 2018 Sanction is, hereby accorded to the operation of the Working Plans of Nowshera Forest Division as recommended by the Principal Chief Conservator of Forests, (HoFF) J&K, Jammu after being approved by the Working Plan Committee constituted vide G.O. No. 67-FST of 2016 dated 03-03-2016. Existing Working Plan Revised Working Plan S. Name of the Period Division Name of the Working Period No. Working originally Plan Officer approved Plan Officer approved 1. Nowshera Shri. M.R. 2005-06 to Dr. Jitendra Kumar 2018-19 to Singh 2015-16 Singh, IFS 2027-2028 The above revised Working Plan is subject to the following conditions : 1. That in the event of ban on the felling of green trees in the forests of J&K being lifted, extraction of green trees will not be allowed during the extended period unless the table of felling for each working circle is approved by the Working Plan Committee; and 2. That the Divisional Forest Officer shall compile the extraction data according to the relevant control forms for the corresponding working plan periods, and the period that has elapsed thereafter, so that the same is taken into account during the extended period. 3. -

Census of India 1981
CENSUS OF INDIA 1981 SERIES-8 JAMMU & KASHMIR Special Paper of 1981 VILLAGE / TOWN WISE POPULATION AND SCHEDULED CASTE POPULATION ABDUL GANI Joint Dil ector of Census Operations Jammu and Kashmir PREFACE This is a special publication presenting the 1981 Census total popu lation and scheduled caste population of the State, districts and Tehsils down to village/urban block level to meet the requirement of data users interested in figures of population at village/ward level. This requirement could have been served by the 1981 District Census Handbooks which contain comprehensive basic information about populatIon by sex including literacy and work partici pation but the printing and publication of these handbooks which is the respon sibility of the State government will take some time. Until these handbooks are published, it is hoped that the present volume will serve a useful purpose to feed the urgent requirement of all data users. The Director of Census Opserations Shri A. H. Khan, under whose guidance the entire census operations were carried out, deserve all cred it for the success of the operations but he had to leave the organisation because of superannuation before this paper could be made ready for the press. I must record my deepest sense of gratitude to Shri V.S. Verma, Registrar General, India and Shri V.P. Pandey, Joint Registrar General, IndIa for their valuable guidance and for having agreed to bring out this specIal paper even in deviation of the approved census publications programme and arrange for its printing on a priority basis through the Printing Divi~ion of the Registrar General's Office under the supervision of Shri Tirath Dass, Joint Director. -

Page1final.Qxd (Page 2)
daily Follow us: Daily Excelsior JAMMU, MONDAY, AUGUST 9, 2021 REGD. NO. JK-71/21-23 Vol No. 57 12 Pages ` 5.00 ExcelsiorRNI No. 28547/65 No. 219 NIA searches 56 premises of Jamaat in 14 J&K distts JeI cadre charged with motivating Kashmiri youth to indulge in disruptive activities Doc, Govt teacher, Retd teachers 4 former heads also raided Biggest ever crackdown among those raided in Jammu against JeI in Kashmir Sanjeev Pargal *Funds raised by outfit Fayaz Bukhari JAMMU, Aug 8: The National channelized to HM, LeT Investigation Agency (NIA) today SRINAGAR, Aug 8: The National Investigation Agency (NIA) today carried conducted raids at 56 locations spread over 14 districts of Jammu and Kashmir on out the biggest ever crackdown in Kashmir against Jamat-e-Islami leaders in a ter- residences, premises and other locations of proscribed Jamaat-e-Islami (JeI) leaders ror funding case. and activists following reports that despite ban imposed on the organization its Four former heads of the activists were indulging in collection of donations which were being used for violent banned religious organization and secessionist activities and were motivating youth were among those raided in *Watch video on of Kashmir to indulge in disruptions. Kashmir. www.excelsiornews.com Following raids, the NIA detained district president The raids were conducted this of Jamaat-e-Islami for Kishtwar and recovered large morning after several NIA teams quantity of incriminating documents, electronic devices and mobile telephones from other arrived in Srinagar for the last 10 places which were raided during the day. At all the places, the NIA teams were joined in days and they had booked around Surrounded with lush green hills and clouds hovering over the sky, a view of Bhaderwah the operation by CRPF and Jammu and Kashmir Police to ensure that there was no unto- 140 vehicles for carrying out town on Sunday. -

Aadhaar Enrolment Enabled Business Units
S.No Center Location 1 J&K Bank BU:Shalamar Road Block:Jammu ,district:Jammu 2 J&K Bank BU:Gandhi Nagar Block:Jammu ,district:Jammu 3 J&K Bank BU:Patel Nagar Block:Jammu ,district:Jammu 4 J&K Bank BU:Channi Himmat Block:Jammu ,district:Jammu 5 J&K Bank BU:Akhnoor Block:Akhnoor,district:Jammu 6 J&K Bank BU:Durga Nagar Block:jammu,district:Jammu 7 J&K Bank BU:Sidhra Block:Dansal ,district:Jammu 8 J&K Bank BU:Nagrota Block:Dansal ,district:Jammu 9 J&K Bank BU:Arnia Block:Bishnah,district:Jammu 10 J&K Bank BU:Khour Block:Khour,district:Jammu 11 J&K Bank BU:Bari brahamna Block:Bari Brahmna ,district:Samba 12 J&K Bank BU:Samba main Block:Samba ,district:Samba 13 J&K Bank BU:Dayalachak Block:Hiranagar,district:KATHUA 14 J&K Bank BU:Phinter Block:Bilawar,district:KATHUA 15 J&K Bank BU:Basoli Block:Basholi,district:KATHUA 16 J&K Bank BU:Kalibari Block:Hiranagar,district:KATHUA 17 J&K Bank BU:Doda Main Block:Doda ,district:Doda 18 J&K Bank BU: Seri Block:Thatri ,district:Doda 19 J&K Bank BU:Hidyal Block:Kishtwar ,district:Doda 20 J&K Bank BU:Kuleed Block:Kishtwar ,district:Doda 21 J&K Bank BU: Tethar Block:Banihal ,district:Doda 22 J&K Bank BU: Maitra Ramban Block:Ramban ,district:Ramban 23 J&K Bank BU: Cama Housing Colony Udhampur, Block:Udhampur ,district:Udhampur 24 J&K Bank BU:SMM Ramnagar,Udhampur Block:Udhampur ,district:Udhampur 25 J&K Bank BU: Rehambal, Udhampur Block:Udhampur,district:Udhampur 26 J&K Bank BU: Arli Katra, Reasi Block:Katra ,district:Reasi 27 J&K Bank BU: DC Office Reasi Block:Reasi ,district:Reasi 28 J&K Bank BU: Kheora -

Fresh Spurt in COVID Cases As 708 Test Positive In
9thyear of publication SRINAGAR OBSERVER J&K ERA Starts Work On Rs 9.67 Crore Ensure hassle free services to the people “Commissioner SMC directs Advisor Khan Inspects Progress Of “Rigid Concrete Pavement” Works Of Sports Facilities At Srinagar Jammu and Kashmir Economic Reconstruction Agency Commissioner Srinagar Municipal Corporation Mr Gazanfar Ali today today started work on Rs 9.16 crore “Rigid Concrete reviewed Mohharam UL Haram arrangements in Shia populated areas Advisor to Lieutenant Governor, Farooq Khan took stock of Pavement “of Civil –Secretariat to Rambagh Chowk at Shalimar , Chandpora, Harwan , Lashkare Mohhalla , Hasnabad and progress of sports infrastructure development works at road. The work on the sub-project being executed under several other adjoining Areas. Mr Ali who visited these | Page 03 Multipurpose Indoor Sports Hall Polo Ground and Water Sports World Bank funded JTFRP (Jhelum Tawi Flood | Page 07 Center Nehru Park here today. During his visit to | Page 05 THURSDAY, AUGUST 20, 2020 29, Zil Hajj 1441 Hijri Published from Srinagar RNI No:JKENG/2012/43267 Vol:9 Issue No: 190 Pages:8 Rs.5.00 epaper: www.srinagarobserver.com BRIEFNEWS 3 Militants Labourer drowns to Fresh Spurt in COVID Cases death in Pulwama Killed in Twin PULWAMA: A 20-year-old labourer was on Wednesday drowned to death while extracting sand from river As 708 Test Positive In J&K Kashmir Gunfights Jhelum in South Kashmir district of Pulwama. An official told a local news Jehangeer Ganai gathering agency that a group of men 15 More Die of were extracting sand from Jhelum in boats at Karnabal Kakapora area of SRINAGAR: Jammu and COVID in Valley, Pulwama on Wednesday. -

Camscanner 06-30-2021 15.10
Government of Jammu & Kashmir, Finance Department (Development Expenditure Division-I) ******* Minutes of District Plan (Capex) meeting for the Financial Year 2021-22 held under the Chairmanship of Hon'ble Lieutenant Governor, UT of J&K. Hon'ble Lieutenant Governor Sh. Manoj Sinha chaired the 2nd District Plan (Capex) meeting on 16.06.2021 at 11.00 AM. All the Advisors to Hon'ble Lieutenant Governor, J&K, Chief Secretary/Financial Commissioner (Finance), J&K, all DDC Chairpersons, all the Administrative Secretaries, Divisional Commissioners Jammu/Kashmir besides all DDCs and other senior officers participated in the meeting. Dr. A.K Mehta, IAS, Chief Secretary/Financial Commissioner (Finance), J&K welcomed all the participants to the historic meeting for approval of District Plans (Capex) after implementation of three tier Panchayati Raj System in the Union Territory. He complimented all the DDC chairpersons and other elected representatives of the Panchayati Raj Institutions for formulating the plan despite the constraints due to Covid-19 pandemic. He referred to the quantum jump in the outlay of current years' Plan i.e. 12600.58 Crore which is more than double than the last year's Plan size. In the inaugural remarks Hon'ble Lieutenant Governor referred to 16.06.2021 as historic day as three tier Panchayati Raj System has been duly implemented and all Panchayats/BDCs/DDCs have actively participated in the Plan formulation process. The chair informed the DDCs/BDCs/Panchayats that they have now a bigger role to play in the development of the Districts. The Hon'ble Lieutenant Governor, while highlighting key features of District Capex Budget, observed that the plan has been prepared through public/ PRls participation with focus on rapid rise in the standard of living of the people, ensuring better roads, potable 1 I Scanned with CamScanner water and electricity, creation of opportunities of employment, exploring Tourism Potential and empowerment of the youth.