Psychedelic Effects of Psilocybin Correlate with Serotonin 2 a Receptor Occupancy and Plasma Psilocin Levels
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hallucinogens - LSD, Peyote, Psilocybin, and PCP
Hallucinogens - LSD, Peyote, Psilocybin, and PCP Hallucinogenic compounds found in some • Psilocybin (4-phosphoryloxy-N,N- plants and mushrooms (or their extracts) dimethyltryptamine) is obtained from have been used—mostly during religious certain types of mushrooms that are rituals—for centuries. Almost all indigenous to tropical and subtropical hallucinogens contain nitrogen and are regions of South America, Mexico, and classified as alkaloids. Many hallucinogens the United States. These mushrooms have chemical structures similar to those of typically contain less than 0.5 percent natural neurotransmitters (e.g., psilocybin plus trace amounts of acetylcholine-, serotonin-, or catecholamine- psilocin, another hallucinogenic like). While the exact mechanisms by which substance. hallucinogens exert their effects remain • PCP (phencyclidine) was developed in unclear, research suggests that these drugs the 1950s as an intravenous anesthetic. work, at least partially, by temporarily Its use has since been discontinued due interfering with neurotransmitter action or to serious adverse effects. by binding to their receptor sites. This DrugFacts will discuss four common types of How Are Hallucinogens Abused? hallucinogens: The very same characteristics that led to • LSD (d-lysergic acid diethylamide) is the incorporation of hallucinogens into one of the most potent mood-changing ritualistic or spiritual traditions have also chemicals. It was discovered in 1938 led to their propagation as drugs of abuse. and is manufactured from lysergic acid, Importantly, and unlike most other drugs, which is found in ergot, a fungus that the effects of hallucinogens are highly grows on rye and other grains. variable and unreliable, producing different • Peyote is a small, spineless cactus in effects in different people at different times. -

Hallucinogens - LSD, Peyote, Psilocybin, and PCP
Information for Behavioral Health Providers in Primary Care Hallucinogens - LSD, Peyote, Psilocybin, and PCP What are Hallucinogens? Hallucinogenic compounds found in some plants and mushrooms (or their extracts) have been used— mostly during religious rituals—for centuries. Almost all hallucinogens contain nitrogen and are classified as alkaloids. Many hallucinogens have chemical structures similar to those of natural neurotransmitters (e.g., acetylcholine-, serotonin-, or catecholamine-like). While the exact mechanisms by which hallucinogens exert their effects remain unclear, research suggests that these drugs work, at least partially, by temporarily interfering with neurotransmitter action or by binding to their receptor sites. This InfoFacts will discuss four common types of hallucinogens: LSD (d-lysergic acid diethylamide) is one of the most potent mood-changing chemicals. It was discovered in 1938 and is manufactured from lysergic acid, which is found in ergot, a fungus that grows on rye and other grains. Peyote is a small, spineless cactus in which the principal active ingredient is mescaline. This plant has been used by natives in northern Mexico and the southwestern United States as a part of religious ceremonies. Mescaline can also be produced through chemical synthesis. Psilocybin (4-phosphoryloxy-N, N-dimethyltryptamine) is obtained from certain types of mushrooms that are indigenous to tropical and subtropical regions of South America, Mexico, and the United States. These mushrooms typically contain less than 0.5 percent psilocybin plus trace amounts of psilocin, another hallucinogenic substance. PCP (phencyclidine) was developed in the 1950s as an intravenous anesthetic. Its use has since been discontinued due to serious adverse effects. How Are Hallucinogens Abused? The very same characteristics that led to the incorporation of hallucinogens into ritualistic or spiritual traditions have also led to their propagation as drugs of abuse. -

Activation of 5-HT2C (But Not 5-HT1A) Receptors in the Amygdala Enhances Fear-Induced Antinociception: Blockade with Local 5-HT2C Antagonist Or Systemic fluoxetine
Neuropharmacology 135 (2018) 376e385 Contents lists available at ScienceDirect Neuropharmacology journal homepage: www.elsevier.com/locate/neuropharm Activation of 5-HT2C (but not 5-HT1A) receptors in the amygdala enhances fear-induced antinociception: Blockade with local 5-HT2C antagonist or systemic fluoxetine Lígia Renata Rodrigues Tavares a, b, Daniela Baptista-de-Souza a, c, * Azair Canto-de-Souza a, b, c, d, a Psychobiology Group, Department of Psychology/CECH- Federal University of Sao~ Carlos-UFSCar, Sao~ Carlos, Sao~ Paulo, 13565-905, Brazil b Joint Graduate Program in Physiological Sciences UFSCar/UNESP, Sao~ Carlos, Sao~ Paulo, 13565-905, Brazil c Neuroscience and Behavioral Institute-IneC, Ribeirao~ Preto, Sao~ Paulo, 14040-901, Brazil d Program in Psychology UFSCar, Sao~ Carlos, Sao~ Paulo, 13565-905, Brazil article info abstract Article history: It is well-known that the exposure of rodents to threatening environments [e.g., the open arm of the Received 17 August 2017 elevated-plus maze (EPM)] elicits pain inhibition. Systemic and/or intracerebral [e.g., periaqueductal gray Received in revised form matter, amygdala) injections of antiaversive drugs [e.g., serotonin (5-HT) ligands, selective serotonin 5 March 2018 reuptake inhibitors (SSRIs)] have been used to change EPM-open arm confinement induced anti- Accepted 6 March 2018 nociception (OAA). Here, we investigated (i) the role of the 5-HT and 5-HT receptors located in the Available online 13 March 2018 1A 2C amygdaloid complex on OAA as well as (ii) the effects of systemic pretreatment with fluoxetine (an SSRI) on the effects of intra-amygdala injections of 8-OH-DPAT (a 5-HT1A agonist) or MK-212 (a 5-HT2C agonist) Keywords: fi Amygdala on nociception in mice con ned to the open arm or enclosed arm of the EPM. -

Paradoxical Actions of the Serotonin Precursor 5-Hydroxytryptophan on the Activity of Identified Serotonergic Neurons in a Simple Motor Circuit
The Journal of Neuroscience, February 15, 2000, 20(4):1622–1634 Paradoxical Actions of the Serotonin Precursor 5-hydroxytryptophan on the Activity of Identified Serotonergic Neurons in a Simple Motor Circuit David J. Fickbohm and Paul S. Katz Department of Biology, Georgia State University, Atlanta, Georgia 30302 Neurotransmitter synthesis is regulated by a variety of factors, cated an increase in a putative 5-HT electrochemical signal yet the effect of altering transmitter content on the operation of during swim CPG activation. Paradoxically, the spiking activity neuronal circuits has been relatively unexplored. We used elec- of the serotonergic neurons decreased to a single burst at the trophysiological, electrochemical, and immunohistochemical onset of the rhythmic motor program, whereas the overall techniques to investigate the effects of augmenting the seroto- duration of the episode remained about the same. 5-HTP treat- nin (5-HT) content of identified serotonergic neurons embed- ment gradually reduced the rhythmicity of the CPG output. ded in a simple motor circuit. The dorsal swim interneurons Thus, more serotonin did not result in a more robust swim (DSIs) are serotonergic neurons intrinsic to the central pattern motor program, suggesting that serotonin synthesis must be generator (CPG) for swimming in the mollusc Tritonia diom- kept within certain limits for the circuit to function correctly and edea. As expected, treatment with the serotonin precursor indicating that altering neurotransmitter synthesis can have 5-hydroxytryptophan (5-HTP) increased the intensity of seroto- serious consequences for the output of neural networks. nin immunolabeling and enhanced the potency of synaptic and Key words: intrinsic neuromodulation; central pattern gener- modulatory actions elicited by the DSIs. -

Psilocybin Mushrooms Fact Sheet
Psilocybin Mushrooms Fact Sheet January 2017 What are psilocybin, or “magic,” mushrooms? For the next two decades thousands of doses of psilocybin were administered in clinical experiments. Psilocybin is the main ingredient found in several types Psychiatrists, scientists and mental health of psychoactive mushrooms, making it perhaps the professionals considered psychedelics like psilocybin i best-known naturally-occurring psychedelic drug. to be promising treatments as an aid to therapy for a Although psilocybin is considered active at doses broad range of psychiatric diagnoses, including around 3-4 mg, a common dose used in clinical alcoholism, schizophrenia, autism spectrum disorders, ii,iii,iv research settings ranges from 14-30 mg. Its obsessive-compulsive disorder, and depression.xiii effects on the brain are attributed to its active Many more people were also introduced to psilocybin metabolite, psilocin. Psilocybin is most commonly mushrooms and other psychedelics as part of various found in wild or homegrown mushrooms and sold religious or spiritual practices, for mental and either fresh or dried. The most popular species of emotional exploration, or to enhance wellness and psilocybin mushrooms is Psilocybe cubensis, which is creativity.xiv usually taken orally either by eating dried caps and stems or steeped in hot water and drunk as a tea, with Despite this long history and ongoing research into its v a common dose around 1-2.5 grams. therapeutic and medical benefits,xv since 1970 psilocybin and psilocin have been listed in Schedule I of the Controlled Substances Act, the most heavily Scientists and mental health professionals criminalized category for drugs considered to have a consider psychedelics like psilocybin to be “high potential for abuse” and no currently accepted promising treatments as an aid to therapy for a medical use – though when it comes to psilocybin broad range of psychiatric diagnoses. -

(DMT), Harmine, Harmaline and Tetrahydroharmine: Clinical and Forensic Impact
pharmaceuticals Review Toxicokinetics and Toxicodynamics of Ayahuasca Alkaloids N,N-Dimethyltryptamine (DMT), Harmine, Harmaline and Tetrahydroharmine: Clinical and Forensic Impact Andreia Machado Brito-da-Costa 1 , Diana Dias-da-Silva 1,2,* , Nelson G. M. Gomes 1,3 , Ricardo Jorge Dinis-Oliveira 1,2,4,* and Áurea Madureira-Carvalho 1,3 1 Department of Sciences, IINFACTS-Institute of Research and Advanced Training in Health Sciences and Technologies, University Institute of Health Sciences (IUCS), CESPU, CRL, 4585-116 Gandra, Portugal; [email protected] (A.M.B.-d.-C.); ngomes@ff.up.pt (N.G.M.G.); [email protected] (Á.M.-C.) 2 UCIBIO-REQUIMTE, Laboratory of Toxicology, Department of Biological Sciences, Faculty of Pharmacy, University of Porto, 4050-313 Porto, Portugal 3 LAQV-REQUIMTE, Laboratory of Pharmacognosy, Department of Chemistry, Faculty of Pharmacy, University of Porto, 4050-313 Porto, Portugal 4 Department of Public Health and Forensic Sciences, and Medical Education, Faculty of Medicine, University of Porto, 4200-319 Porto, Portugal * Correspondence: [email protected] (D.D.-d.-S.); [email protected] (R.J.D.-O.); Tel.: +351-224-157-216 (R.J.D.-O.) Received: 21 September 2020; Accepted: 20 October 2020; Published: 23 October 2020 Abstract: Ayahuasca is a hallucinogenic botanical beverage originally used by indigenous Amazonian tribes in religious ceremonies and therapeutic practices. While ethnobotanical surveys still indicate its spiritual and medicinal uses, consumption of ayahuasca has been progressively related with a recreational purpose, particularly in Western societies. The ayahuasca aqueous concoction is typically prepared from the leaves of the N,N-dimethyltryptamine (DMT)-containing Psychotria viridis, and the stem and bark of Banisteriopsis caapi, the plant source of harmala alkaloids. -
A Serotonin Receptor with a Possible Role in Joint Diseases
Anders Kling 5-HT2 A – a serotonin receptor with a possible role in joint diseases role with a possible receptor – a serotonin 5-HT2A – a serotonin receptor with a possible role in joint diseases Anders Kling Umeå University 2013 Umeå University Department of Pharmacology and Clinical Neuroscience New Serie 1547 Department of Pharmacology and Clinical Neurosciences Umeå University ISSN: 0346-6612 Umeå University, Sweden 2013 SE-901 87 Umeå, Sweden ISBN 978-91-7459-549-9 5-HT2A – a serotonin receptor with a possible role in joint diseases Anders Kling Institutionen för farmakologi och klinisk neurovetenskap, Klinisk farmakologi/ Department of Pharmacology and Clinical Neuroscience, Clinical Pharmacology Umeå universitet/ Umeå University Umeå 2013 Responsible publisher under swedish law: the Dean of the Medical Faculty This work is protected by the Swedish Copyright Legislation (Act 1960:729) ISBN: 978-91-7459-549-9 ISSN: 0346-6612 New series No: 1547 Elektronisk version tillgänglig på http://umu.diva-portal.org/ Tryck/Printed by: Print och Media, Umeå universitet Umeå, Sweden 2013 Innehåll/Table of Contents Innehåll/Table of Contents i Abstract iv Abbreviations vi List of studies viii Populärvetenskaplig sammanfattning ix 5-HT2A – en serotoninreceptor med möjlig betydelse för ledsjukdomar ix Introduction 1 The serotonin system 1 Serotonin 1 Serotonin receptors 2 The serotonin system and platelets 2 Serotonin receptor 5-HT2A 3 Localisation/expression of 5-HT2A receptors 3 Functions of the 5-HT2A receptor 4 Regulation of the 5-HT2A receptor -
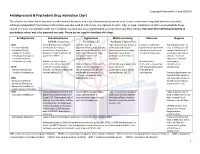
Antidepressant & Psychedelic Drug Interaction Chart
Copyright Psychedelic School 8/2020 Antidepressant & Psychedelic Drug Interaction Chart This chart is not intended to be used to make medical decisions and is for informational purposes only. It was constructed using data whenever possible, although extrapolation from known information was also used to inform risk. Any decision to start, stop, or taper medication and/or use psychedelic drugs should be made in conjunction with your healthcare provider(s). It is recommended to not perform any illicit activity. This chart the intellectual property of psychedelic school and is for personal use only. Please do not copy or distribute this chart. Antidepressant Phenethylamines Tryptamines MAOI-containing Ketamine Ibogaine -MDMA, mescaline -Psilocybin, LSD -Ayahuasca, Syrian Rue SSRIs Taper & discontinue at least 2 Consider taper & Taper & discontinue at least 2 Has been studied and Taper & discontinue at · Paroxetine (Paxil) weeks prior (all except discontinuation at least 2 weeks weeks prior (all except found effective both with least 2 weeks prior (all · Sertraline (Zoloft) fluoxetine) or 6 weeks prior prior (all except fluoxetine) or 6 fluoxetine) or 6 weeks prior and without concurrent except fluoxetine) or 6 · Citalopram (Celexa) (fluoxetine only) due to loss of weeks prior (fluoxetine only) (fluoxetine only) due to use of antidepressants weeks prior (fluoxetine · Escitalopram (Lexapro) psychedelic effect due to potential loss of potential risk of serotonin only) due to risk of · Fluxoetine (Prozac) psychedelic effect syndrome additive QTc interval · Fluvoxamine (Luvox) MDMA is unable to cause Recommended prolongation, release of serotonin when the Chronic antidepressant use may Life threatening toxicities can to be used in conjunction arrhythmias, or SPARI serotonin reuptake pump is result in down-regulation of occur with these with oral antidepressants cardiotoxicity · Vibryyd (Vilazodone) blocked. -

Serotonin Autoreceptors on Dorsal Raphe Neurons: Structure-Activity Relationships of Tryptamine Analogs’
0270.6474/81/0110-1148$o2.oo/0 The Journal of Neuroscience Copyright 0 Society for Neuroscience Vol. 1, No. 10, pp. 1148-1154 Printed in U.S.A. October 1981 SEROTONIN AUTORECEPTORS ON DORSAL RAPHE NEURONS: STRUCTURE-ACTIVITY RELATIONSHIPS OF TRYPTAMINE ANALOGS’ MICHAEL A. ROGAWSKI’ AND GEORGE K. AGHAJANIAN Departments of Pharmacology and Psychiatry, Yale University School of Medicine and the Connecticut Mental Health Center, New Haven, Connecticut 06510 Abstract A series of indole-ethylamines were tested for their ability to suppress the spontaneous firing of single dorsal raphe serotonergic neurons in the rat. The compounds were all derivatives of either tryptamine or N,N-dimethyltryptamine possessing hydroxy or methoxy substituents on the benzene ring portion of the indole nucleus. Their activity was assessed using quantitative microiontophoresis or following systemic (intravenous) administration. The serotonin autoreceptor or so-called “S2 receptor” mediating the inhibition of raphe serotonergic neurons was found to exhibit a high degree of structural specificity among the closely related tryptamine analogs. The following structure- activity rules were demonstrated: (1) for either hydroxy or methoxy derivatives, the relative favorability of the ring positions conforms to the series 5 >> 4 > 6; (2) methoxy derivatives are more sensitive to a shift of the ring substituent from the 5- to the 4- or 6-positions than are hydroxy compounds; and (3) activity is enhanced by N,N-dimethylation. Furthermore, addition of a methyl group at the 7-position of 5-methoxy-N,N-dimethyltryptamine markedly reduces the activity of this potent agonist. Of the radioligands which label brain serotonin receptors, the pharmacological characteristics of D-[“HIlysergic acid diethylamide binding best correspond to those displayed by the SZ receptor as determined in the present physiological analysis, although sufficient data are not yet available to make a complete comparison. -

Psychedelics: a Window to Mental Illness; Psilocybin and Depression
Nova Southeastern University NSUWorks College of Pharmacy Student Articles College of Pharmacy 7-22-2020 Psychedelics: A Window To Mental Illness; Psilocybin And Depression Kiomary Rivera Quintana [email protected] Follow this and additional works at: https://nsuworks.nova.edu/hpd_corx_stuarticles Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Rivera Quintana, Kiomary, "Psychedelics: A Window To Mental Illness; Psilocybin And Depression" (2020). College of Pharmacy Student Articles. 5. https://nsuworks.nova.edu/hpd_corx_stuarticles/5 This Literature Review is brought to you for free and open access by the College of Pharmacy at NSUWorks. It has been accepted for inclusion in College of Pharmacy Student Articles by an authorized administrator of NSUWorks. For more information, please contact [email protected]. 2020 Psychedelics: A Window to Mental Illness PSILOCYBIN AND DEPRESSION KIOMARY RIVERA QUINTANA STUDENT PHARMACIST CLASS OF 2022 PHRE 5223-DRUGS OF ABUSE NOVA SOUTHEASTERN UNIVERSITY INTRODUCTION Drug abuse is characterized by improper repeated use of drugs to seek outcomes such as pleasure, stress relief and an altered reality.1 It can lead to addiction, a severe form of substance use disorder (SUD) in which a person’s drug habits worsen and they become unable to control the impulse to use drugs despite knowing the negative consequences.1 In addition to drug seeking behavior, brain function also changes affecting the natural inhibition and reward centers. Use of and addiction to alcohol, nicotine, and illicit drugs costs the Nation more than $740 billion a year related to healthcare, crime, and lost productivity.1 Whether a person will abuse drugs or become addicted is influenced by multiple factors; the more risk factors a person has, the greater the chance. -

Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com Ce4less.Com
Hallucinogens And Dissociative Drug Use And Addiction Introduction Hallucinogens are a diverse group of drugs that cause alterations in perception, thought, or mood. This heterogeneous group has compounds with different chemical structures, different mechanisms of action, and different adverse effects. Despite their description, most hallucinogens do not consistently cause hallucinations. The drugs are more likely to cause changes in mood or in thought than actual hallucinations. Hallucinogenic substances that form naturally have been used worldwide for millennia to induce altered states for religious or spiritual purposes. While these practices still exist, the more common use of hallucinogens today involves the recreational use of synthetic hallucinogens. Hallucinogen And Dissociative Drug Toxicity Hallucinogens comprise a collection of compounds that are used to induce hallucinations or alterations of consciousness. Hallucinogens are drugs that cause alteration of visual, auditory, or tactile perceptions; they are also referred to as a class of drugs that cause alteration of thought and emotion. Hallucinogens disrupt a person’s ability to think and communicate effectively. Hallucinations are defined as false sensations that have no basis in reality: The sensory experience is not actually there. The term “hallucinogen” is slightly misleading because hallucinogens do not consistently cause hallucinations. 1 ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com How hallucinogens cause alterations in a person’s sensory experience is not entirely understood. Hallucinogens work, at least in part, by disrupting communication between neurotransmitter systems throughout the body including those that regulate sleep, hunger, sexual behavior and muscle control. Patients under the influence of hallucinogens may show a wide range of unusual and often sudden, volatile behaviors with the potential to rapidly fluctuate from a relaxed, euphoric state to one of extreme agitation and aggression. -

Lysergic Acid Diethylamide (LSD) Promotes Social Behavior Through Mtorc1 in the Excitatory Neurotransmission
Lysergic acid diethylamide (LSD) promotes social behavior through mTORC1 in the excitatory neurotransmission Danilo De Gregorioa,b,1, Jelena Popicb,2,3, Justine P. Ennsa,3, Antonio Inserraa,3, Agnieszka Skaleckab, Athanasios Markopoulosa, Luca Posaa, Martha Lopez-Canula, He Qianzia, Christopher K. Laffertyc, Jonathan P. Brittc, Stefano Comaia,d, Argel Aguilar-Vallese, Nahum Sonenbergb,1,4, and Gabriella Gobbia,f,1,4 aNeurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, QC, Canada, H3A 1A1; bDepartment of Biochemistry, McGill University, Montreal, QC, Canada, H3A 1A3; cDepartment of Psychology, McGill University, Montreal, QC, Canada, H3A 1B1; dDivision of Neuroscience, Vita Salute San Raffaele University, 20132 Milan, Italy; eDepartment of Neuroscience, Carleton University, Ottawa, ON, Canada, K1S 5B6; and fMcGill University Health Center, Montreal, QC, Canada, H3A 1A1 Contributed by Nahum Sonenberg, November 10, 2020 (sent for review October 5, 2020; reviewed by Marc G. Caron and Mark Geyer) Clinical studies have reported that the psychedelic lysergic acid receptor (6), but also displays affinity for the 5-HT1A receptor diethylamide (LSD) enhances empathy and social behavior (SB) in (7–9). Several studies have demonstrated that LSD modulates humans, but its mechanism of action remains elusive. Using a glutamatergic neurotransmission and, indirectly, the α-amino- multidisciplinary approach including in vivo electrophysiology, 3-hydroxy-5-methyl-4-isoxazole propionate (AMPA) receptors. optogenetics, behavioral paradigms, and molecular biology, the Indeed, in vitro studies have shown that LSD increased the ex- effects of LSD on SB and glutamatergic neurotransmission in the citatory response of interneurons in the piriform cortex following medial prefrontal cortex (mPFC) were studied in male mice.