Images from Prototype MVCT Scanner in Cobalt-60 Beam
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Oncologist, Tom Baker Cancer Centre Department of Oncology, Calgary Cancercontrol Alberta, Alberta Health Services
MEDICAL ONCOLOGIST, TOM BAKER CANCER CENTRE DEPARTMENT OF ONCOLOGY, CALGARY CANCERCONTROL ALBERTA, ALBERTA HEALTH SERVICES The Department of Oncology, Cumming School of Medicine, University of Calgary in conjunction with Cancer Control, Alberta Health Services, invite applications for a full-time academic clinician/clinician scientist within the discipline of Medical Oncology at the Assistant Professor level or higher. The successful applicant will become a member of a multidisciplinary cancer program located at the Tom Baker Cancer Centre and the Foothills Hospital site of the Calgary Zone and will join a team of 23 Medical Oncologists. Special training and/or a record of academic success in areas such as epidemiology, clinical trials, investigational new drug development, translational research and/or health services research would be desirable. The Tom Baker Cancer Centre, a component of a provincial program of cancer control is the tertiary referral centre and the main cancer treatment, research and education facility for southern Alberta. Approximately 7,000 new patients are seen each year at the Centre in state-of-the-art facilities. Radiation services for southern Alberta are provided at TBCC by 18 Radiation Oncologists, and facilities include 9 linear accelerators, CT simulation, intensity modulated radiotherapy, brachytherapy, and stereotactic capabilities. The Provincial Bone Marrow Transplant program is also delivered in Calgary. Postgraduate training programs in Medical Oncology and other oncology disciplines (Radiation, Gynecological, Surgical, Hematology, and Palliative Care) are fully accredited by the RCPSC. The TBCC has a very active clinical research program, including in-house investigator lead, cooperative groups, (such as the CCTG and N.R.G. (N.S.A.B.P., R.T.O.G., G.O.G.)), and industry trials. -

Locum Medical Oncologist, Tom Baker Cancer Centre Department of Oncology, Calgary Cancercontrol Alberta, Alberta Health Services
LOCUM MEDICAL ONCOLOGIST, TOM BAKER CANCER CENTRE DEPARTMENT OF ONCOLOGY, CALGARY CANCERCONTROL ALBERTA, ALBERTA HEALTH SERVICES The Department of Oncology, Cumming School of Medicine, University of Calgary in conjunction with Cancer Control, Alberta Health Services, invite applications for a LOCUM TENENS within the section of Medical Oncology. The successful applicant will become a member of a multidisciplinary cancer program located at the Tom Baker Cancer Centre and the Foothills Hospital site of the Calgary Zone and will join a team of 23 Medical Oncologists. The Tom Baker Cancer Centre, a component of a provincial program of cancer control is the tertiary referral centre and the main cancer treatment, research and education facility for southern Alberta. Approximately 7,000 new patients are seen each year at the Centre in state-of-the-art facilities. Postgraduate training programs in Medical Oncology and other oncology disciplines (Radiation, Gynecological, Surgical, Hematology, and Palliative Care) are fully accredited by the RCPSC. The TBCC has a very active clinical research program, including in-house investigator lead, cooperative groups, (such as the CCTG and N.R.G. (N.S.A.B.P., R.T.O.G., G.O.G.)), and industry trials. Radiation services for southern Alberta are provided at TBCC by 21 Radiation Oncologists, and facilities include 9 linear accelerators, CT simulation, intensity modulated radiotherapy, brachytherapy, and stereotactic capabilities. The Provincial Bone Marrow Transplant program is also delivered in Calgary The Calgary Health Zone comprises four teaching hospitals situated in the City of Calgary, and serves residents of Southern Alberta, and portions of British Columbia and Saskatchewan. -

Hospital Services in Alberta – General Hospital (Active Treatment /Acute Care) JULY 2018
Alberta Health, Health Facilities Planning Branch For General Reference Purposes Only Hospital Services In Alberta – General Hospital (Active Treatment /Acute Care) JULY 2018 Hospital Services in Alberta – JULY 2018 General Hospital (Active Treatment / Acute Care) Auxiliary Hospital (Chronic/ Long Term Care) Alberta Health Services (AHS) New Zones: Zone 1 – South [ ] Zone 2 – Calgary [ ] Zone 3 – Central [ ] Zone 4 – Edmonton [ ] Zone 5 – North [ ] Legend: (1) Hospital Legal Name: Name appearing on M.O. #10/2011, as amended by M.O.s #10/2013, #42/2013, #33/2014, #31/2015 referencing the Consolidated Schedule of Approved Hospitals (CSAH). (2) Operator Type: Regional Health Authority (AHS) or Voluntary (VOL) (3) Operator Identity: Corporate organization name of the “hospital service operator”. (4) Sub-Acute Care (SAC): Some hospitals (highlighted) also operate a registered SAC service. Disclaimer: This list is compiled from registration information documented by the department as certified by Alberta Health Services (AHS). Facilities on the list may also provide health services or programs other than approved hospital services. This list is amended from time to time, as certified by Alberta Health Services, but may not be complete/accurate when it is read. Questions regarding specific facilities appearing on this list should be directed to Alberta Health Services. © 2018 Government of Alberta Page 1 of 24 Alberta Health, Health Facilities Planning Branch For General Reference Purposes Only Hospital Services In Alberta – General -

THE Neem)R Sports 10 Vol
LETHBRIDQE CoMMUNny COUEQE This Week Surfln'83 2 Weekenders 8 Mixology 9 THE NEeM)R Sports 10 Vol. xvn-No. 14 Thursday, January 27, 1983 I Comic City 12 Provincial grants reduced Coiiege facing cutbacics LCC may receive only a five per cent in back of some sort and we don't know He says LCC could look at cutting staff "Occasionally additional money is crease in provincial grants this year, says where that will be," says Cooper. since 80 per cent of the operating costs are given to an institution to set up a new pro the vice-presklent of administration. "Last year LCC received a 14.6 per cent spent on suff salaries. gram, so it may end up with more than a Dean Cooper bates his predicdon on a increase in provincial grants. This year "Our first priority is education. The Five per cent increase all together." recent statement from provincial there is a significant change." last thing we want to cut is the quality of Although city school systenu can seek ueasurer, Lou Hyndman, that post- The 20 to 25 per cent increased cost of education." local funding beyond the five per cent, ad secondary institutions shouldn't expecl utilities presenu a problem for LCC. Cooper says the provincial government vanced education does not have the taxing more than a seven per cent increase. Cooper says this means an area of the col geiKrally gives the same percenuge in authority. "This is very disappointing to me. It lege will face a cutback of the same crease to post-secondary institutions "There is no altemative. -

Arnie Charbonneau Cancer Institute VISION 2022
Arnie Charbonneau Cancer Institute VISION 2022 MESSAGE FROM THE DIRECTOR, ARNIE CHARBONNEAU CANCER INSTITUTE The Arnie Charbonneau Cancer Institute is meeting the cancer challenge by enabling research that spans the patient journey, from primary cancer prevention to life after cancer, and all health research pillars. The Arnie Charbonneau Cancer Institute is a university-based institute that conducts and supports cancer research. Members of the Institute are located in the Faculties of Science, Social Science, Engineering, Nursing, in the Cumming School of Medicine and its academic departments, in the Tom Baker Cancer Centre, and in our teaching hospitals. The Institute’s mission is to ‘meet the cancer challenge’, a challenge that is simultaneously biological, diagnostic, therapeutic, personal, and societal. We address this challenge by supporting research that spans the patient journey, from primary cancer prevention to life after cancer, and that spans the biomedical, clinical, health services, and population health research pillars of the Canadian Institutes of Health Research (CIHR). Three themes guide our strategy: accelerating cancer control, improving the lives of patients with cancer, and reducing the burden of cancer in Alberta and beyond. Building research partnerships, fostering a research culture, enhancing competitiveness, supporting recruitment, training the next generation of cancer researchers, building infrastructure and research programs, and connecting with the community of Calgary, are some of the ways in which the Institute will address these goals to ‘meet the cancer challenge’ and add unique value. J. Gregory Cairncross, MD, FRSC Director, Arnie Charbonneau Cancer Institute Professor, Clinical Neurosciences University of Calgary Page | 1 EXECUTIVE SUMMARY One of seven health research institutes at the University of Calgary, the Arnie Charbonneau Cancer Institute supports cancer research of all types. -

Department of Surgery - Surgical Sections
Department of Surgery - Surgical Sections Zone Clinical Section Chief Phone Fax Address Other Links Dentistry & Oral Health Foothills Medical Centre - Dental Clinic - Adult North Tower 10th Floor Dr. Graham Cobb 403-271-1665 403-278-9944 - Dental Clinic – Public Health 1403 29 St. NW - Pediatric Dental Clinic Calgary, Alberta T2N 2T9 General Surgery Foothills Medical Centre - General Surgery Residency Training North Tower, 10th Floor Dr. Tony MacLean 403- 944-1509 403-270-8431 Program 1403 29 St. NW - Colorectal Surgery Residency Program Calgary, Alberta T2N 2T9 Ophthalmology Dr. Andrew Crichton (Interim) 403-943-3932 - Ophthalmology Residency Program Oral and Maxillofacial Surgery Dr. Richard Edwards 403-244-3678 403-228-7833 #702, 2303 - 4 Street SW Calgary, AB T2S 2S7 Orthopaedic Surgery 3330 Hospital Drive NW - Orthopaedic Surgery Dr. Jason Werle 403-210-7478 403-221-4310 Calgary Alberta T2N 4N1 - Orthopaedics Residency Training Program Otolaryngology Richmond Road Diagnostic Treatment Centre ENT Clinic RM 21304E Dr. Douglas Bosch 403-955-9059 403-955-8779 1820 Richmond Rd SW - Otolaryngology Residency Program Calgary, Alberta T2T 5C7 Pediatric Surgery Alberta Children's Hospital 2888 Shaganappi Trail NW Dr. Frankie Fraulin 403-955-7392 403-955-7634 - Pediatric Surgery Residency Program Calgary, Alberta T3B 6A8 Zone Clinical Section Chief Phone Fax Address Other Links Plastic Surgery Foothills Medical Centre Main Building, Rm 382 Dr. Rob Harrop 403-944-4317 403-944-2840 1403 29 St NW - Plastic Surgery Residency Program Calgary, Alberta T2N 2T9 Podiatric Surgery CBI Health Centre-Sunridge 2675 - 36 Street NE Dr. Francois Harton 403-250-3010 403-221-8356 Calgary, Alberta T2G 5B6 Surgical Oncology Tom Baker Cancer Centre 1331 - 29 St. -

Fitness Centre Location and Directions
Fitness Centre Location and Directions Fitness Centre Directions Hours of Operation Alberta Children’s Hospital (ACH) • From the staff door on the Lower Level (LL) by the bike racks Open 24 hours/day Room A0417 OR 7 days/week 2888 Shaganappi Trail NW • On the main level by the cafeteria, go through the LL north 365 days/year through the restricted access doorway, past the mailroom. TURN LEFT, by the change rooms. The last door on the left is the fitness centre. Foothills Medical Centre (FMC) • From the SSB Main Entrance: TURN LEFT by the gift shop. Open 24 hours/day Room AGW7A • Follow the hallway towards the Tom Baker Cancer Centre 7 days/week Special Services Building (SSB) through the double automatic doors. 365 days/year 1403 29 Street NW • Take the first set of stairs to the right, down to the ground level to the atrium w/blue ceramic walls. • Continue straight ahead to the end of the atrium. Peter Lougheed Centre (PLC) • From the West Entrance, at the information desk TURN LEFT, Open 24 hours/day Room 19103 down the hall past Second Cup. The fitness centre is at the 7 days/week 3500 26 Ave NE end of the hall on your right. 365 days/year • Change rooms with day use lockers are located on your left. Rockyview General Hospital (RGH) • From the Highwood Cafeteria at level #3, walk past the park- Open 24 hours/day Room 3N33 ing and elevators, TURN RIGHT. Walk past another set of el- 7 days/week 7007 14 Street SW evators (on your left) to the end of the hallway (the mailroom 365 days/year is directly in front of you). -

Newsletters from 2009 to 2015
news Volume 17 Number 1 February 2015 “Building the smallest democracies at the heart of society.” The United Nations: The International Year of the Family, 1994 Agreement# 40063171 Experiences of Men Who Attended Domestic Violence Treatment Programs and Made Changes to End Violence in Their Intimate Relationships by Crystal Giesbrecht y Master of Social Work thesis behaviour, and recognition that research study at the University the cause of their violence and the Mof Regina (summarized in changes that they had to make were a presentation at RESOLVE Research internal, not external. Realization that Day 2014), sought to understand the changes that needed to happen experiences of men who were were within themselves gave the men violent in their intimate relationships, agency to do something about the attended domestic violence treatment problem. programs, and successfully made The men’s descriptions of their changes toward an end of their violent formative years included the notion behaviour. Phenomenological research of typical masculine behaviour; they methods were used to conduct in– spoke of growing up with the idea depth qualitative interviews with four that being a man meant not showing men who attended Domestic Abuse/ their emotions. Getting in touch with Violence Treatment Programs (DAVTPs) Crystal Giesbrecht their emotions helped the men to and made changes to their behaviour. be successful in the DAVTPs and to make positive While not all men who attend DAVTPs make changes in many of their relationships, not just in changes, a change among even a few participants their intimate partnerships. makes a substantial difference in the lives of women and children. -

TBCC) in Calgary Is Seeking a Radiation Oncologists Interested in a 0.5 FTE (Permanent) Position
RADIATION ONCOLOGIST DEPARTMENT OF ONCOLOGY TOM BAKER CANCER CENTRE, CALGARY CANCERCONTROL ALBERTA, AHS The Tom Baker Cancer Centre (TBCC) in Calgary is seeking a Radiation Oncologists interested in a 0.5 FTE (permanent) position. An additional 0.5 FTE is guaranteed for 2 years. The successful applicant will become a member of a multidisciplinary cancer program located at the Tom Baker Cancer Centre and the Foothills Hospital site of the Calgary Zone and will join an existing team of 23 Radiation Oncologists, several of whom work part time. The TBCC is a full-service, academic cancer centre with 8 linear accelerators, orthovoltage and HDR capability. There are active gyne, prostate and breast brachytherapy programs. A new, full service, 109,000 m2 cancer centre with 15 linac vaults (12 to be filled at opening), an MRI-equipped brachytherapy suite, an MR simulator, a PET/CT simulator and 160 inpatient beds, will be operational by 2023-24. TBCC includes the provincial Alberta Radiosurgery Centre and expanding programs for lung, liver and spine SBRT. In 2018, faculty provided over 4700 consultations. There are close interdisciplinary working relationships with Medical, Surgical, Gynecologic, Hematologic and Psychosocial Oncology, Palliative Care, and Medical Physics. There are strong research links with the Arnie Charbonneau Cancer Institute at the University of Calgary. A full complement of ancillary staff and services are available. Clinical trials and translational research programs are augmented by an annual, centre-specific, Investigator Initiated Trial grant competition. The University of Calgary’s Radiation Oncology Residency Training and post-residency fellowship programs compliment post-graduate training programs in Surgical, Medical, Gynecologic, Hematologic, Palliative and Psychosocial Oncology. -
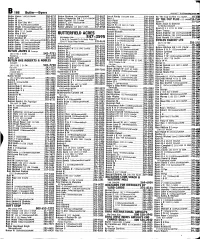
B KS S; I N Michael
1 B 166 Butler—Byers 000102 ^ TELUS AdvertisingStnim21 Butler Vance 1601bl8AvNW 284-4717 Buttar Resham 24CastleglenWyNE 293--8627 Buuck Randy 2601a48 StSE 272-1063 By The Cup Coffee 736 8AvSW 233-2718 Butler W 272-2191 Buttco Properties Ltd l 920 69AvSW253-3474 Buur J 230-2047 BY THE CUP PLUS 633 6Avsw234-7544 Butler W RR4 274-9522 Butte George 232 27AvNW 277-1947 Buur Peter 280-8340 Butler W Fax Line RR4 274-2424 Byam D 217-1135 Buttee C 509 73GlamisDrSW 313-1285 Buur Peter 285-3263 Byam Jesse & Daelene '. ' Butler W G 4104DoverbrookRdSE 272-1883 Buttee William 248-7627 Buur R H 110 1415 17 StSE 269-1415 124 McKerrellGdnsSE 257-539? Butler Wade 52DougiasRidgeCloseSE 236-1704 Butter Johann 919 808 5 StSE 237-0948 Buwalda EIke 239-2332 Byam R L 4 1931 31 StSW 246-527» Butler William 204 8948ElbowDrSW 640-4207 Buwalda J 7739BowcliffeCrNW 288-2902 Butler Wm 2113 2AvNW 283-4606 Buxom Blondes 276-5429 Byam Tracey 686-9587 Butler Wm J RR4 274-9360 BUTTERFIELD ACRES Buxton C 242-2978 Byard Andrew 205 l027CameronAvSW.802-133f Butler Y Computer 208-9465 Buxton David S l03HolmwoodAvNW 289-9661 Byard Andrew 205 1027CameronAvSW.802-1337 Butler-Gretton M 247-3795 Information Line 547-3595 Buxton F 94 ShawbrookeCrSW 256-4785 Byatt Harold 235 lOAvNE 276-9681 ButlerToGo 502 105 150CrowfootCrNW815-9668 3 Km N Of Crowchild Tr On Rocky Ridge Rd BVBLOS BAKERY LTD ;• 254077 Rocky Ridge Rd NW 239-0638 Buxton F 94 ShawbrookeCrSW 873-0728 Butlin Greg lOOCoralSpringsMewNE 590-4143 Buxton G & I ...640-9639 2479 23 StNE 250-3711 Butlin James 224WoodsideBaySW 238-0987 -

APL Memo- Calgary Zone Outpatient Lab Closures in Acute Sites
MEMORANDUM DATE: April 15, 2020 TO: All Calgary Zone Clinical Trial and Research Study Teams FROM: Alberta Precision Laboratories RE: Urban Hospital Outpatient Labs KEY MESSAGES: Effective Thursday, April 16 the outpatient labs located at Alberta Children’s Hospital (ACH), Peter Lougheed Centre (PLC), Rockyview General Hospital (RGH) and South Health Campus (SHC) will be closed. Patients will be re-directed to community Patient Service Centres. Staff will be deployed as appropriate. The safety of vulnerable patient populations and staff in the urban hospitals is a priority as we respond to the COVID-19 pandemic. Closing outpatient laboratory collections within urban acute care sites will reduce the number of individuals entering these facilities, limiting the risk of COVID-19 transmission. An APL memo was distributed on March 25th, 2020 strongly recommending physicians cease ordering routine or non- essential lab work. This has already reduced volumes of patients attending outpatient collection locations. The postponement of elective surgery combined with the closure of most ambulatory clinics has already resulted in a decreased need for outpatient lab service. Re-directing lab collections for ambulatory and outpatients to community PSCs will limit traffic into acute care sites and allow for more appropriate physical distancing. ACTION REQUIRED AND COLLECTION PROCESS: Patients who continue to attend remaining ambulatory clinics at the hospital will have their urgent laboratory blood work collected by the onsite phlebotomy team. Tom Baker Cancer Centre patients will continue to receive service in the Special Services Building (SSB) outpatient lab at Foothills Medical Center (FMC) which will remain open. Clinical Trial and Research Study Patients who require KIT/ Research collections originally collected from an Urban Hospital Outpatient Lab will be redirected to go to the SSB Outpatient Lab located at the FMC. -

The University of Calgary Department of Oncology/Alberta Cancer Foundation Fellowship Positions for 2018-19
The University of Calgary Department of Oncology/Alberta Cancer Foundation Fellowship Positions for 2018-19. The Department of Oncology at the University of Calgary in conjunction with the Alberta Cancer Foundation (ACF) and other donors, is pleased to offer six fellowships for the academic year 2018-19. Of the six, four are awarded in an open competition format, and two are site specific awards. The site specific fellowships are in Gynecologic Oncology (Lillian Koch fellowship) and Sarcoma (Cameron Daye fellowship). APPLICATIONS are open to all trainees who have completed core training in an oncology discipline and are seeking to enhance their clinical and/or research skills. THERE IS A LARGE PATIENT POPULATION in Calgary, Alberta, Canada which will help our fellows enhance their clinical skills. Fellows will be trained under direct supervision of leading specialists in oncology. Training will take place at the Tom Baker Cancer Centre, Foothills Medical Centre or Alberta Children’s hospital, depending on the focus of the fellowship. SCHOLARLY ACTIVITY is a requirement for fellows, and projects may be clinical, health policy, or translational research related. There is a strong research association through the Arnie Charbonneau Cancer Institute as well as excellent population health and epidemiologic research support available. ALL RESIDENCY PROGRAMS in the Department of Oncology are fully accredited through the Royal College of Physicians and Surgeons of Canada, thus ensuring an excellent training atmosphere for multi-disciplinary cancer research and outstanding patient care. IN ACCORDANCE with Canadian immigration requirements, preference will be given to Canadian citizens or permanent residents of Canada. The University of Calgary respects, appreciates, and honours diversity.