Exploring Alternative Therapeutic Interventions for the Treatment of Leigh Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NDUFAF1 Antibody
Efficient Professional Protein and Antibody Platforms NDUFAF1 Antibody Basic information: Catalog No.: UPA63763 Source: Rabbit Size: 50ul/100ul Clonality: monoclonal Concentration: 1mg/ml Isotype: Rabbit IgG Purification: Protein A purified. Useful Information: WB:1:1000 ICC:1:50-1:200 Applications: IHC:1:50-1:200 FC:1:50-1:100 Reactivity: Human Specificity: This antibody recognizes NDUFAF1 protein. Immunogen: Synthetic peptide within C terminal human NDUFAF1. This gene encodes a complex I assembly factor protein. Complex I (NADH-ubiquinone oxidoreductase) catalyzes the transfer of electrons from NADH to ubiquinone (coenzyme Q) in the first step of the mitochondrial respiratory chain, resulting in the translocation of protons across the inner mitochondrial membrane. The encoded protein is required for assembly of complex I, and mutations in this gene are a cause of mitochondrial complex I deficiency. Alternatively spliced transcript variants have been observed for Description: this gene, and a pseudogene of this gene is located on the long arm of chromosome 19. Part of the mitochondrial complex I assembly (MCIA) com- plex. The complex comprises at least TMEM126B, NDUFAF1, ECSIT, and ACAD9. Interacts with ECSIT. Interacts with ACAD9. At early stages of com- plex I assembly, it is found in intermediate subcomplexes that contain dif- ferent subunits including NDUFB6, NDUFA6, NDUFA9, NDUFS3, NDUFS7, ND1, ND2 and ND3 Uniprot: Q9Y375 Human BiowMW: 38 kDa Buffer: 1*TBS (pH7.4), 1%BSA, 50%Glycerol. Preservative: 0.05% Sodium Azide. Storage: Store at 4°C short term and -20°C long term. Avoid freeze-thaw cycles. Note: For research use only, not for use in diagnostic procedure. -

Molecular Mechanism of ACAD9 in Mitochondrial Respiratory Complex 1 Assembly
bioRxiv preprint doi: https://doi.org/10.1101/2021.01.07.425795; this version posted January 9, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Molecular mechanism of ACAD9 in mitochondrial respiratory complex 1 assembly Chuanwu Xia1, Baoying Lou1, Zhuji Fu1, Al-Walid Mohsen2, Jerry Vockley2, and Jung-Ja P. Kim1 1Department of Biochemistry, Medical College of Wisconsin, Milwaukee, Wisconsin, 53226, USA 2Department of Pediatrics, University of Pittsburgh School of Medicine, University of Pittsburgh, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA 15224, USA Abstract ACAD9 belongs to the acyl-CoA dehydrogenase family, which catalyzes the α-β dehydrogenation of fatty acyl-CoA thioesters. Thus, it is involved in fatty acid β-oxidation (FAO). However, it is now known that the primary function of ACAD9 is as an essential chaperone for mitochondrial respiratory complex 1 assembly. ACAD9 interacts with ECSIT and NDUFAF1, forming the mitochondrial complex 1 assembly (MCIA) complex. Although the role of MCIA in the complex 1 assembly pathway is well studied, little is known about the molecular mechanism of the interactions among these three assembly factors. Our current studies reveal that when ECSIT interacts with ACAD9, the flavoenzyme loses the FAD cofactor and consequently loses its FAO activity, demonstrating that the two roles of ACAD9 are not compatible. ACAD9 binds to the carboxy-terminal half (C-ECSIT), and NDUFAF1 binds to the amino-terminal half of ECSIT. Although the binary complex of ACAD9 with ECSIT or with C-ECSIT is unstable and aggregates easily, the ternary complex of ACAD9-ECSIT-NDUFAF1 (i.e., the MCIA complex) is soluble and extremely stable. -
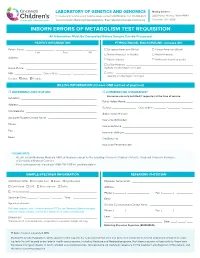
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

Genes Investigated
BabyNEXTTM EXTENDED Investigated genes and associated diseases Gene Disease OMIM OMIM Condition RUSP gene Disease ABCC8 Familial hyperinsulinism 600509 256450 Metabolic disorder - ABCC8-related Inborn error of amino acid metabolism ABCD1 Adrenoleukodystrophy 300371 300100 Miscellaneous RUSP multisystem (C) * diseases ABCD4 Methylmalonic aciduria and 603214 614857 Metabolic disorder - homocystinuria, cblJ type Inborn error of amino acid metabolism ACAD8 Isobutyryl-CoA 604773 611283 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of (S) ** organic acid metabolism ACAD9 acyl-CoA dehydrogenase-9 611103 611126 Metabolic Disorder - (ACAD9) deficiency Inborn error of fatty acid metabolism ACADM Acyl-CoA dehydrogenase, 607008 201450 Metabolic Disorder - RUSP medium chain, deficiency of Inborn error of fatty (C) acid metabolism ACADS Acyl-CoA dehydrogenase, 606885 201470 Metabolic Disorder - RUSP short-chain, deficiency of Inborn error of fatty (S) acid metabolism ACADSB 2-methylbutyrylglycinuria 600301 610006 Metabolic Disorder - RUSP Inborn error of (S) organic acid metabolism ACADVL very long-chain acyl-CoA 609575 201475 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of fatty (C) acid metabolism ACAT1 Alpha-methylacetoacetic 607809 203750 Metabolic Disorder - RUSP aciduria Inborn error of (C) organic acid metabolism ACSF3 Combined malonic and 614245 614265 Metabolic Disorder - methylmalonic aciduria Inborn error of organic acid metabolism 1 ADA Severe combined 608958 102700 Primary RUSP immunodeficiency due -

An Essential Role for ECSIT in Mitochondrial Complex I Assembly and Mitophagy in Macrophages
Article An Essential Role for ECSIT in Mitochondrial Complex I Assembly and Mitophagy in Macrophages Graphical Abstract Authors Fla´ via R.G. Carneiro, Alice Lepelley, John J. Seeley, Matthew S. Hayden, Sankar Ghosh Correspondence [email protected] In Brief Macrophages rely on fine-tuning their metabolism to fulfill their anti-bacterial functions. Carneiro et al. show that the complex I assembly factor ECSIT is an essential regulator of the balance between mitochondrial respiration and glycolysis and the maintenance of a healthy mitochondrial pool through mitophagy. Highlights d Loss of ECSIT in macrophages leads to a striking glycolytic shift d ECSIT is essential for complex I assembly and stability in macrophages d Role of ECSIT in mROS production and removal of damaged mitochondria by mitophagy Carneiro et al., 2018, Cell Reports 22, 2654–2666 March 6, 2018 ª 2018 The Author(s). https://doi.org/10.1016/j.celrep.2018.02.051 Cell Reports Article An Essential Role for ECSIT in Mitochondrial Complex I Assembly and Mitophagy in Macrophages Fla´ via R.G. Carneiro,1,3,4 Alice Lepelley,1,4 John J. Seeley,1 Matthew S. Hayden,1,2 and Sankar Ghosh1,5,* 1Department of Microbiology and Immunology, Vagelos College of Physicians and Surgeons, Columbia University, New York, NY 10032, USA 2Section of Dermatology, Department of Surgery, Dartmouth-Hitchcock Medical Center, Lebanon, NH 03756, USA 3FIOCRUZ, Center for Technological Development in Health (CDTS), Rio de Janeiro, Brazil 4These authors contributed equally 5Lead Contact *Correspondence: [email protected] https://doi.org/10.1016/j.celrep.2018.02.051 SUMMARY 2015). There, ECSIT-dependent mROS production promotes activation of the phagosomal nicotinamide adenine dinucleotide ECSIT is a mitochondrial complex I (CI)-associated phosphate (NADPH) oxidase system and ROS-dependent protein that has been shown to regulate the pro- killing of engulfed microbes (West et al., 2011). -

Genetic and Genomic Analysis of Hyperlipidemia, Obesity and Diabetes Using (C57BL/6J × TALLYHO/Jngj) F2 Mice
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Nutrition Publications and Other Works Nutrition 12-19-2010 Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P. Stewart Marshall University Hyoung Y. Kim University of Tennessee - Knoxville, [email protected] Arnold M. Saxton University of Tennessee - Knoxville, [email protected] Jung H. Kim Marshall University Follow this and additional works at: https://trace.tennessee.edu/utk_nutrpubs Part of the Animal Sciences Commons, and the Nutrition Commons Recommended Citation BMC Genomics 2010, 11:713 doi:10.1186/1471-2164-11-713 This Article is brought to you for free and open access by the Nutrition at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Nutrition Publications and Other Works by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. Stewart et al. BMC Genomics 2010, 11:713 http://www.biomedcentral.com/1471-2164/11/713 RESEARCH ARTICLE Open Access Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P Stewart1, Hyoung Yon Kim2, Arnold M Saxton3, Jung Han Kim1* Abstract Background: Type 2 diabetes (T2D) is the most common form of diabetes in humans and is closely associated with dyslipidemia and obesity that magnifies the mortality and morbidity related to T2D. The genetic contribution to human T2D and related metabolic disorders is evident, and mostly follows polygenic inheritance. The TALLYHO/ JngJ (TH) mice are a polygenic model for T2D characterized by obesity, hyperinsulinemia, impaired glucose uptake and tolerance, hyperlipidemia, and hyperglycemia. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

New Perspective in Diagnostics of Mitochondrial Disorders
Pronicka et al. J Transl Med (2016) 14:174 DOI 10.1186/s12967-016-0930-9 Journal of Translational Medicine RESEARCH Open Access New perspective in diagnostics of mitochondrial disorders: two years’ experience with whole‑exome sequencing at a national paediatric centre Ewa Pronicka1,2*, Dorota Piekutowska‑Abramczuk1†, Elżbieta Ciara1†, Joanna Trubicka1†, Dariusz Rokicki2, Agnieszka Karkucińska‑Więckowska3, Magdalena Pajdowska4, Elżbieta Jurkiewicz5, Paulina Halat1, Joanna Kosińska6, Agnieszka Pollak7, Małgorzata Rydzanicz6, Piotr Stawinski7, Maciej Pronicki3, Małgorzata Krajewska‑Walasek1 and Rafał Płoski6* Abstract Background: Whole-exome sequencing (WES) has led to an exponential increase in identification of causative vari‑ ants in mitochondrial disorders (MD). Methods: We performed WES in 113 MD suspected patients from Polish paediatric reference centre, in whom routine testing failed to identify a molecular defect. WES was performed using TruSeqExome enrichment, followed by variant prioritization, validation by Sanger sequencing, and segregation with the disease phenotype in the family. Results: Likely causative mutations were identified in 67 (59.3 %) patients; these included variants in mtDNA (6 patients) and nDNA: X-linked (9 patients), autosomal dominant (5 patients), and autosomal recessive (47 patients, 11 homozygotes). Novel variants accounted for 50.5 % (50/99) of all detected changes. In 47 patients, changes in 31 MD-related genes (ACAD9, ADCK3, AIFM1, CLPB, COX10, DLD, EARS2, FBXL4, MTATP6, MTFMT, MTND1, MTND3, MTND5, NAXE, NDUFS6, NDUFS7, NDUFV1, OPA1, PARS2, PC, PDHA1, POLG, RARS2, RRM2B, SCO2, SERAC1, SLC19A3, SLC25A12, TAZ, TMEM126B, VARS2) were identified. The ACAD9, CLPB, FBXL4, PDHA1 genes recurred more than twice suggesting higher general/ethnic prevalence. In 19 cases, variants in 18 non-MD related genes (ADAR, CACNA1A, CDKL5, CLN3, CPS1, DMD, DYSF, GBE1, GFAP, HSD17B4, MECP2, MYBPC3, PEX5, PGAP2, PIGN, PRF1, SBDS, SCN2A) were found. -

1 Cerebrospinal Fluid Neurofilament Light Is Associated with Survival In
1 Cerebrospinal fluid Neurofilament Light is associated with survival in mitochondrial disease patients Kalliopi Sofou†,a, Pashtun Shahim†, b,c, Már Tuliniusa, Kaj Blennowb,c, Henrik Zetterbergb,c,d,e, Niklas Mattssonf, Niklas Darina aDepartment of Pediatrics, University of Gothenburg, The Queen Silvia’s Children Hospital, Gothenburg, Sweden bInstitute of Neuroscience and Physiology, Department of Psychiatry and Neurochemistry, the Sahlgrenska Academy at University of Gothenburg, Mölndal, Sweden. cClinical Neurochemistry Laboratory, Sahlgrenska University Hospital, Mölndal, Sweden dDepartment of Molecular Neuroscience, UCL Institute of Neurology, Queen Square, London, UK eUK Dementia Research Institute at UCL, London, UK fClinical Memory Research Unit, Lund University, Malmö, Sweden, and Lund University, Skåne University Hospital, Department of Clinical Sciences, Neurology, Lund, Sweden †Equal contributors Correspondence to: Kalliopi Sofou, MD, PhD Department of Pediatrics University of Gothenburg, The Queen Silvia’s Children Hospital SE-416 85 Gothenburg, Sweden Tel: +46 (0) 31 3421000 E-mail: [email protected] Abbreviations Ab42 Amyloid-b42 AD Alzheimer’s disease AUROC Area under the receiver operating-characteristic curve CNS Central nervous system CSF Cerebrospinal fluid DWI Diffusion weighted imaging FLAIR Fluid attenuated inversion recovery GFAp Glial fibrillary acidic protein KSS Kearns-Sayre syndrome LP Lumbar puncture ME Mitochondrial encephalopathy Mitochondrial encephalomyopathy, lactic acidosis and MELAS stroke-like -

Drugs for Orphan Mitochondrial Disease
Drugs for Orphan Mitochondrial Disease Gino Cortopassi, CEO Ixchel:Mayan goddess of health www.ixchelpharma.com Davis, CA Executive Summary • Ixchel is a clinical stage company focused on developing IXC-109 as therapeutic for mitochondrial diseases: 109 increases mitochondrial activities in cells & mice. • XC-109 is an NCE prodrug of the active moiety Mono-methylfumarate (MMF) upon which a Composition-of-Matter patent has been applied for. • IP: rights to 5 patent families, including composition of matter, method of use, formulation and 2 granted orphan drug designations. • Efficacy: demonstrated efficacy in preclinical mouse models with IXC-109 in Leigh’s Syndrome, Friedreich’s ataxia cardiac defects. • Patient advocacy groups & KOLs: Ixchel developed a 10-year relationship with patient advocacy groups FARA, Ataxia UK, UMDF & MDA, and networks with 8 Key Opinion Leaders in Mitochondrial Research and Mitochondrial Disease clinical development • Proven path and comps – Valuation of other MMF prodrugs: Vumerity/Alkermes 8700, Xenoport/Dr. Reddy’s – Valuation of Reata FA – IXC-109 is pharmacokinetically superior to Biogen’s DMF and Vumerity 2 Ixchel’s pipeline in orphan mitochondrial disease Benefits in Benefits in Patient Cells Target Identified Orphan Mitochondrial: Mouse models POC clinical trial Friedreich’s Ataxia, IXC103 Leigh’s Syndrome, LHON Mitochondrial Myopathy, IXC109 Duchenne’s Muscular Dystrophy 3 Defects of mitochondria are inherited and cause disease Neurodegeneration Friedreich’s ataxia Mitochondrial defect Genetics Leber’s (LHON) Myopathy Leigh Syndrome Muscle Wasting MELAS 4 Friedreich’s Ataxia as mitochondrial disease target for therapy FA as an orphan therapeutic target: § FA is the most prevalent inherited ataxia: ~6000 in North America, 15,000 Europe. -

Understanding ACAD9 Function and the Physiologic Consequences of Its Deficiency
Title Page Understanding ACAD9 Function and the Physiologic Consequences of its Deficiency by Andrew Guelde Sinsheimer BA, Oberlin College, 2008 Submitted to the Graduate Faculty of the Department of Human Genetics Graduate School of Public Health in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2019 Committee Membership Page UNIVERSITY OF PITTSBURGH GRADUATE SCHOOL OF PUBLIC HEALTH This dissertation was presented by Andrew Guelde Sinsheimer It was defended on April 23, 2019 and approved by David Finegold, MD, Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh Eric S. Goetzman, PhD. Associate Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh Candace Kammerer, PhD, Associate Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh Dissertation Advisor: Jerry Vockley, MD, PhD, Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh ii Copyright © by Andrew Guelde Sinsheimer 2019 iii Abstract Jerry Vockley, MD, PhD Understanding ACAD9 Function and the Physiologic Consequences of its Deficiency Andrew Guelde Sinsheimer, PhD University of Pittsburgh, 2019 Abstract Acyl CoA Dehydrogenase 9 (ACAD9) is a member of the family of flavoenzymes that catalyze the dehydrogenation of Acyl-CoAs to 2,3 enoyl-CoAs in mitochondrial fatty acid oxidation (FAO). Inborn errors of metabolism of nearly all family members, including ACAD9, have been described in humans, and represent significant causes of morbidity and mortality particularly in children. ACAD9 deficiency leads to a combined defect in fatty acid oxidation and oxidative phosphorylation (OXPHOS) due to a duel role in the pathways. In addition to its function in mitochondrial FAO, ACAD9 has been shown to have a second function as one of 14 factors responsible for assembly of complex I of the electron transport chain (ETC). -

Clinical, Biochemical and Genetic Spectrum of 70 Patients with ACAD9
Clinical, biochemical and genetic spectrum of 70 patients with ACAD9 deficiency is riboflavin supplementation effective? Repp, Birgit M; Mastantuono, Elisa; Alston, Charlotte L; Schiff, Manuel; Haack, Tobias B; Rötig, Agnes; Ardissone, Anna; Lombès, Anne; Catarino, Claudia B; Diodato, Daria; Schottmann, Gudrun; Poulton, Joanna; Burlina, Alberto; Jonckheere, An; Munnich, Arnold; Rolinski, Boris; Ghezzi, Daniele; Rokicki, Dariusz; Wellesley, Diana; Martinelli, Diego; Wenhong, Ding; Lamantea, Eleonora; Ostergaard, Elsebet; Pronicka, Ewa; Pierre, Germaine; Smeets, Hubert J M; Wittig, Ilka; Scurr, Ingrid; de Coo, Irenaeus F M; Moroni, Isabella; Smet, Joél; Mayr, Johannes A; Dai, Lifang; de Meirleir, Linda; Schuelke, Markus; Zeviani, Massimo; Morscher, Raphael J; McFarland, Robert; Seneca, Sara; Klopstock, Thomas; Meitinger, Thomas; Wieland, Thomas; Strom, Tim M; Herberg, Ulrike; Ahting, Uwe; Sperl, Wolfgang; Nassogne, Marie-Cecile; Ling, Han; Fang, Fang; Freisinger, Peter; Van Coster, Rudy; Strecker, Valentina; Taylor, Robert W; Häberle, Johannes; Vockley, Jerry; Prokisch, Holger; Wortmann, Saskia Published in: Orphanet Journal of Rare Diseases DOI: 10.1186/s13023-018-0784-8 Publication date: 2018 Document version Publisher's PDF, also known as Version of record Document license: CC BY Citation for published version (APA): Repp, B. M., Mastantuono, E., Alston, C. L., Schiff, M., Haack, T. B., Rötig, A., Ardissone, A., Lombès, A., Catarino, C. B., Diodato, D., Schottmann, G., Poulton, J., Burlina, A., Jonckheere, A., Munnich, A., Rolinski, B., Ghezzi, D., Rokicki, D., Wellesley, D., ... Wortmann, S. (2018). Clinical, biochemical and genetic spectrum of 70 patients with ACAD9 deficiency: is riboflavin supplementation effective? Orphanet Journal of Rare Diseases, 13, [120]. https://doi.org/10.1186/s13023-018-0784-8 Download date: 28.