Esophagogastric Tamponade Tube Practice Guideline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Letters to the Editor
letters to the Editor Porphyria, Cardiopulmonary Bypass, and heart with additional hemorrhage into the pericardial sac (5). Peri- cardiocentesis, however, can be a temporizing measure in the se- Volatile Anesthetics verely compromised patient (4,7,8) until definitive surgical estab- lishment of a pericardial window. A pericardial window can be To the Editor: established under local anesthesia (9) via the subxiphoid or lateral We take issue with Stevens et al’s contentious statements in their thoracotomy approach (1,2,5,8,9). The subxiphoid approach is less discussion of volatile anesthetics in the patient with acute intermit- useful for trauma because limited surgical exposure may preclude tent porphyria undergoing mitral valve replacement (1). repair of cardiac wounds (2). However, a pericardial window dur- In the “pre-propofol” era, the safe and appropriate use of halo- ing awake lateral thoracotomy may be both poorly tolerated and thane and isoflurane in porphyric patients was established (2). dangerous in the distressed, moving patient (7). Recent reports of the successful use of isoflurane in porphyric A blunt trauma victim (2) recently presented for an emergent patients undergoing cardiac surgery also exist (3,4). As the authors surgical pericardial window for recurrent acute pericardial tampon- themselves allude to a report of elevated porphyrins after propofol ade. Although the patient was not hypotensive, jugular venous anesthesia in acute intermittent porphyria, favoring propofol over distention, pulsus paradoxus (1,3,7), patient distress (4), and echo- inhaled anesthetics because of the latter’s implied lack of a “safety cardiographic signs were present. As an alternative to endotracheal record” cannot be supported. -

Incidence, Risk Factors and Management of Severe Post-Transsphenoidal Epistaxis Q ⇑ Kenneth M
Journal of Clinical Neuroscience 22 (2015) 116–122 Contents lists available at ScienceDirect Journal of Clinical Neuroscience journal homepage: www.elsevier.com/locate/jocn Clinical Study Incidence, risk factors and management of severe post-transsphenoidal epistaxis q ⇑ Kenneth M. De Los Reyes a, Bradley A. Gross a, , Kai U. Frerichs a, Ian F. Dunn a, Ning Lin a, Jordina Rincon-Torroella a, Donald J. Annino b, Edward R. Laws a a Department of Neurological Surgery, Brigham and Women’s Hospital and Harvard Medical School, 75 Francis Street, Boston, MA, 02115, USA b Department of Otolaryngology, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, USA article info abstract Article history: Among the major complications of transsphenoidal surgery, less attention has been given to severe post- Received 16 June 2014 operative epistaxis, which can lead to devastating consequences. In this study, we reviewed 551 consec- Accepted 2 July 2014 utive patients treated over a 4 year period by the senior author to evaluate the incidence, risk factors, etiology and management of immediate and delayed post-transsphenoidal epistaxis. Eighteen patients (3.3%) developed significant postoperative epistaxis – six immediately and 12 delayed (mean postoper- Keywords: ative day 10.8). Fourteen patients harbored macroadenomas (78%) and 11 of 18 (61.1%) had complex Endoscopic nasal/sphenoid anatomy. In the immediate epistaxis group, 33% had acute postoperative hypertension. Epistaxis In the delayed group, one had an anterior ethmoidal pseudoaneurysm, and one had restarted anticoagu- Management Microscopic lation on postoperative day 3. We treated the immediate epistaxis group with bedside nasal packing fol- Pituitary lowed by operative re-exploration if conservative measures were unsuccessful. -

World Journal of Hepatology
World Journal of W J H Hepatology Submit a Manuscript: https://www.f6publishing.com World J Hepatol 2020 June 27; 12(6): 288-297 DOI: 10.4254/wjh.v12.i6.288 ISSN 1948-5182 (online) ORIGINAL ARTICLE Retrospective Cohort Study Hospital teaching status on the outcomes of patients with esophageal variceal bleeding in the United States Pavan Patel, Laura Rotundo, Evan Orosz, Faiz Afridi, Nikolaos Pyrsopoulos ORCID number: Pavan Patel Pavan Patel, Faiz Afridi, Nikolaos Pyrsopoulos, Division of Gastroenterology and Hepatology, (0000-0001-5682-4939); Laura Rutgers - New Jersey Medical School, Newark, NJ 07101-1709, United States Rotundo (0000-0002-4094-3682); Evan Orosz (0000-0003-2474-5501); Laura Rotundo, Evan Orosz, Department of Medicine, Rutgers - New Jersey Medical School, Faiz Afridi (0000-0002-0172-0486); Newark, NJ 07101-1709, United States Nikolaos Pyrsopoulos (0000-0002-6950-8174). Corresponding author: Nikolaos Pyrsopoulos, FACP, MD, PhD, Chief Doctor, Professor, Division of Gastroenterology and Hepatology, Rutgers – New Jersey Medical School, 185 S. Author contributions: Patel P Orange Avenue, MSB H-535, Newark, NJ 07101-1709, United States. provided conception and design of [email protected] the study, acquisition and analysis of data, and drafting of the manuscript; Rotundo L, Afridi F and Orosz E drafted the manuscript; Pyrsopoulos N Abstract contributed to the manuscript by BACKGROUND providing revision and oversight Acute variceal bleeding is a major complication of portal hypertension and is a of its writing. leading cause of death in patients with cirrhosis. There is limited data on the Institutional review board outcomes of patients with esophageal variceal bleeding in teaching versus statement: This study did not nonteaching hospitals. -

Femoral and Sciatic Nerve Blocks for Total Knee Replacement in an Obese Patient with a Previous History of Failed Endotracheal Intubation −A Case Report−
Anesth Pain Med 2011; 6: 270~274 ■Case Report■ Femoral and sciatic nerve blocks for total knee replacement in an obese patient with a previous history of failed endotracheal intubation −A case report− Department of Anesthesiology and Pain Medicine, School of Medicine, Catholic University of Daegu, Daegu, Korea Jong Hae Kim, Woon Seok Roh, Jin Yong Jung, Seok Young Song, Jung Eun Kim, and Baek Jin Kim Peripheral nerve block has frequently been used as an alternative are situations in which spinal or epidural anesthesia cannot be to epidural analgesia for postoperative pain control in patients conducted, such as coagulation disturbances, sepsis, local undergoing total knee replacement. However, there are few reports infection, immune deficiency, severe spinal deformity, severe demonstrating that the combination of femoral and sciatic nerve blocks (FSNBs) can provide adequate analgesia and muscle decompensated hypovolemia and shock. Moreover, factors relaxation during total knee replacement. We experienced a case associated with technically difficult neuraxial blocks influence of successful FSNBs for a total knee replacement in a 66 year-old the anesthesiologist’s decision to perform the procedure [1]. In female patient who had a previous cancelled surgery due to a failed tracheal intubation followed by a difficult mask ventilation for 50 these cases, peripheral nerve block can provide a good solution minutes, 3 days before these blocks. FSNBs were performed with for operations on a lower extremity. The combination of 50 ml of 1.5% mepivacaine because she had conditions precluding femoral and sciatic nerve blocks (FSNBs) has frequently been neuraxial blocks including a long distance from the skin to the used for postoperative pain control after total knee replacement epidural space related to a high body mass index and nonpalpable lumbar spinous processes. -
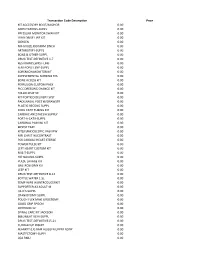
Transaction Code Description
Transaction Code Description Price KIT ACCESSORY BOOT/ANCHOR 0.00 AMPUTATIONS-SUPPL 0.00 PRESSURE MONITOR SWAN KIT 0.00 LVAD DRIVE LINE KIT 0.00 OXYGEN 0.00 NU-GAUZE,IODAFRM 1INCH 0.00 ARTHROTMY-SUPPL 0.00 BONE & OTHER-SUPPL 0.00 DRUG TEST-DEFINITIVE 1-7 0.00 RESTRAINTS,WRST-LMB 0.00 FEM-POPLIT.BYP-SUPPL 0.00 SORENSON MONITOR KIT 0.00 SUPPLEMENTAL NURSING SYS 0.00 BONE ACCESS KIT 0.00 PERFUSION CUSTOM PACK 0.00 PICC DRESSING CHANGE KIT 0.00 FOLLOLWUP 30 0.00 KIT PORTICO DELIVERY SYST 0.00 PACK,NASAL POST W/DRAWSTR 0.00 PLASTIC RECONS-SUPPL 0.00 COOL CATH TUBING KIT 0.00 CARDIAC ANESTHESIA SUPPLY 0.00 PORT-A-CATH-SUPPL 0.00 CARDINAL PAIN INJ KIT 0.00 BIOPSY TRAY 0.00 KIT(LF)ENDOSCOPIC VASVIEW 0.00 MRI CHEST W/CONTRAST 0.00 PCK CARDIAC HEART STERILE 0.00 POWER PULSE KIT 0.00 LEFT HEART CUSTOM KIT 0.00 M & T-SUPPL 0.00 HIP NAILING-SUPPL 0.00 PULSE LAVAGE KIT 0.00 GASTROSTOMY KIT 0.00 LEEP KIT 0.00 DRUG TEST-DEFINITIVE 8-14 0.00 BOTTLE WATER 1.5L 0.00 TEMP WIRE W/INTRODUCERKIT 0.00 SUPPORTER,A3 ADULT-M 0.00 I & D'S-SUPPL 0.00 CRANIOTOMY-SUPPL 0.00 POUCH FLEX MAXI UROSTOMY 0.00 GOOD GRIP SPOON 0.00 OXYHOOD 12- 0.00 SPINAL CARE KIT JACKSON 0.00 BI&UNILAT VEIN-SUPPL 0.00 DRUG TEST-DEFINITIVE15-21 0.00 CUDDLECUP INSERT 0.00 BLANKET (LF) BAIR HUGGER UPPER BODY 0.00 MASTECTOMY-SUPPL 0.00 LOA RMU 0.00 PACK LINQ 0.00 CHOLECYSTECTOM-SUPPL 0.00 RES BWL,SIG,AP-SUPPL 0.00 TRAY BIOPSY GENERAL UTIL 0.00 KIT(LF)CUSTOM SYRINGE ANGIO 0.00 OXISENSOR(LF)PEDI (PINK) 0.00 THORACIC SURG-SUPPL 0.00 NU-GAUZE PLAIN 1/2INCH 0.00 NU-GAUZE,IODAFRM 1/4INCH 0.00 PICC -

Progressive Mandibular Midline Deviation After Difficult Tracheal
Anaesthesia 2013 doi:10.1111/anae.12271 Case Report Progressive mandibular midline deviation after difficult tracheal intubation J. Mareque Bueno,1,2 M. Fernandez-Barriales,3 M. A. Morey-Mas4,5 and F. Hernandez-Alfaro6,7 1 Associate Professor, 6 Professor, Department of Oral and Maxillofacial Surgery, Universitat Internacional de Catalunya, Barcelona, Spain 2 Staff, 3 Visiting Resident, 7 Director, Institute of Maxillofacial Surgery, Teknon Medical Center, Barcelona, Spain 4 Staff, Department of Oral and Maxillofacial Surgery, Hospital Son Dureta, Palma de Mallorca, Illes Balears, Spain 5 Associate Professor, Especialidad Universitaria en Implantologıa Oral, Universitat des Illes Balears, Illes Balears, Spain Summary We report condylar resorption of the temporomandibular joint after difficult intubation, leading to progressive midline mandibular deviation, subsequently treated by prosthetic joint replacement. ................................................................................................................................................................. Correspondence to: M. Fernandez-Barriales Email: [email protected] Accepted: 19 March 2013 Forces applied during difficult tracheal intubations can Following induction of anaesthesia and neuromus- cause oedema, bleeding, tracheal and oesophageal per- cular blockade, laryngoscopy with a Macintosh blade foration, pneumothorax or aspiration. Resorption of (size 3) permitted revealed a poor laryngeal view the temporomandibular joint has not been associated (Cormack-Lehane -

Chapter I GENERAL CORRECT CODING POLICIES for NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL for MEDICARE SERVICES
CHAP1-gencorrectcodingpolicies Revision Date: 1/1/2021 Chapter I GENERAL CORRECT CODING POLICIES FOR NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL FOR MEDICARE SERVICES Current Procedural Terminology (CPT) codes, descriptions and other data only are copyright 2020 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors, prospective payment systems, and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein. Revision Date (Medicare): 1/1/2021 Table of Contents LIST OF ACRONYMS ............................................ I-2 Chapter I ................................................... I-4 General Correct Coding Policies ............................ I-4 A. Introduction ..........................................I-4 B. Coding Based on Standards of Medical/Surgical Practice I-8 C. Medical/Surgical Package .............................I-11 D. Evaluation & Management (E&M) Services ...............I-16 E. Modifiers and Modifier Indicators ....................I-18 F. Standard Preparation/Monitoring Services for Anesthesia .................................................. I-26 G. Anesthesia Service Included in the Surgical Procedure I-26 H. HCPCS/CPT -
Application and Care of Two Kinds of Sphenoid Sinus Packing Materials After Pituitary Tumor Resection with the Transnasal Endoscopic Approach
Neuroscience & Medicine, 2020, 11, 130-141 https://www.scirp.org/journal/nm ISSN Online: 2158-2947 ISSN Print: 2158-2912 Application and Care of Two Kinds of Sphenoid Sinus Packing Materials after Pituitary Tumor Resection with the Transnasal Endoscopic Approach Shuo Yang, Qiyu Feng, Huidan Zhu, Zhihuan Zhou*, Ji Zhang* Department of Neurosurgery, State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Sun Yat-sen University Cancer Center, Guangzhou, China How to cite this paper: Yang, S., Feng, Abstract Q.Y., Zhu, H.D., Zhou, Z.H. and Zhang, J. (2020) Application and Care of Two Kinds Background: Neuroendoscopic transsphenoidal approach for resection of of Sphenoid Sinus Packing Materials after pituitary adenomas has the advantages of less damage, fewer complications, Pituitary Tumor Resection with the Trans- and a faster recovery than the traditional approach and has beening favored nasal Endoscopic Approach. Neuroscience by neurosurgeons. However, there has no standard method of selecting suita- & Medicine, 11, 130-141. https://doi.org/10.4236/nm.2020.114015 ble packing materials after the operation to relieve pain in patients and achieve the ideal hemostatic effect. We compared the postoperative complica- Received: October 4, 2020 tions and treatment effects of two different packing materials in patients with Accepted: December 12, 2020 pituitary adenomas. Objective: To investigate the advantages and disadvan- Published: December 15, 2020 tages of using a catheter balloon and iodoform gauze for hemostasis in pa- Copyright © 2020 by author(s) and tients undergoing pituitary tumor resection by neuroendoscopic transsphe- Scientific Research Publishing Inc. noidal approach. Materials and Methods: We retrospectively analyzed these This work is licensed under the Creative data of 48 cases treated with pituitary adenoma resection by the single nasal Commons Attribution International License (CC BY 4.0). -

Review Article the Management of Difficult Intubation in Children
Pediatric Anesthesia 2009 19 (Suppl. 1): 77–87 doi:10.1111/j.1460-9592.2009.03014.x Review article The Management of difficult intubation in children ROBERT W.M. WALKER FRCA* AND JAMES ELLWOOD FRCA† *Department of Paediatric Anaesthesia, Royal Manchester Children’s Hospital, Pendlebury, Manchester and †Department of Paediatric Anaesthesia, Royal Manchester Children’s Hospital, North West School of Anaesthesia, Pendlebury, Manchester Summary This article looks at the current techniques and equipment recom- mended for the management of the difficult intubation scenario in pediatric practice. We discuss the general considerations including preoperative preparation, the preferred anesthetic technique and the use of both rigid laryngoscopic and fiberoptic techniques for intuba- tion. The unanticipated scenario is also discussed. Keywords: paediatric; anaesthesia; difficult airway; difficult intubation; failed intubation; fibreoptic intubation; Laryngeal mask Introduction issues which need to be discussed in detail with the parents and the child if appropriate. This should be Generally, but not always, in pediatric practice, the performed well in advance at the preoperative visit. management of the difficult intubation scenario is a Firstly, the relative benefit of any planned surgery well predicted, well planned and hopefully well must be weighed against the possible risks of the executed procedure. However, undoubtedly, there anesthetic management. If there is any doubt sur- will be occasions when difficulty with either airway rounding either the timing of the surgery or indeed management (difficulty or inability to ventilate the the need for surgery, a full discussion should take patient or maintain an airway) and ⁄ or with endo- place with carers, child, surgeon and anesthetist to tracheal intubation is unexpected. -

Nasal Intubation: a Comprehensive Review
662 Review Article Nasal intubation: A comprehensive review Varun Chauhan, Gaurav Acharya Nasal intubation technique was first described in 1902 by Kuhn. The others pioneering the Access this article online nasal intubation techniques were Macewen, Rosenberg, Meltzer and Auer, and Elsberg. It Website: www.ijccm.org is the most common method used for giving anesthesia in oral surgeries as it provides a DOI: 10.4103/0972-5229.194013 good field for surgeons to operate. The anatomy behind nasal intubation is necessary to Quick Response Code: Abstract know as it gives an idea about the pathway of the endotracheal tube and complications encountered during nasotracheal intubation. Various techniques can be used to intubate the patient by nasal route and all of them have their own associated complications which are discussed in this article. Various complications may arise while doing nasotracheal intubation but a thorough knowledge of the anatomy and physics behind the procedure can help reduce such complications and manage appropriately. It is important for an anesthesiologist to be well versed with the basics of nasotracheal intubation and advances in the techniques. A thorough knowledge of the anatomy and the advent of newer devices have abolished the negative effect of blindness of the procedure. Keywords: Blind nasal intubation, complications, epistaxis, fiber optic, nasotracheal intubation Introduction (e.g., mandibular reconstructive procedures or mandibular osteotomies) and oropharyngeal surgeries. Nasal intubation technique was first -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

THE BONFILS INTUBATION ENDOSCOPE in Clinical and Emergency Medicine
® THE BONFILS INTUBATION ENDOSCOPE in Clinical and Emergency Medicine Tim PIEPHO Rüdiger NOPPENS ® THE BONFILS INTUBATION ENDOSCOPE in Clinical and Emergency Medicine Tim PIEPHO Rüdiger NOPPENS Department of Anesthesiology University Medical Center of the Johannes Gutenberg University Mainz, Germany With contributions from: Andreas THIERBACH Rita METZ Pedro BARGON 4 The BONFILS Intubation Endoscope in Clinical and Emergency Medicine Important notes: The BONFILS Intubation Endoscope Medical knowledge is ever changing. As new research in Clinical and Emergency Medicine and clinical experience broaden our knowledge, Tim Piepho and Rüdiger Noppens changes in treat ment and therapy may be required. Department of Anesthesiology, The authors and editors of the material herein have University Medical Center of the Johannes Gutenberg University Mainz, Germany consulted sources believed to be reliable in their efforts to provide information that is complete and in accord with the standards accept ed at the time of publication. However, in view of the possibili ty of human error by Correspondence address: the authors, editors, or publisher, or changes in medical Tim Piepho knowledge, neither the authors, editors, publisher, nor Klinik für Anästhesiologie any other party who has been involved in the preparation Universitätsmedizin der Johannes Gutenberg-Universität Mainz of this booklet, warrants that the information contained Langenbeckstr. 1 herein is in every respect accurate or complete, and they Telephone: +49 (0)6131/171 are not responsible for any errors or omissions or for the results obtained from use of such information. The E-mail: [email protected] information contained within this booklet is intended for use by doctors and other health care professionals.