Effective Treatment of Advanced Human Melanoma Metastasis In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hodgkin Lymphoma Treatment Regimens
HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 5) Clinical Trials: The National Comprehensive Cancer Network recommends cancer patient participation in clinical trials as the gold standard for treatment. Cancer therapy selection, dosing, administration, and the management of related adverse events can be a complex process that should be handled by an experienced health care team. Clinicians must choose and verify treatment options based on the individual patient; drug dose modifications and supportive care interventions should be administered accordingly. The cancer treatment regimens below may include both U.S. Food and Drug Administration-approved and unapproved indications/regimens. These regimens are provided only to supplement the latest treatment strategies. These Guidelines are a work in progress that may be refined as often as new significant data become available. The NCCN Guidelines® are a consensus statement of its authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult any NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way. Classical Hodgkin Lymphoma1 Note: All recommendations are Category 2A unless otherwise indicated. Primary Treatment Stage IA, IIA Favorable (No Bulky Disease, <3 Sites of Disease, ESR <50, and No E-lesions) REGIMEN DOSING Doxorubicin + Bleomycin + Days 1 and 15: Doxorubicin 25mg/m2 IV push + bleomycin 10units/m2 IV push + Vinblastine + Dacarbazine vinblastine 6mg/m2 IV over 5–10 minutes + dacarbazine 375mg/m2 IV over (ABVD) (Category 1)2-5 60 minutes. -

Desmoid Tumors: Understanding Treatment Options in 2019
Desmoid Tumors: Understanding Treatment Options in 2019 Breelyn A. Wilky, MD Associate Professor Sarcoma Program, Division of Oncology A real desmoid story… 35 year old female physician who noted abdominal cramping and pain in her mid abdomen and a palpable mass in August 2018 She performed an ultrasound on herself in the ER which showed a 4.5 x 4.5 cm mass in her mid abdomen CT scan showed a mesenteric mass that was wrapped around and blocking the inferior mesenteric vein with multiple satellite nodules/lymph nodes. Biopsy confirmed the diagnosis of desmoid tumor A real desmoid story… Mother had a neuroendocrine cancer in the appendix, father had Hodgkins lymphoma The patient had a negative colonoscopy for any polyps She had no other medical problems but has three children, with the last baby born 4 months prior to her symptoms. This most recent baby was conceived with in vitro fertilization. Tumor board discussion… Ongoing pain likely related to venous outflow obstruction (confirmed on colonoscopy as well) Treatment options in 2019… Watch and Wait • Doxorubicin/ Dacarbazine Chemotherapy Attempt • MTX/vinblastine (IV) Surgery • Doxil • Sorafenib • Imatinib Targeted • Pazopanib treatments Radiation • Nirogacestat (chemo pills) • Tegavivint (IV) • Tamoxifen +/- sulindac Estrogen- Ablation • Aromatase blocking IRE/Nanoknife inhibitors Treatments HIFU • Celebrex Choosing a treatment approach . Anxiety over “doing nothing” . How long is acceptable to wait for Symptoms a response? Location . Can shrinkage or necrosis create a Risk to surrounding structures more definitive option? (surgery, and organs electroporation?) Growth pattern over time . What is the expected function or appearance after my desmoid Obvious estrogen exposure surgery? (pregnancy) . -

Systemic Therapy for Advanced Soft Tissue Sarcoma
Systemic Therapy for Advanced Soft Tissue Sarcoma a, b Jennifer Y. Sheng, MD *, Sujana Movva, MD KEYWORDS Advanced soft tissue sarcoma Chemotherapy Novel therapies KEY POINTS Survival for advanced soft tissue sarcomas has improved significantly over the last 20 years because of advancements in histologic classification, improved treatment ap- proaches, and novel agents. An important factor guiding choice of therapy is soft tissue sarcoma subtype, as drugs such as eribulin and trabectedin may have particular activity in leiomyosarcoma and liposarcoma. Focus on angiogenesis inhibition has led to the approval of pazopanib for soft tissue sar- coma, and the pathway continues to be investigated in this disease. Toxicity is an important area of investigation in soft tissue sarcoma, and new agents, such as aldoxorubicin, may be alternatives with better safety profiles. Future studies on treatment of advanced soft tissue sarcoma will continue to focus on identification of novel drug targets, personalization of therapy, and combination immunotherapies. BACKGROUND Sarcomas are rare tumors that arise from or are differentiated from tissues of meso- dermal origin. They comprise less than 1% of all adult malignancies.1 In 2015 there were approximately 14, 900 new cases diagnosed, with 6360 deaths in the United States. Sarcomas are grouped into 2 general categories: soft tissues sarcomas and primary bone sarcomas, which have different staging and treatment approaches. This article includes a discussion of chemotherapy in advanced or refractory soft tis- sue sarcoma. Patients with metastatic disease are usually best managed with chemo- therapy. Distant metastasis occurs in up to 10% of patients, with the lung being the most common site in 83% of cases.2 Systemic therapy can involve cytotoxic a Department of Oncology, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins Uni- versity School of Medicine, Baltimore, MD, USA; b Department of Hematology/Oncology, Fox Chase Cancer Center, 333 Cottman Avenue, Philadelphia, PA 19111, USA * Corresponding author. -
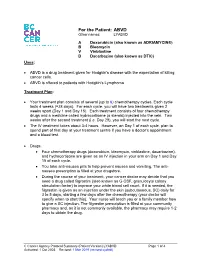
ABVD Other Names: LYABVD
For the Patient: ABVD Other names: LYABVD A Doxorubicin (also known as ADRIAMYCIN®) B Bleomycin V Vinblastine D Dacarbazine (also known as DTIC) Uses: • ABVD is a drug treatment given for Hodgkin's disease with the expectation of killing cancer cells. • ABVD is offered to patients with Hodgkin’s Lymphoma Treatment Plan: • Your treatment plan consists of several (up to 6) chemotherapy cycles. Each cycle lasts 4 weeks (=28 days). For each cycle, you will have two treatments given 2 weeks apart (Day 1 and Day 15). Each treatment consists of four chemotherapy drugs and a medicine called hydrocortisone (a steroid) injected into the vein. Two weeks after the second treatment (i.e. Day 29), you will start the next cycle. • The IV treatment takes about 3-4 hours. However, on Day 1 of each cycle, plan to spend part of that day at your treatment centre if you have a doctor’s appointment and a blood test. • Drugs: • Four chemotherapy drugs (doxorubicin, bleomycin, vinblastine, dacarbazine), and hydrocortisone are given as an IV injection in your arm on Day 1 and Day 15 of each cycle. • You take anti-nausea pills to help prevent nausea and vomiting. The anti- nausea prescription is filled at your drugstore. • During the course of your treatment, your cancer doctor may decide that you need a drug called filgrastim (also known as G-CSF, granulocyte colony stimulation factor) to improve your white blood cell count. If it is needed, the filgrastim is given as an injection under the skin (subcutaneous, SC) daily for 3 to 5 days, starting a few days after the chemotherapy (your doctor will specify when to start this). -

CVD: Cisplatin, Vinblastine, and Dacarbazine
PATIENT EDUCATION patienteducation.osumc.edu CVD: Cisplatin, Vinblastine, and Dacarbazine What is CVD? It is the short name for the drugs used in this chemotherapy treatment. The three drugs you will receive during this treatment are Cisplatin (“C”), Vinblastine (“V”), and Dacarbazine (DTIC-DomeTM or “D”). This chemotherapy will be given daily for 5 days. What is Cisplatin (SIS-pla-tin) and how does it work? Cisplatin is a chemotherapy drug known as an “alkylating agent.” Cisplatin works to stop fast growing cancer cells from dividing and making new cells. This will be given daily on days 2 through 5. What is Vinblastine (vin-BLAS-teen) and how does it work? Vinblastine is a chemotherapy drug known as an “anti-microtubule inhibitor.” This drug fights cancer cells by stopping fast growing cancer cells from dividing and making new cancer cells. This drug will be given daily on days 1 through 5. What is Dacarbazine (da-KAR-ba-zeen) and how does it work? Dacarbazine is a chemotherapy drug known as an “alkylating agent.” Dacarbazine works to stop fast growing cancer cells from dividing and making new cells. This drug will be given on the first day. This handout is for informational purposes only. Talk with your doctor or health care team if you have any questions about your care. © September 10, 2020. The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute. Why am I getting three chemotherapy drugs for my cancer? These drugs work to stop fast growing cancer cells from dividing and making new cells, but they attack the cancer cells differently. -

Gemcitabine-Containing Chemotherapy for the Treatment of Metastatic Myxofibrosarcoma Refractory to Doxorubicin: a Case Series
Brief Report Gemcitabine-Containing Chemotherapy for the Treatment of Metastatic Myxofibrosarcoma Refractory to Doxorubicin: A Case Series 1, 2, 1,2, Arielle Elkrief y, Suzanne Kazandjian y and Thierry Alcindor * 1 Cedars Cancer Center, McGill University Health Centre, Montreal, QC H4A 3J1, Canada; [email protected] 2 Department of Medicine, McGill University Health Centre, Montreal, QC H4A 3J1, Canada; [email protected] * Correspondence: [email protected] These authors contributed equally to this paper. y Received: 7 December 2020; Accepted: 3 February 2021; Published: 5 February 2021 Abstract: Background: Myxofibrosarcoma is a type of soft-tissue sarcoma that is associated with high rates of local recurrence and distant metastases. The first-line treatment for metastatic soft-tissue sarcoma has conventionally been doxorubicin-based. Recent evidence suggests that myxofibrosarcoma may be molecularly similar to undifferentiated pleomorphic sarcoma (UPS), which is particularly sensitive to gemcitabine-based therapy. The goal of this study was to evaluate the activity of gemcitabine-containing regimens for the treatment of metastatic myxofibrosarcoma refractory to doxorubicin. Material and Methods: We retrospectively evaluated seven consecutive cases of metastatic myxofibrosarcoma at our institution treated with gemcitabine-based therapy in the second-line setting, after progression on doxorubicin. Baseline clinical and baseline characteristics were collected. Primary endpoints were objective response rate (ORR), progression-free survival (PFS) and overall survival (OS). Results: After progression on first-line doxorubicin, a partial, or complete radiological response was observed in four of seven patients who received gemcitabine-based chemotherapy. With a median follow-up of 14 months, median progression-free and overall survival were 8.5 months and 11.4 months, respectively. -

Efficacy, Safety, and Tolerability of Approved Combination BRAF and MEK Inhibitor Regimens for BRAF-Mutant Melanoma
Cancers 2019, 11, 1642; doi:10.3390/cancers11111642 S1 of S5 Supplementary Materials: Efficacy, Safety, and Tolerability of Approved Combination BRAF and MEK Inhibitor Regimens for BRAF-Mutant Melanoma Omid Hamid, C. Lance Cowey, Michelle Offner, Mark Faries and Richard D. Carvajal Table S1. Anticancer Treatment by Regimen Following Study Drug Discontinuation. Dabrafenib + Trametinib Vemurafenib + Encorafenib + [1,2] Cobimetinib [3] Binimetinib [4] COMBI-v † COMBI-d coBRIM COLUMBUS n = 352 n = 209 n = 183 n = 192 Any treatment 72 (20%) 101 (48%) 105 (57%) 80 (42%) Immunotherapy NR 117 (56%) 67 (37%) NR Any anti–PD-1/anti–PD-L1 NR NR 28 (15%) 39 (20%) Ipilimumab (anti-CTLA-4) 41 (12%) 86 (41%) 53 (29%) 33 (17%) Nivolumab (anti-PD-1) NR 15 (7%) NR NR Pembrolizumab (anti–PD-L1) 4 (1%) 27 (13%) NR NR anti-CTLA-4 + NR NR 4 (2%) 6 (3%) anti–PD-1/anti–PD-L1 ‡ Targeted therapies NR 21 (10%) § 32 (18%) NR BRAFi + MEKi NR NR 15 (8%) 10 (5%) ¶ BRAFi NR NR 19 (10%) 11 (6%) # MEKi NR NR 2 (1%) NR Chemotherapy NR 37 (18%) 30 (16%) 14 (7%) ** Other NR NR 2 (1%) †† 5 (3%) ‡‡ NR = not reported. Data are n (%). PD-1 = programmed death cell receptor 1. PD-L1 = programmed death cell ligand 1. † Multiple uses of a type of therapy for an individual patient were only counted once in the frequency for that treatment category; patients mght have received multiple lines of treatment. Received by ≥2% of patients. ‡ Ipilimumab + nivolumab or ipilimumab + pembrolizumab. § Small-molecule targeted therapy. -

Dacarbazine Medac 100 Mg (-200 Mg, -500 Mg, -1000 Mg) Summary of Product Characteristics 1. Name of the Medicinal Product Dacar
medac GmbH 1.3.1.1.1 Document page: 1 Dacarbazine medac 100 mg (-200 mg, -500 mg, -1000 mg) Summary of Product Characteristics 1. Name of the Medicinal Product Dacarbazine medac 100 mg, Powder for solution for injection or infusion Dacarbazine medac 200 mg, Powder for solution for injection or infusion Dacarbazine medac 500 mg, Powder for solution for infusion Dacarbazine medac 1000 mg, Powder for solution for infusion 2. Qualitative and Quantitative Composition Each single-dose vial of Dacarbazine medac 100 mg (-200 mg, -500 mg, -1000 mg) contains 100 mg (200 mg, 500 mg, 1000 mg) dacarbazine (as dacarbazine citrate, formed in situ). After reconstitution Dacarbazine medac 100 mg (-200 mg) contains 10 mg/ml dacarbazine (see 6.6. a). After reconstitution and final dilution Dacarbazine medac 500 mg (-1000 mg) contains 1.4 – 2.0 mg/ml (2.8 – 4.0 mg/ml) dacarbazine (see 6.6. b). For excipients, see section 6.1. 3. Pharmaceutical Form Dacarbazine medac 100 mg (-200 mg): Powder for solution for injection or infusion. Dacarbazine medac 500 mg (-1000 mg): Powder for solution for infusion. Dacarbazine medac is a white or pale yellow powder. CLINICAL PARTICULARS 4.1 Therapeutic Indications Dacarbazine is indicated for the treatment of patients with metastasized malignant melanoma. Further indications for dacarbazine as part of a combination chemotherapy are: - advanced Hodgkin’s disease, - advanced adult soft tissue sarcomas (except mesothelioma, Kaposi sarcoma). 4.2 Posology and Method of Administration The use of dacarbazine should be confined to physicians experienced in oncology or hematology respectively. Dacarbazine is sensitive to light exposure. -

Cancer Drug Costs for a Month of Treatment at Initial Food
Cancer drug costs for a month of treatment at initial Food and Drug Administration approval Year of FDA Monthly Cost Monthly cost (2013 Generic name Brand name(s) approval (actual $'s) $'s) Vinblastine Velban 1965 $78 $575 Thioguanine, 6-TG Thioguanine Tabloid 1966 $17 $122 Hydroxyurea Hydrea 1967 $14 $97 Cytarabine Cytosar-U, Tarabine PFS 1969 $13 $82 Procarbazine Matulane 1969 $2 $13 Testolactone Teslac 1969 $179 $1,136 Mitotane Lysodren 1970 $134 $801 Plicamycin Mithracin 1970 $50 $299 Mitomycin C Mutamycin 1974 $5 $22 Dacarbazine DTIC-Dome 1975 $29 $125 Lomustine CeeNU 1976 $10 $41 Carmustine BiCNU, BCNU 1977 $33 $127 Tamoxifen citrate Nolvadex 1977 $44 $167 Cisplatin Platinol 1978 $125 $445 Estramustine Emcyt 1981 $420 $1,074 Streptozocin Zanosar 1982 $61 $147 Etoposide, VP-16 Vepesid 1983 $181 $422 Interferon alfa 2a Roferon A 1986 $742 $1,573 Daunorubicin, Daunomycin Cerubidine 1987 $533 $1,090 Doxorubicin Adriamycin 1987 $521 $1,066 Mitoxantrone Novantrone 1987 $477 $976 Ifosfamide IFEX 1988 $1,667 $3,274 Flutamide Eulexin 1989 $213 $399 Altretamine Hexalen 1990 $341 $606 Idarubicin Idamycin 1990 $227 $404 Levamisole Ergamisol 1990 $105 $187 Carboplatin Paraplatin 1991 $860 $1,467 Fludarabine phosphate Fludara 1991 $662 $1,129 Pamidronate Aredia 1991 $507 $865 Pentostatin Nipent 1991 $1,767 $3,015 Aldesleukin Proleukin 1992 $13,503 $22,364 Melphalan Alkeran 1992 $35 $58 Cladribine Leustatin, 2-CdA 1993 $764 $1,229 Asparaginase Elspar 1994 $694 $1,088 Paclitaxel Taxol 1994 $2,614 $4,099 Pegaspargase Oncaspar 1994 $3,006 $4,713 -

Injectable and Health Care Administered Oncology Medical Drug Criteria Through Preferred (Optional)
Injectable and Health Care Administered Oncology Medical Drug Program Summary For patients with late stage metastatic disease (Stage IV), please refer to MP 2.373 Step Therapy Treatment in Cancer, Including Treatments for Stage Four, Advanced Metastatic Cancer and Severe Related Health Conditions for additional guidance *No Preferred Strategy The clinical rationale section is inf ormational, please refer to the medical drug criteria section for agents requiring medical drug review. FDA APPROVED INDICATIONS AND DOSAGE1-65 Agent Indication Dosage Abraxane® [paclitaxel ● Metastatic breast cancer Metastatic breast cancer: (protein bound)] af ter failure of combination 260 mg/m2 intravenously chemotherapy or relapse over 30 minutes, every 3 Injectable suspension within 6 months of adjuvant weeks chemotherapy. Prior therapy should have included an anthracycline unless clinically contraindicated ● Locally advanced or NSCLC: metastatic Non-Small Cell 100 mg/m2 intravenously Lung Cancer (NSCLC) as over 30 minutes on Days 1, f irst-line treatment in 8, and 15 of each 21-day combination with cycle. Administer carboplatin, in patients who carboplatin on Day 1 of each are not candidates for 21-day cycle immediately curative surgery or radiation af ter Abraxane therapy ● Metastatic adenocarcinoma Metastatic of the pancreas as first-line adenocarcinoma of the treatment in combination pancreas: with gemcitabine 125 mg/m2 intravenously over 30-40 minutes on Days 1, 8, and 15 of each 28-day cycle. Administer gemcitabine immediately af ter paclitaxel (protein bound) on days 1, 8, and 15 of each 28-day cycle Adcetris® (brentuximab Treatment of adult patients vedotin) with: Injection for intravenous ● Previously untreated Stage Previously untreated use III or IV classical Hodgkin Stage III or IV cHL: 1.2 lymphoma (cHL) in mg/kg up to a maximum of combination with 120 mg every 2 weeks for a doxorubicin, vinblastine, and maximum of 12 doses dacarbazine CBC_CS_Reg_MDC_Injectable_and_Health_Care_Administered_Oncology_P rogSum_AR0620_r0321 Page 1 of 46 © Copyright Prime Therapeutics LLC. -

Acronyms for Oncology Regimens
ACRONYMS AND ABBREVIATIONS OF COMMONLY USED REGIMENS ACRONYM CHEMOTHERAPY COMBINATION 7 + 3 Anthracycline (daunorubicin/idarubicin) or anthracenedione (mitoxantrone)/cytarabine ABV Doxorubicin/ bleomycin/vincristine ABVD Doxorubicin/ bleomycin/vinblastine/dacarbazine AC Doxorubicin/cyclophosphamide ACE Doxorubicin/cyclophosphamide/etoposide AI Doxorubicin/ifosfamide AIDA Tretinoin/idarubicin/dexamethasone/mitoxantrone/6-mercaptopurine/ methotrexate AP Doxorubicin/cisplatin AT Doxorubicin/docetaxel BEACOPP Bleomycin/etoposide/doxorubicin/cyclophosphamide/vincristine/procarbazine/ prednisone BEP Bleomycin/etoposide/cisplatin BMC Bleomycin/methotrexate/carmustine CAD Cyclophosphamide/doxorubicin/dacarbazine CAP Cyclophosphamide/doxorubicin/cisplatin CAPIRI Capecitabine/irinotecan CAPOX Capecitabine/oxaliplatin CAV Cyclophosphamide/doxorubicin/vincristine CDE Cyclophosphamide/doxorubicin/etoposide CDE-R Cyclophsopahmide/doxorubicin/etoposide/rituximab CECA Cyclophosphamide/etoposide/carboplatin/cytarabine CFAR Alemtuzumab/fludarabine/cyclophosphamide/rituximab CHOEP Cyclophosphamide/doxorubicin/vincristine/etoposide/prednisone CHOP Cyclophosphamide/doxorubicin/vincristine/prednisone CHOP-R Cyclophosphamide/doxorubicin/vincristine/prednisone/rtuximab ChlVPP Chlorambucil/vinblastine/procarbazine/prednisone CMF Cyclophosphamide/methotrexate/5-Fluorouracil CNOP Cyclophosphamide/mitoxantrone/vincristine/prednisone CODOX-M Cyclophsopahmide/vincristine/doxorubicin/cyclophosphamide/methotrexate/ leucovorin/intrathecal cytarabine/intrathecal methotrexate -

Treatment of Advanced Prostate Cancer John H
Clinical Review Treatment of Advanced Prostate Cancer John H. Lynch, MD Washington, DC Many patients with prostate cancer present with ad chiectomy has been the traditional approach, but most vanced disease (stage C or D). For these patients, patients prefer equally effective drug therapies that in treatment is palliative and is aimed at reducing serum clude the administration of estrogens, luteinizing hor testosterone levels. Since the growth of prostate cancer mone-releasing hormone (LHRH) agonists, and anti is testosterone-dependent (approximately 95% of tes androgens. tosterone is produced by the testes, with the remainder Key words. Prostate; treatment outcome; disease man coming from the adrenals), hormonal manipulation has agement; drug therapy; orchiectomy. (/ Fam Pm been the mainstay of palliative treatment. Bilateral or 1993; 37:488-494) Prostate cancer is the most common malignancy in the improve the results seen with LHRH analogs; also, flare male population of the United States. Unfortunately, reactions diminish with concurrent treatment. prostate cancer is not diagnosed in many patients until Current research indicates that many patients with the tumor has progressed to an advanced stage with prostate cancer want to take a more active role in deci involvement beyond the prostate (stage C or D). The sion-making with regard to their treatment.4 Thus, pri etiology of prostate cancer is not well understood, but mary care physicians may become more involved in coun there is a clear association between serum testosterone seling these patients on treatment options. levels and prostate tissue growth. This paper discusses the treatment options for pa The treatment of advanced prostate cancer is primar tients with advanced stage prostate cancer, and highlights ily palliative, as cures are rare.