Trogarzo™ (Ibalizumab‐Uiyk)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pros and Cons of Entry and Fusion Inhibitors (Review)
MOLECULAR MEDICINE REPORTS 19: 1987-1995, 2019 Investigational drugs in HIV: Pros and cons of entry and fusion inhibitors (Review) EMMANUELE VENANZI RULLO1,2, MANUELA CECCARELLI1, FABRIZIO CONDORELLI3, ALESSIO FACCIOLÀ1, GIUSEPPA VISALLI4, FRANCESCO D'ALEO1, IVANA PAOLUCCI1, BRUNO CACOPARDO5, MARILIA RITA PINZONE2-5, MICHELE DI ROSA6, GIUSEPPE NUNNARI1 and GIOVANNI F. PELLICANÒ7 1Department of Clinical and Experimental Medicine, Unit of Infectious Diseases, University of Messina, I-90124 Messina, Italy; 2Department of Pathology and Laboratory Medicine, School of Medicine, University of Pennsylvania, Philadelphia, PA 19104, USA; 3Department of Pharmacological Sciences, University of Eastern Piedmont ‘A. Avogadro’, I-13100 Novara; 4Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, I-90124 Messina; 5Department of Clinical and Experimental Medicine, University of Catania, I-95123 Catania; 6Department of Biomedical and Biotechnological Sciences, Human Anatomy and Histology Section, University of Catania, I-95123 Catania; 7Department of Human Pathology of the Adult and the Developmental Age ‘G. Barresi’, Unit of Infectious Diseases, University of Messina, I-98122 Messina, Italy Received September 2, 2018; Accepted November 29, 2018 DOI: 10.3892/mmr.2019.9840 Abstract. Despite the profound changes and improve- 4. Gp41 antagonists ments reached in the field of HIV treatment, tolerability and 5. CD4 antagonists adherence to highly active antiretroviral therapy remains a 6. Discussion challenge. Furthermore, multi-experienced patients could take advantage of drugs with different mechanisms of action to combat the spread of resistance to actual therapy. For these 1. Introduction reasons identification of new HIV drugs is crucial. Among all the molecules that at present are under investigation, entry HIV continues to be an important challenge and a major and fusion inhibitors pose an interesting class owing to their global public health issue. -

Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients
antibodies Review Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients Andrew T. Lucas 1,2,3,*, Ryan Robinson 3, Allison N. Schorzman 2, Joseph A. Piscitelli 1, Juan F. Razo 1 and William C. Zamboni 1,2,3 1 University of North Carolina (UNC), Eshelman School of Pharmacy, Chapel Hill, NC 27599, USA; [email protected] (J.A.P.); [email protected] (J.F.R.); [email protected] (W.C.Z.) 2 Division of Pharmacotherapy and Experimental Therapeutics, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 3 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-919-966-5242; Fax: +1-919-966-5863 Received: 30 November 2018; Accepted: 22 December 2018; Published: 1 January 2019 Abstract: The rapid advancement in the development of therapeutic proteins, including monoclonal antibodies (mAbs) and antibody-drug conjugates (ADCs), has created a novel mechanism to selectively deliver highly potent cytotoxic agents in the treatment of cancer. These agents provide numerous benefits compared to traditional small molecule drugs, though their clinical use still requires optimization. The pharmacology of mAbs/ADCs is complex and because ADCs are comprised of multiple components, individual agent characteristics and patient variables can affect their disposition. To further improve the clinical use and rational development of these agents, it is imperative to comprehend the complex mechanisms employed by antibody-based agents in traversing numerous biological barriers and how agent/patient factors affect tumor delivery, toxicities, efficacy, and ultimately, biodistribution. -

Keeping up with FDA Drug Approvals: 60 New Drugs in 60 Minutes Elizabeth A
Keeping Up with FDA Drug Approvals: 60 New Drugs in 60 Minutes Elizabeth A. Shlom, PharmD, BCPS Senior Vice President & Director Clinical Pharmacy Program | Acurity, Inc. Privileged and Confidential April 10, 2019 Privileged and Confidential Program Objectives By the end of the presentation, the pharmacist or pharmacy technician participant will be able to: ▪ Identify orphan drugs and first-in-class medications approved by the FDA in 2018. ▪ List five new drugs and their indications. ▪ Identify the place in therapy for three novel monoclonal antibodies. ▪ Discuss at least two new medications that address public health concerns. Dr. Shlom does not have any conflicts of interest in regard to this presentation. Both trade names and generic names will be discussed throughout the presentation Privileged and Confidential 2018 NDA Approvals (NMEs/BLAs) ▪ Lutathera (lutetium Lu 177 dotatate) ▪ Braftovi (encorafenib) ▪ Vizimpro (dacomitinib) ▪ Biktarvy (bictegravir, emtricitabine, ▪ TPOXX (tecovirimat) ▪ Libtayo (cemiplimab-rwic) tenofovir, ▪ Tibsovo (ivosidenib) ▪ Seysara (sarecycline) alafenamide) ▪ Krintafel (tafenoquine) ▪ Nuzyra (omadacycline) ▪ Symdeko (tezacaftor, ivacaftor) ▪ Orilissa (elagolix sodium) ▪ Revcovi (elapegademase-lvir) ▪ Erleada (apalutamide) ▪ Omegaven (fish oil triglycerides) ▪ Tegsedi (inotersen) ▪ Trogarzo (ibalizumab-uiyk) ▪ Mulpleta (lusutrombopag) ▪ Talzenna (talazoparib) ▪ Ilumya (tildrakizumab-asmn) ▪ Poteligeo (mogamulizumab-kpkc) ▪ Xofluza (baloxavir marboxil) ▪ Tavalisse (fostamatinib disodium) ▪ Onpattro (patisiran) -

An HIV Clinician's View
HIV Meets Oncology: An HIV Clinician’s View Merceditas S. Villanueva MD Director, HIV/AIDS Program Yale University School of Medicine HIV and Cancer Retreat April 30, 2019 Financial Disclosures • None Case Presentation • 58 year old man diagnosed with HIV in 1996 • Early years: serial ART mono and dual therapy with multidrug resistance • Moved to CT 2005-worked in pharmaceutical field (ART development) • I met him in 2009-applying for disability ART Over Time Saquinavir Tenofovir Emtricitabine Stavudine Ritonavir Atazanavir Maraviroc Elvitegravir Zidovudine Doravirine Indinavir Enfuvirtide Raltegravir Nelfinavir Ibalizumab 1985 1990 1995 2000 2005 2010 2015 2018 Didanosine Tenofovir Lamivudine Efavirenz Darunavir Rilpivirine alafenamide Abacavir Fosemprenavir Dolutegravir Nevirapine Lopinavir+Ritonavir Etravirine ART in Single Tablet Regimen Now 1 pill a Day 2-3 ARVs co-formulated ART Simpler and Safer AN AIDS TIMELINE: The 1st Decade RONALD REAGAN GEORGE H.W. BUSH 1981-1989 1989-1993 ’85 ’87 AZT ’82 First approved HIV “AIDS” ’83 Virus test isolation 1981 AN AIDS TIMELINE: The 2nd Decade GEORGE H.W. BUSH WILLIAM CLINTON 1989-1993 1993-2000 92’ ddl/ddC 93’ d4t Dual NRTI’s HAART ’97: NEL, DLV, Combivir ’95: Saquinavir ’96: NVP, IDV, RIT ’92 AIDS ’96 HIV leading cause viral load of death approved adults 25-44 yrs old AIDS Deaths Red down Ribbon 40% due Tony to Awards HAART 19901 1994 1995 ‘96 My Pt was diagnosed HIV+ AN AIDS TIMELINE: THE 3rd Decade … GEORGE W. BUSH BARACK H. OBAMA 2001-2008 2009 - 2016 ’00 ’01 ’03 ‘04 ’05 ‘06 Darunavir ’07 ’08 Trizivir Tenofo Fuzeon Truvada Tipranavir Maraviroc Etravirine -Atripla vir Raltegravir Lopinavir ’00 13th Int’l AIDS : Conf in PEPFAR 25 30 Durban SA $15B/5 yrs years years 2000 AN AIDS TIMELINE: THE 4th Decade … DONALD J. -

TROGARZO (Ibalizumab-Uiyk) RATIONALE for INCLUSION IN
TROGARZO (ibalizumab-uiyk) RATIONALE FOR INCLUSION IN PA PROGRAM Background Trogarzo (ibalizumab-uiyk) is a recombinant humanized monoclonal antibody that blocks HIV-1 from infecting CD4+ T-cells. This medication blocks the HIV-1 virus from entering the host cell by interfering with post-attachment steps required for the entry of HIV-1 virus that occurs via cell fusion. The binding specificity of ibalizumab-uiyk to domain 2 of CD4 allows ibalizumab-uiyk to block viral entry into host cells without causing immunosuppression (1). Regulatory Status FDA approved indication: Trogarzo, a CD4-directed post-attachment HIV-1 inhibitor, in combination with other antiretroviral(s), is indicated for the treatment of human immunodeficiency virus type 1 (HIV-1) infection in heavily treatment-experienced adults with multidrug resistant HIV-1 infection failing their current antiretroviral regimen (1). Immune reconstitution inflammatory syndrome has been reported in one patient treated with Trogarzo in combination with other antiretrovirals. During the initial phase of combination antiretroviral therapies, patients whose immune systems respond may develop an inflammatory response to indolent or residual opportunistic infections, which may necessitate further evaluation and treatment(1). Phenotypic and genotypic test results revealed no evidence of cross-resistance between ibalizumab-uiyk and any of the approved classes of anti-retroviral drugs (CCR5 co-receptor antagonists, gp41 fusion inhibitors, integrase strand transfer inhibitors [INSTIs], non-nucleos(t)ide reverse transcriptase inhibitors [NNRTIs], nucleos(t)ide reverse transcriptase inhibitors [NRTIs], or protease inhibitors [PIs]). Ibalizumab-uiyk is active against HIV-1 resistant to all approved antiretroviral agents and exhibits antiretroviral activity against R5-tropic, X4-tropic, and dual-tropic HIV-1 (1). -

CDER Breakthrough Therapy Designation Approvals Data As of December 31, 2020 Total of 190 Approvals
CDER Breakthrough Therapy Designation Approvals Data as of December 31, 2020 Total of 190 Approvals Submission Application Type and Proprietary Approval Use Number Number Name Established Name Applicant Date Treatment of patients with previously BLA 125486 ORIGINAL-1 GAZYVA OBINUTUZUMAB GENENTECH INC 01-Nov-2013 untreated chronic lymphocytic leukemia in combination with chlorambucil Treatment of patients with mantle cell NDA 205552 ORIGINAL-1 IMBRUVICA IBRUTINIB PHARMACYCLICS LLC 13-Nov-2013 lymphoma (MCL) Treatment of chronic hepatitis C NDA 204671 ORIGINAL-1 SOVALDI SOFOSBUVIR GILEAD SCIENCES INC 06-Dec-2013 infection Treatment of cystic fibrosis patients age VERTEX PHARMACEUTICALS NDA 203188 SUPPLEMENT-4 KALYDECO IVACAFTOR 21-Feb-2014 6 years and older who have mutations INC in the CFTR gene Treatment of previously untreated NOVARTIS patients with chronic lymphocytic BLA 125326 SUPPLEMENT-60 ARZERRA OFATUMUMAB PHARMACEUTICALS 17-Apr-2014 leukemia (CLL) for whom fludarabine- CORPORATION based therapy is considered inappropriate Treatment of patients with anaplastic NOVARTIS lymphoma kinase (ALK)-positive NDA 205755 ORIGINAL-1 ZYKADIA CERITINIB 29-Apr-2014 PHARMACEUTICALS CORP metastatic non-small cell lung cancer (NSCLC) who have progressed on or are intolerant to crizotinib Treatment of relapsed chronic lymphocytic leukemia (CLL), in combination with rituximab, in patients NDA 206545 ORIGINAL-1 ZYDELIG IDELALISIB GILEAD SCIENCES INC 23-Jul-2014 for whom rituximab alone would be considered appropriate therapy due to other co-morbidities -

Evaluating the Pressor Effects of Drugs & Ambulatory Blood
Characterizing FDA’s Approach to Benefit-Risk Assessment throughout the Medical Product Life Cycle Tommy Douglas Conference Center • Silver Spring, MD May 16th, 2019 9:00 am – 4:55 pm Contents 2 Welcome & Overview Dr. Mark McClellan, MD, PhD, Director, Duke-Margolis Center for Health Policy 9:00 am – 9:05 am Electronic Comments Federal eRulemaking Portal Docket ID: FDA-2019-N-1468 Due June 17, 2019 11:59 PM ET www.regulations.gov/docket?D=FDA-2019-N-1468 Opening Remarks Theresa Mullin, PhD, Associate Director for Strategic Initiatives Center for Drug Evaluation and Research (CDER) 9:05 am – 9:15 am Applying Framework for Benefit-Risk Assessment Throughout the Human Drug Life Cycle Opening Remarks Theresa Mullin, PhD Associate Director Strategic Initiatives FDA Center for Drug Evaluation and Research May 16, 2019 Context • FDA qualitative structured B-R framework – primarily discussed in context of premarket assessment • PDUFA VI (FDARA 2017) enhancing benefit-risk assessment in regulatory decision-making • FDA will further the agency’s implementation of structured benefit-risk assessment, including the incorporation of the patient’s voice in drug development and decision- making, in the human drug review program • FY 2019 --FDA will convene a meeting, conducted through a qualified third party, to gather industry, patient, researcher, and other stakeholder input on key topics. • Including applying the benefit-risk framework throughout the human drug lifecycle, including best approaches to communicating FDA’s benefit-risk assessment • FY -

Medical Drug Benefit Clinical Criteria Updates
Medical drug benefit Clinical Criteria updates On November 15, 2019, the Pharmacy and Therapeutics (P&T) Committee approved the following Clinical Criteria applicable to the medical drug benefit for Amerigroup Iowa, Inc. These policies were developed, revised or reviewed to support clinical coding edits. Visit Clinical Criteria to search for specific policies. For questions or additional information, use this email. Please see the explanation/definition for each category of Clinical Criteria below: New: newly published criteria Revised: addition or removal of medical necessity requirements, new document number Annual Review: minor wording and formatting updates, new document number Updates marked with an asterisk (*): criteria may be perceived as more restrictive Please share this notice with other members of your practice and office staff. Please note: The Clinical Criteria listed below applies only to the medical drug benefits contained within the member’s medical plan. This does not apply to pharmacy services. Effective date Document Clinical Criteria title New, revised, number annual review 03/30/2020 ING-CC-0148 Agents for Hemophilia B New 03/30/2020 ING-CC-0149* Select Clotting Agents for New Bleeding Disorders 03/30/2020 ING-CC-0150* Kymriah (tisagenlecleucel) Revised 03/30/2020 ING-CC-0151 Yescarta (axicabtagene ciloleucel) Revised 03/30/2020 ING-CC-0059 Selected Injectable NK-1 Revised Antiemetic Agents 03/30/2020 ING-CC-0056 Selected Injectable 5HT3 Revised Antiemetic Agents 03/30/2020 ING-CC-0074 Akynzeo (fosnetupitant -
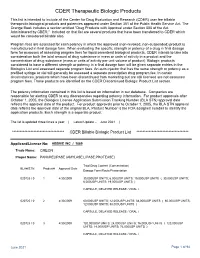
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Provider Administered Drugs – Site of Care – Oxford Clinical Policy
UnitedHealthcare® Oxford Clinical Policy Provider Administered Drugs – Site of Care Policy Number: PHARMACY 276.34 T2 Effective Date: October 1, 2021 Instructions for Use Table of Contents Page Related Policies ® Coverage Rationale ........................................ 2 • Actemra (Tocilizumab) Injection for Intravenous Infusion Documentation Requirements ....................... 3 ® • Adakveo (Crizanlizumab-Tmca) Definitions ....................................................... 3 • Alpha1-Proteinase Inhibitors Prior Authorization Requirements ................. 3 ™ • Amondys 45 (Casimersen) Applicable Codes ........................................... 4 ® • Benlysta (Belimumab) Clinical Evidence ............................................ 5 ® • Cimzia (Certolizumab Pegol) References ...................................................... 6 ® ® • Complement Inhibitors (Soliris & Ultomiris ) Policy History/Revision Information .............. 8 ® Instructions for Use ........................................ 8 • Crysvita (Burosumab) • Denosumab (Prolia® & Xgeva®) • Drug Coverage Guidelines • Entyvio® (Vedolizumab) • Evkeeza™ (Evinacumab-dgnb) • Exondys 51® (Eteplirsen) • Givlaari® (Givosiran) • Home Health Care • Ilaris® (Canakinumab) • Ilumya™ (Tildrakizumab-Asmn) • ™ ® ® ® Infliximab (Avsola , Inflectra , Remicade , Renflexis ) • Intravenous Enzyme Replacement Therapy (ERT) for Gaucher Disease • Long-Acting Injectable Antiretroviral Agents for HIV • Medical Therapies for Enzyme Deficiencies • Oncology Medication Clinical Coverage • -

Trogarzo, INN-Ibalizumab
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Trogarzo 200 mg concentrate for solution for infusion 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each vial contains 200 mg of ibalizumab (in 1.33 mL of solution). Ibalizumab is produced in murine myeloma non-secreting (NS0) cells by recombinant DNA technology. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Concentrate for solution for infusion (sterile concentrate). Colourless to slightly yellow, clear to slightly opalescent aqueous solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Trogarzo, in combination with other antiretroviral(s), is indicated for the treatment of adults infected with multidrug resistant HIV-1 infection for whom it is otherwise not possible to construct a suppressive antiviral regimen (see section 5.1). 4.2 Posology and method of administration Therapy should be initiated by a physician experienced in the management of HIV infection. Posology The recommended dose of ibalizumab is a single loading dose of 2,000 mg followed by a maintenance dose of 800 mg every 2 weeks. If the treating physician determines there is no additional clinical benefit for the patient in terms of viral load reduction, discontinuation of ibalizumab treatment should be considered, see section 5.1. Missed dose If a maintenance dose (800 mg) of ibalizumab is missed by 3 days or longer beyond the scheduled dosing day, a loading dose (2,000 mg) should be administered as early as possible. -

New Antiretroviral Data BHIVA Bournemouth 2019
New Antiretroviral Data BHIVA Bournemouth 2019 Dr. Mindy Clarke Consultant in HIV & Sexual health Brighton & Sussex University Hospital NHS Trust Honorary Senior Clinical Lecturer Brighton & Sussex Medical School COMPETING INTERESTS OF FINANCIAL VALUE > £1,000: in last 12 months • Amanda Clarke: has acted in a consultancy capacity for Gilead Sciences and ViiV Healthcare. She has received personal grants for attending conferences from Gilead Sciences. What we’ll cover • Naive– triple & dual • Switch – triple , dual, injectables • Failure • Pipeline • Guideline changes Meet Bob, Sam, IzZy & Ray Bob – been declining Rx, wants new ART, no side effects Sam – on treatment for years, lots of comorbidities wants to know about switching options IzZy –fed up of pills, wants to know about injectables Ray – multidrug resistance, detectable viral load, CD4 declining Meet Bob, Sam, IzZy & Ray Bob – been declining Rx, wants new ART, no side effects Sam – on treatment for years, lots of comorbidities wants to know about switching options IzZy –fed up of pills, wants to know about injectables Ray – multidrug resistance, detectable viral load, CD4 declining Doravirine: treatment naïve – week 96 data once/day, no food requirements Drive Ahead n=728 Drive Forward n=768 • Double blind, RCT, phase III • Double blind RCT, phase III • Doravirine/3TC/TDFvs • Doravirine vs DRV/r + EFV/FTC/TDF 2NRTIs • No resistance, VL>1,000 • No resistance, VL>1,000 copies/mL copies/mL • Week 48 primary endpoint: • Week 48 primary endpoint: 84% v 81% 84% v 80% 1. Orkin. IDWeek 2018. Abstr LB1. 2. Orkin. Clin Infect Dis. 2018;[Epub]. Molina JM, et al. AIDS 2018.