Anaplasmosis Fact Sheet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anaplasma Species of Veterinary Importance in Japan
Veterinary World, EISSN: 2231-0916 REVIEW ARTICLE Available at www.veterinaryworld.org/Vol.9/November-2016/4.pdf Open Access Anaplasma species of veterinary importance in Japan Adrian Patalinghug Ybañez1 and Hisashi Inokuma2 1. Biology and Environmental Studies Program, Sciences Cluster, University of the Philippines Cebu, Lahug, Cebu City 6000, Philippines; 2. Department of Veterinary Clinical Science, Obihiro University of Agriculture and Veterinary Medicine, Obihiro, Inada Cho, Hokkaido 080-8555, Japan. Corresponding author: Adrian Patalinghug Ybañez, e-mail: [email protected], HI: [email protected] Received: 14-06-2016, Accepted: 28-09-2016, Published online: 04-11-2016 doi: 10.14202/vetworld.2016.1190-1196 How to cite this article: Ybañez AP, Inokuma H (2016) Anaplasma species of veterinary importance in Japan, Veterinary World, 9(11): 1190-1196. Abstract Anaplasma species of the family Anaplasmataceae, order Rickettsiales are tick-borne organisms that can cause disease in animals and humans. In Japan, all recognized species of Anaplasma (except for Anaplasma ovis) and a potentially novel Anaplasma sp. closely related to Anaplasma phagocytophilum have been reported. Most of these detected tick- borne pathogens are believed to be lowly pathogenic in animals in Japan although the zoonotic A. phagocytophilum has recently been reported to cause clinical signs in a dog and in humans. This review documents the studies and reports about Anaplasma spp. in Japan. Keywords: Anaplasma spp., Japan, tick-borne pathogen. Introduction A. phagocytophilum sequences [10-15]. Phylogenetic Anaplasma species are Gram-negative, obligate inferences have suggested that 2 clades exist within intracellular bacteria of the order Rickettsiales, fam- the genus Anaplasma: (1) Erythrocytic (A. -

Tick Borne Diseases Nebraska 2018 HAN FINAL DRAFT APRIL 19 2018
TO: Primary care providers, infectious disease, laboratories, infection control, and public health FROM Thomas J. Safranek, M.D. Jeff Hamik State Epidemiologist Vector-borne Disease Epidemiologist 402-471-2937 PHONE 402-471-1374 PHONE 402-471-3601 FAX 402-471-3601 FAX Thomas Williams, M.D. Chief Medical Officer Director, Division of Public Health Department of Health and Human Services RE: TICK-BORNE DISEASES IN NEBRASKA DATE: April 20, 2018 The arrival of spring marks the beginning of another tick season. In the interest of public health and prevention, our office seeks to inform Nebraska health care providers about the known tick- borne diseases in our state. Key messages for Nebraska clinicians: Spotted fever rickettsia including Rocky Mountain spotted fever (RMSF) Our office receives reports of from 6 to 31 patients with spotted fever rickettsia every year. Health care providers risk overlooking this diagnosis because of its rarity. RMSF NEEDS TO BE A DIAGNOSTIC CONSIDERATION IN ANY PERSON WITH A FEVER AND A HISTORY OF EXPOSURE TO ENVIRONMENTS WHERE TICKS MIGHT BE PRESENT. The skin rash is not always present when the patient first presents to a physician. This disease is frequently overlooked or misdiagnosed, with numerous reports of serious and sometimes fatal consequences. Nebraska experienced a fatal case of RMSF in 2015 where the diagnosis was missed and treatment was delayed until the disease was well advanced. Laboratory diagnosis is made by detecting a rise in antibody titer to Rickettsia rickettsii between acute and convalescent sera. Treatment requires tetracycline-class of antibiotics or chloramphenicol. Tetracycline-class treatment is recommended for persons of all ages, including children. -

Anaplasmosis: an Emerging Tick-Borne Disease of Importance in Canada
IDCases 14 (2018) xxx–xxx Contents lists available at ScienceDirect IDCases journal homepage: www.elsevier.com/locate/idcr Case report Anaplasmosis: An emerging tick-borne disease of importance in Canada a, b,c d,e e,f Kelsey Uminski *, Kamran Kadkhoda , Brett L. Houston , Alison Lopez , g,h i c c Lauren J. MacKenzie , Robbin Lindsay , Andrew Walkty , John Embil , d,e Ryan Zarychanski a Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, University of Manitoba, Winnipeg, MB, Canada b Cadham Provincial Laboratory, Government of Manitoba, Winnipeg, MB, Canada c Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Medical Microbiology and Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada d Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Medical Oncology and Hematology, University of Manitoba, Winnipeg, MB, Canada e CancerCare Manitoba, Department of Medical Oncology and Hematology, Winnipeg, MB, Canada f Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Pediatrics and Child Health, Section of Infectious Diseases, Winnipeg, MB, Canada g Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada h Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Community Health Sciences, University of Manitoba, Winnipeg, MB, Canada i Public Health Agency of Canada, National Microbiology Laboratory, Zoonotic Diseases and Special Pathogens, Winnipeg, MB, Canada A R T I C L E I N F O A B S T R A C T Article history: Human Granulocytic Anaplasmosis (HGA) is an infection caused by the intracellular bacterium Received 11 September 2018 Anaplasma phagocytophilum. -

Ehrlichiosis and Anaplasmosis Are Tick-Borne Diseases Caused by Obligate Anaplasmosis: Intracellular Bacteria in the Genera Ehrlichia and Anaplasma
Ehrlichiosis and Importance Ehrlichiosis and anaplasmosis are tick-borne diseases caused by obligate Anaplasmosis: intracellular bacteria in the genera Ehrlichia and Anaplasma. These organisms are widespread in nature; the reservoir hosts include numerous wild animals, as well as Zoonotic Species some domesticated species. For many years, Ehrlichia and Anaplasma species have been known to cause illness in pets and livestock. The consequences of exposure vary Canine Monocytic Ehrlichiosis, from asymptomatic infections to severe, potentially fatal illness. Some organisms Canine Hemorrhagic Fever, have also been recognized as human pathogens since the 1980s and 1990s. Tropical Canine Pancytopenia, Etiology Tracker Dog Disease, Ehrlichiosis and anaplasmosis are caused by members of the genera Ehrlichia Canine Tick Typhus, and Anaplasma, respectively. Both genera contain small, pleomorphic, Gram negative, Nairobi Bleeding Disorder, obligate intracellular organisms, and belong to the family Anaplasmataceae, order Canine Granulocytic Ehrlichiosis, Rickettsiales. They are classified as α-proteobacteria. A number of Ehrlichia and Canine Granulocytic Anaplasmosis, Anaplasma species affect animals. A limited number of these organisms have also Equine Granulocytic Ehrlichiosis, been identified in people. Equine Granulocytic Anaplasmosis, Recent changes in taxonomy can make the nomenclature of the Anaplasmataceae Tick-borne Fever, and their diseases somewhat confusing. At one time, ehrlichiosis was a group of Pasture Fever, diseases caused by organisms that mostly replicated in membrane-bound cytoplasmic Human Monocytic Ehrlichiosis, vacuoles of leukocytes, and belonged to the genus Ehrlichia, tribe Ehrlichieae and Human Granulocytic Anaplasmosis, family Rickettsiaceae. The names of the diseases were often based on the host Human Granulocytic Ehrlichiosis, species, together with type of leukocyte most often infected. -

Anaplasmosis
Anaplasmosis Definition: Anaplasmosis is an infection caused by the bacterium Anaplasma phagocytophilum. It is most commonly transmitted by the bite of an infected deer tick (Ixodes scapularis). Signs and symptoms: Symptoms of anaplasmosis can range from mild to very severe and may include: fever, headache, muscle pain, malaise, chills, nausea, abdominal pain, cough, and confusion. Severe symptoms may include: difficulty breathing, hemorrhage, renal failure, or neurological problems. It can be fatal if not treated correctly. People who are immunocompromised or elderly are at higher risk for severe disease. Transmission: Anaplasmosis is primarily transmitted to a person through the bite of an infected deer tick; this tick is endemic throughout Maine. Rarely, it can also be transmitted by receiving blood transfusions from an infected donor. Diagnosis: Anaplasmosis is diagnosed by clinical symptoms and laboratory tests. A blood test is necessary for confirmation. Co-infections with other tick-borne diseases may occur and should be considered. Role of the School Nurse: Prevention • Provide education on prevention efforts including: wearing protective clothing, using an EPA- approved repellent, using caution in tick infested areas, and performing daily tick checks. • Encourage the use of EPA approved repellents when outside (following local policy guidelines), and always performing a tick check when returning indoors. o School nurses can apply repellent with parental permission • If a tick is found, the school nurse should remove the tick using tweezers or a tick spoon. o Tick identification cards are available at: http://www.maine.gov/dhhs/mecdc/infectious- disease/epi/vector-borne/posters/index.shtml. o Testing of the tick is not recommended. -

Human Granulocytic Anaplasmosis (HGA)
MASSACHUSETTS DEPARTMENT OF PUBLIC HEALTH FACT SHEET Human Granulocytic Anaplasmosis (HGA) April 2014 | Page 1 of 3 What is human granulocytic anaplasmosis (HGA)? HGA is caused by bacteria (germs) that attack certain types of white blood cells called granulocytes. HGA is also known as human granulocytic ehrlichiosis. Where do cases of HGA occur? In the United States, HGA is most commonly found in the Northeast, mid-Atlantic and upper Midwest. In Massachusetts, the highest rates of disease occur on the islands of Nantucket and Martha’s Vineyard and in Barnstable and Berkshire counties, but it can occur anywhere in the state. How is HGA spread? HGA is one of the diseases that can be spread by the bite of an infected deer tick. The longer a tick remains attached and feeding, the higher the likelihood that it may spread the bacteria. Deer ticks in Massachusetts can also carry the germs that cause Lyme disease and babesiosis. Deer ticks are capable of spreading more than one type of germ in a single bite. When can I get HGA? HGA can occur during any time of year. The bacteria that cause HGA are spread by infected deer ticks. Young ticks (nymphs) are most active during the warm weather months between May and July. Adult ticks are most active during the fall and spring but will also be out searching for a host any time that winter temperatures are above freezing. How soon do symptoms of HGA appear after a tick bite? Symptoms of HGA usually begin to appear 7 to 14 days after being bitten by an infected tick. -

Ixodes Scapularis) Affected Species: Humans PATHOBIOLOGY and VETERINARY SCIENCE • CONNECTICUT VETERINARY MEDICAL DIAGNOSTIC LABORATORY
Tick Borne Diseases In New England Bullseye rash- common symptom of Lyme disease and STARI Skin lesions- common symptom of Tularemia Tularemia Rocky Mountain Spotted Fever Agent: Rickettsia rickettsii Agent: Francisella tularensis Brown Dog Tick Symptoms: fever, “spotted” rash, headache, nausea, Symptoms: fever, skin lesions in people, vomiting, abdominal pain, muscle pain, lack of appetite, face and eyes redden and become (Rhipicephalus sanguineus) red eyes inflamed, chills, headache, exhaustion Affected Species: humans, dogs Affected Species: humans, rabbits, rodents, cats, dogs, sheep, many Dog Tick mammalian species (Dermacentor variabilis) Ehrlichiosis Agent: Ehrlichia chaffeensis and Ehrlichia ewingii Symptoms: fever, headache, chills, muscle pain, nausea, vomiting, diarrhea, confusion, red eyes Affected Species: humans, dogs, cats Babesiosis Anaplasmosis Agent: Babesia microti Agent: Anaplasma phagocytophilum Symptoms: (many show none), fever, chills, sweats, Lone star tick Symptoms: fever, severe headache, muscle aches, headache, body aches, loss of appetite, nausea chills and shaking, nausea, vomiting, abdominal pain Affected Species: humans (Amblyomma americanum) Affected Species: humans, dogs, horses, cows Borrelia miyamotoi Disease Agent: Borrelia miyamotoi Southern Tick-Associated Lyme Disease Symptoms: fever, chills, headache, body and joint Agent: Borrelia burgdorferi pain, fatigue Rash Illness (STARI) Symptoms: “bullseye” rash Affected Species: humans Agent: Borrelia lonestari (humans only), fever, aching joints, Symptoms: “bullseye” rash, fatigue, muscle pains, headache, fatigue, neurological headache involvement Affected Species: humans Affected Species: humans, Powassan Virus horses, dogs, many others Agent: Powassan Virus Symptoms: (many show none), fever, headache, vomiting, weakness, confusion, loss of coordination, Deer Tick speech difficulties, seizures (Ixodes scapularis) Affected Species: humans PATHOBIOLOGY AND VETERINARY SCIENCE • CONNECTICUT VETERINARY MEDICAL DIAGNOSTIC LABORATORY. -

Tick-Borne Diseases in Maine a Physician’S Reference Manual Deer Tick Dog Tick Lonestar Tick (CDC Photo)
tick-borne diseases in Maine A Physician’s Reference Manual Deer Tick Dog Tick Lonestar Tick (CDC PHOTO) Nymph Nymph Nymph Adult Male Adult Male Adult Male Adult Female Adult Female Adult Female images not to scale know your ticks Ticks are generally found in brushy or wooded areas, near the DEER TICK DOG TICK LONESTAR TICK Ixodes scapularis Dermacentor variabilis Amblyomma americanum ground; they cannot jump or fly. Ticks are attracted to a variety (also called blacklegged tick) (also called wood tick) of host factors including body heat and carbon dioxide. They will Diseases Diseases Diseases transfer to a potential host when one brushes directly against Lyme disease, Rocky Mountain spotted Ehrlichiosis anaplasmosis, babesiosis fever and tularemia them and then seek a site for attachment. What bites What bites What bites Nymph and adult females Nymph and adult females Adult females When When When April through September in Anytime temperatures are April through August New England, year-round in above freezing, greatest Southern U.S. Coloring risk is spring through fall Adult females have a dark Coloring Coloring brown body with whitish Adult females have a brown Adult females have a markings on its hood body with a white spot on reddish-brown tear shaped the hood Size: body with dark brown hood Unfed Adults: Size: Size: Watermelon seed Nymphs: Poppy seed Nymphs: Poppy seed Unfed Adults: Sesame seed Unfed Adults: Sesame seed suMMer fever algorithM ALGORITHM FOR DIFFERENTIATING TICK-BORNE DISEASES IN MAINE Patient resides, works, or recreates in an area likely to have ticks and is exhibiting fever, This algorithm is intended for use as a general guide when pursuing a diagnosis. -

Detection of Tick-Borne Pathogens of the Genera Rickettsia, Anaplasma and Francisella in Ixodes Ricinus Ticks in Pomerania (Poland)
pathogens Article Detection of Tick-Borne Pathogens of the Genera Rickettsia, Anaplasma and Francisella in Ixodes ricinus Ticks in Pomerania (Poland) Lucyna Kirczuk 1 , Mariusz Piotrowski 2 and Anna Rymaszewska 2,* 1 Department of Hydrobiology, Faculty of Biology, Institute of Biology, University of Szczecin, Felczaka 3c Street, 71-412 Szczecin, Poland; [email protected] 2 Department of Genetics and Genomics, Faculty of Biology, Institute of Biology, University of Szczecin, Felczaka 3c Street, 71-412 Szczecin, Poland; [email protected] * Correspondence: [email protected] Abstract: Tick-borne pathogens are an important medical and veterinary issue worldwide. Environ- mental monitoring in relation to not only climate change but also globalization is currently essential. The present study aimed to detect tick-borne pathogens of the genera Anaplasma, Rickettsia and Francisella in Ixodes ricinus ticks collected from the natural environment, i.e., recreational areas and pastures used for livestock grazing. A total of 1619 specimens of I. ricinus were collected, including ticks of all life stages (adults, nymphs and larvae). The study was performed using the PCR technique. Diagnostic gene fragments msp2 for Anaplasma, gltA for Rickettsia and tul4 for Francisella were ampli- fied. No Francisella spp. DNA was detected in I. ricinus. DNA of A. phagocytophilum was detected in 0.54% of ticks and Rickettsia spp. in 3.69%. Nucleotide sequence analysis revealed that only one species of Rickettsia, R. helvetica, was present in the studied tick population. The present results are a Citation: Kirczuk, L.; Piotrowski, M.; part of a large-scale analysis aimed at monitoring the level of tick infestation in Northwest Poland. -

Detection of Babesia Odocoilei in Ixodes Scapularis Ticks Collected from Songbirds in Ontario and Quebec, Canada
pathogens Article Detection of Babesia odocoilei in Ixodes scapularis Ticks Collected from Songbirds in Ontario and Quebec, Canada John D. Scott *, Emily L. Pascoe , Muhammad S. Sajid and Janet E. Foley Department of Medicine and Epidemiology, School of Veterinary Medicine, University of California Davis, Davis, CA 95616, USA; [email protected] (E.L.P.); [email protected] (M.S.S.); [email protected] (J.E.F.) * Correspondence: [email protected] Received: 19 August 2020; Accepted: 16 September 2020; Published: 24 September 2020 Abstract: Songbirds widely disperse ticks that carry a diversity of pathogens, some of which are pathogenic to humans. Among ticks commonly removed from songbirds, the blacklegged tick, Ixodes scapularis, can harbor any combination of nine zoonotic pathogens, including Babesia species. From May through September 2019, a total 157 ticks were collected from 93 songbirds of 29 species in the Canadian provinces of Ontario and Québec. PCR testing for the 18S gene of Babesia species detected Babesia odocoilei in 12.63% of I. scapularis nymphs parasitizing songbirds in Ontario and Québec; none of the relatively small numbers of Ixodes muris, Ixodes brunneus, or Haemaphysalis leporispalustris were PCR-positive. For ticks at each site, the prevalence of B. odocoilei was 16.67% in Ontario and 8.89% and 5.26% in Québec. Of 31 live, engorged I. scapularis larvae and nymphs held to molt, 25 ticks completed the molt; five of these molted ticks were positive for B. odocoilei. PCR-positive ticks were collected from six bird species—namely, Common Yellowthroat, Swainson’s Thrush, Veery, House Wren, Baltimore Oriole, and American Robin. -
Cattle Combination with Decoquinate
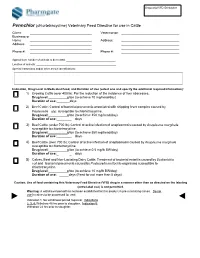
Sequential VFD ID Number Pennchlor (chlortetracycline) Veterinary Feed Directive for use in Cattle Client: __________________________________ Veterinarian: ________________________________ Business or Home __________________________________ Address: ________________________________ Address: __________________________________ ________________________________ __________________________________ ________________________________ Phone #: __________________________________ Phone #: ________________________________ Approximate number of animals to be treated: __________________________________ Location of animals: _______________________________________________________ Special Instructions and/or other animal identifications: Indication, Drug Level in Medicated Feed, and Duration of Use (select one and specify the additional required information): 1) Growing Cattle (over 400 lb): For the reduction of the incidence of liver abscesses. Drug level: g/ton (to achieve 70 mg/head/day) Duration of use:_ days 2) Beef Cattle: Control of bacterial pneumonia associated with shipping fever complex caused by Pasteurella spp. susceptible to chlortetracycline. Drug level: g/ton (to achieve 350 mg/head/day) Duration of use:_ _ days 3) Beef Cattle (under 700 lb): Control of active infection of anaplasmosis caused by Anaplasma marginale susceptible to chlortetracycline. Drug level: g/ton (to achieve 350 mg/head/day) Duration of use:_ _ days 4) Beef Cattle (over 700 lb): Control of active infection of anaplasmosis caused by Anaplasma marginale susceptible to chlortetracycline. -

Ehrlichiosis and Anaplasmosis
Ehrlichiosis and Anaplasmosis The Diseases and Transmission Ehrlichia and Anaplasma are related bacteria that are transmitted by ticks. These bacteria infect white blood cells in humans. There are three different bacteria that cause disease in humans: Anaplasma phagocytophilum Ehrlichia chaffeensis Ehrlichia ewingii Pathogen (formerly Ehrlichia phagocytophila) Human monocytic Human granulocytic Disease Ehrlichiosis ewingii ehrlichiosis (HME) anaplasmosis (HGA, formerly HGE) Tick Vector Amblyomma americanum (lone star tick) Ixodes scapularis (black-legged tick) Animal reservoirs for E. chaffeensis and E. ewingii are white-tailed deer and dogs. The reservoirs for A. phagocytophilum include cattle, deer, and rodents. You cannot get the diseases directly from animals. The diseases are not spread between humans other than through blood transfusions. Maryland is home to both the lone star tick and the black-legged tick. Symptoms and Treatment Disease Clinical Features . Symptoms appear 7 to 10 days after a tick bite. Symptoms include fever, headache, muscle aches, nausea, vomiting, HME, and loss of appetite. Ehrlichiosis ewingii . Meningoencephalitis occurs in approximately 20% of cases. Development of a rash is possible. This may be confused with Rocky Mountain spotted fever. Symptoms appear 7 to 14 days after a tick bite. HGA . Symptoms include fever, headache, and muscle aches. Meningoencephalitis is rare. Most infections occur when tick activity is highest, in late spring and summer. If left untreated, HME and HGA may be severe. Co-infection with more than one tick borne disease is possible. The immune system is directly infected. Secondary infection and other complications can arise quickly. The elderly and sick are more likely to develop severe illness.