The Role of Law Enforcement in Public Health Emergencies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Healthy Action: an Activity Book for Teachers and Learners
Healthy Action: An Activity Book for Teachers and Learners Acknowledgements This Activity Book was written by Scott Pulizzi and Laurie Rosenblum of Education Development Center, Inc. (EDC), Health and Human Development Division (HHD). The authors worked in close partnership with the staff of the Solidarity and Development Unit coordinating the EFAIDS Programme at Education International (EI). The authors acknowledge the contribution of the World Health Organization (WHO). EI, EDC, and WHO would also like to acknowledge all the teachers’ unions affiliated to EI who have contributed to the EFAIDS Programme and thus to this Activity Book, specifically and the Zimbabwe Teachers’ Association. EI, EDC, and WHO are supported by the Dutch Ministry of Foreign Affairs’ Directorate- General for International Cooperation (DGIS) under the EFAIDS Programme. All photographs taken by Josephine Krikke. Acknowledgements 3 Table of Contents Introduction ................................................... 7 Tobacco Use and Prevention .......................... 11 Alcohol and Other Drugs................................ 27 Nutrition ......................................................... 37 Physical Activity ............................................. 55 Hygiene and Sanitation .................................. 69 Injury Prevention ........................................... 83 Violence Prevention ........................................ 95 Table of Contents 5 Introduction This toolkit is based on the premise that healthy students and teachers live better. -

PERFORMED IDENTITIES: HEAVY METAL MUSICIANS BETWEEN 1984 and 1991 Bradley C. Klypchak a Dissertation Submitted to the Graduate
PERFORMED IDENTITIES: HEAVY METAL MUSICIANS BETWEEN 1984 AND 1991 Bradley C. Klypchak A Dissertation Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY May 2007 Committee: Dr. Jeffrey A. Brown, Advisor Dr. John Makay Graduate Faculty Representative Dr. Ron E. Shields Dr. Don McQuarie © 2007 Bradley C. Klypchak All Rights Reserved iii ABSTRACT Dr. Jeffrey A. Brown, Advisor Between 1984 and 1991, heavy metal became one of the most publicly popular and commercially successful rock music subgenres. The focus of this dissertation is to explore the following research questions: How did the subculture of heavy metal music between 1984 and 1991 evolve and what meanings can be derived from this ongoing process? How did the contextual circumstances surrounding heavy metal music during this period impact the performative choices exhibited by artists, and from a position of retrospection, what lasting significance does this particular era of heavy metal merit today? A textual analysis of metal- related materials fostered the development of themes relating to the selective choices made and performances enacted by metal artists. These themes were then considered in terms of gender, sexuality, race, and age constructions as well as the ongoing negotiations of the metal artist within multiple performative realms. Occurring at the juncture of art and commerce, heavy metal music is a purposeful construction. Metal musicians made performative choices for serving particular aims, be it fame, wealth, or art. These same individuals worked within a greater system of influence. Metal bands were the contracted employees of record labels whose own corporate aims needed to be recognized. -

PERSONAL and COMMUNITY HEALTH (PCH): 14 Days
MIDDLE SCHOOL (GRADE 7) HEALTH EDUCATION UNIT PLANNING GUIDE (revised 6/2009) Page 1 of 15 PERSONAL AND COMMUNITY HEALTH (PCH): 14 days Text Chapter 1, 2, 5 Chapters 12, 13 Chapter 15 Chapter 15 Sub-Unit: Personal Health Sub-Unit: Disease Prevention Sub-Unit: Environmental Health Sub-Unit: Community Health EC 1.1.P Describe the 1.3.P Identify Standard 1.9.P Identify ways that 1.11.P Describe global influences importance of health- (Universal) Precautions and why environmental factors, including on personal and community health. management strategies (e.g., they are important. (also IPS, air quality, affect our health. those involving adequate sleep, GDSH) 1.10.P Identify human activities ergonomics, sun safety, 1.4.P Examine the causes and that contribute to environmental hearing protection, and self symptoms of communicable and challenges (e.g., air, water an noise examination). non-communicable diseases. pollution). 1.2.P Identify the importance of age-appropriate medical services. 1.5.P Discuss the importance of effective personal and dental hygiene practices for preventing illness. 1.6.P Identify effective brushing and flossing techniques for oral care. 1.7.P Identify effective protection for teeth, eyes, head, and neck during sports and recreation activities. (also IPS) 1.8.P Identify ways to prevent vision or hearing damage. 1.12.P Identify ways to reduce exposure to the sun. AI 2.1.P Analyze a variety of 2.2.P Analyze how environmental influences that affect personal pollutants, including noise pollution, health practices. affect health. 2.4.P Analyze the influence of 2.3.P Analyze the relationship culture, media, and technology on between the health of a community health decisions. -

Federal Register / Vol. 62, No. 221 / Monday, November 17, 1997 / Notices Respondent Burden
61336 Federal Register / Vol. 62, No. 221 / Monday, November 17, 1997 / Notices respondent burden. The total annual burden hours are 500. No. of Avg. burden/ Project No. of responses/ response respondents respondent (in hrs.) QDRL Laboratory Interviews: (1) NHIS modules ................................................................................................................. 150 1 1.0 (2) Behavioral Risk Factors Survey ...................................................................................... 100 1 1.0 (3) Other Questionnaire Testing: .......................................................................................... 1998 ............................................................................................................................... 200 1 1.0 1999 ............................................................................................................................... 200 1 1.0 2000 ............................................................................................................................... 200 1 1.0 (4) Perceptions of Quality of Life Project .............................................................................. 100 1 1.0 (5) Perceptions of Confidentiality Project ............................................................................. 50 1 1.0 (6) Perception of Statistical Maps Project ............................................................................ 100 1 1.0 (7) General Methodological Research ................................................................................. -

Social Media and Tactical Considerations for Law Enforcement
Social Media and Tactical Considerations For Law Enforcement This project was supported by Cooperative Agreement Number 2011-CK-WX-K016 awarded by the Office of Community Oriented Policing Services, U.S. Department of Justice. The opinions contained herein are those of the author(s) and do not necessarily represent the official position or policies of the U.S. Department of Justice. References to specific agencies, companies, products, or services should not be considered an endorsement by the author(s) or the U.S. Department of Justice. Rather, the references are illustrations to supplement discussion of the issues. The Internet references cited in this publication were valid as of the date of this publication. Given that URLs and websites are in constant flux, neither the author(s) nor the COPS Office can vouch for their current validity. ISBN: 978-1-932582-72-7 e011331543 July 2013 A joint project of: U.S. Department of Justice Police Executive Research Forum Office of Community Oriented Policing Services 1120 Connecticut Avenue, N.W. 145 N Street, N.E. Suite 930 Washington, DC 20530 Washington, DC 20036 To obtain details on COPS Office programs, call the COPS Office Response Center at 800-421-6770. Visit COPS Online at www.cops.usdoj.gov. Contents Foreword ................................................................. iii Acknowledgments ........................................................... iv Introduction ............................................................... .1 Project Background......................................................... -

2018 Deer Hunting Regulations
2018 WISCONSIN Deer Hunting Regulations Photo by Brad Holtz Katie Hettel harvested this buck while hunting with family and friends in Florence County. Katie has been deer hunting for 14 years and this is her second buck. This 9-pointer was observed on trail cameras around the property a week prior to the season, and on opening morning of the 9-day gun deer season, Katie harvested it with a clean shot at 40 yards. Congratulations, Katie! WISCONSIN DEPARTMENT OF NATURAL RESOURCES PUB-WM-431 2018 This pamphlet gives you a summary of Wisconsin’s important deer hunting laws and how they affect you; it is not a complete set of all the hunting- related laws. Wisconsin Deer Hunting Basics This guide outlines the basics of what you need to know to hunt deer in Wisconsin in 2018. 1. What’s New in 2018 4. Carry proof of your deer harvest authorizations ► Several deer management zone and metro sub-unit boundaries have changed. See You are not required to validate or attach a paper harvest authorization pages 24 - 27. (formerly known as “deer carcass tag”) to the deer, but you must still carry ► Several DMUs will offer an extended, any-deer archery season through Jan. 31, 2019. See page 10. proof of your harvest authorization. Three main deer harvest authorization ► Deer tags are now referred to as “harvest authorizations.” Hunters must still carry proof types are offered, but you may be eligible for one or more of the other of a hunting license and deer harvest authorizations while afield. antlerless harvest authorization types listed on pages 14 - 16. -

Hunting Deer in California
HUNTING DEER IN CALIFORNIA We hope this guide will help deer hunters by encouraging a greater understanding of the various subspecies of mule deer found in California and explaining effective hunting techniques for various situations and conditions encountered throughout the state during general and special deer seasons. Second Edition August 2002 STATE OF CALIFORNIA Arnold Schwarzenegger, Governor DEPARTMENT OF FISH AND GAME L. Ryan Broddrick, Director WILDLIFE PROGRAMS BRANCH David S. Zezulak, Ph.D., Chief Written by John Higley Technical Advisors: Don Koch; Eric Loft, Ph.D.; Terry M. Mansfield; Kenneth Mayer; Sonke Mastrup; Russell C. Mohr; David O. Smith; Thomas B. Stone Graphic Design and Layout: Lorna Bernard and Dana Lis Cover Photo: Steve Guill Funded by the Deer Herd Management Plan Implementation Program TABLE OF CON T EN T S INTRODUCT I ON ................................................................................................................................................5 CHAPTER 1: THE DEER OF CAL I FORN I A .........................................................................................................7 Columbian black-tailed deer ....................................................................................................................8 California mule deer ................................................................................................................................8 Rocky Mountain mule deer .....................................................................................................................9 -

Kickbacks, Honest Services, and Health Care Fraud After Skilling Joan H
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of North Carolina School of Law University of North Carolina School of Law Carolina Law Scholarship Repository Faculty Publications Faculty Scholarship 2012 Kickbacks, Honest Services, and Health Care Fraud After Skilling Joan H. Krause University of North Carolina School of Law, [email protected] Follow this and additional works at: http://scholarship.law.unc.edu/faculty_publications Part of the Law Commons Publication: Annals of Health Law This Article is brought to you for free and open access by the Faculty Scholarship at Carolina Law Scholarship Repository. It has been accepted for inclusion in Faculty Publications by an authorized administrator of Carolina Law Scholarship Repository. For more information, please contact [email protected]. Kickbacks, Honest Services, and Health Care Fraud After Skilling Joan H Krause· This essay considers how the 2010 Supreme Court decision in Skilling v. United States', which limited the situations in which mail and wire fraud cases may be premised on violations of the "intangible right to honest services," has the potential to alter the future of health care fraud enforcement. To be clear, Skilling was not a healthcare case. Rather, the litigation stemmed from the investigation of Enron's former CEO, Jeffrey Skilling, who was accused of engaging in a conspiracy to commit honest services wire fraud as well as multiple forms of securities-related fraud. In rejecting a vagueness challenge to the honest services theory, however, the Court read the statute in a very narrow way that puts kickbacks and bribery cases squarely in the crosshairs, an approach that may have serious implications for healthcare fraud. -

Remote Sensing for Post Disaster Management of Freight Transportation Networks
Final Report Remote Sensing for Post Disaster Management of Freight Transportation Networks Shahram Pezeshk, Ph.D., P.E Gregory Taff, Ph.D. Charles V. Camp, Ph.D. and Mathew J. Bolton, Graduate Student ABSTRACT • ii ABSTRACT • ii ABSTRACT In the event of a natural disaster, assessing the status of our transportation network and repairing it is of critical importance to recovery efforts. We must also consider terrorist attacks worldwide in terms of infrastructure integrity assessment and recovery. Major roadways, if damaged at key locations, can be rendered useless for commercial traffic and more importantly, for emergency response and law enforcement vehicles. The delay or inability to answer emergency calls can lead to the loss of numer- ous lives. With the use of several geographic techniques and tools, these dangers can be minimized. This report documents the test of developing a method of research utilizing remote sensing tech- niques to detect damage to road bridges. Through using derived pixel data and algorithms, pre- and post- earthquake images are compared to identify difference in the pixels’ brightness values (BV’s). With these techniques we can develop an expedient assessment of the transportation infrastructure’s integrity throughout Shelby County, Tennessee if it were to play host to one of these disastrous evens. These techniques could be implemented throughout the rest of the world. This research develops methodology for damage detection for a possible future event. Our goal was to test these methods of bridges change detection on an area for which we have data on the integrity of multiple bridges (damaged or not), and high spatial resolution imagery of both before and after an earthquake. -

Health Law: a Career Guide
Health Law: A Career Guide Written By: Catherine Pattanayak, Assistant Director Joan Ruttenberg, Director of the Heyman Fellowship Program & Annelise Eaton, 2012 Summer Fellow Bernard Koteen Office of Public Interest Advising Wasserstein Hall Suite 4039 www.law.harvard.edu/current/careers/opia Table of Contents ___________________________ Section I: An Introduction to Health Law…p. 1 Section II: Health Law Issue Areas…p. 4 Section III: Health Law Practice Settings…p. 10 Section IV: Types of Practice…p. 16 Section V: Planning Your Public Interest Health Law Career…p. 20 Section VI: Professional Narratives…p. 25 Section VII: Extracurricular Activities…p. 33 Section VIII: Health Law Courses throughout Harvard University…p. 35 Section IX: Selected Health Law Organizations…p. 39 Section X: Health Law Fellowships, Honors Programs, and Entry-Level Hiring…p. 46 Section I: An Introduction to Health Law Health law is an incredibly broad, diverse and dynamic field of law. Health lawyers work on cases and policy relating to access to care, insurance coverage, difficult ethical choices (particularly at the beginning and end of life), providers of care (and how these providers are organized and paid), the safety of our drugs and food supply, disease prevention and treatment, and many other fascinating topics. In part because of the breadth of the field, health law also cuts across and involves doctrine and practice from a wide array of areas, including contract law, tax law, corporations and nonprofit organization, insurance and pension law, employment and labor law, public benefits law, torts, ethics, criminal law, administrative law, Organization Profile: privacy, civil rights, reproductive rights, New York Lawyers for the Public Interest (NYLPI) constitutional law, and statutory drafting and www.nylpi.org interpretation—even First Amendment religious liberty and freedom of speech concepts can be Since the 1970s, New York Lawyers for the Public implicated in the field of health law. -
First Do No Harm: Advancing Public Health in Policing Practices Contents
M PROGRA H First Do No Harm: Advancing Public Health in Policing Practices E AND MENTAL HEALT E AND MENTAL US NOVEMBER 2015 TANCE TANCE S SUB David Cloud • Chelsea Davis FROM THE PRESIDENT First Do No Harm addresses the disconnect between law enforcement and public health systems, which has resulted in an ineffective default response of arrest, incarcerate, and repeat for some of our society’s most vulnerable mem- bers—people living in poverty, using drugs, or living with mental illness. The now well-documented and contemporaneous failures of the war on drugs and the movement to deinstitutionalize people with serious mental illness and intellectual disabilities illuminate the need for a cohesive response among system actors to society’s ills. As you read this report, it will be clear to you that the money and resources spent rooting out and arresting people suffering from illness and addiction are far better reserved for finding alterna- tives that connect them to treatment and care. Otherwise, the burden is placed on law enforcement officers to provide a means of relief or otherwise send sick and impoverished people to overcrowded cells and through the wringer of the criminal justice system. Recent national health care reform and bipartisan calls for criminal justice reform present an opportunity to course correct. Our public services must bet- ter align themselves to address the health disparities that arise from poverty and the lack of proper treatment and care. In the case of Gloucester, Massachu- setts—which had seen an uptick in heroin-related deaths—the police chief has offered the city’s precincts as sanctuary to people with drug addictions where they can be directly connected to treatment without fear of arrest or incarcera- tion. -
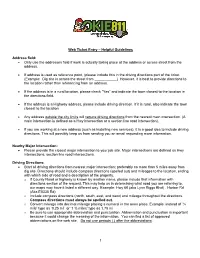
Web Ticket Entry – Helpful Guidelines Address Field
Web Ticket Entry – Helpful Guidelines Address field: Only use the addresses field if work is actually taking place at the address or across street from the address. If address is used as reference point, (please include this in the driving directions part of the ticket. (Example: Dig site is across the street from ___________) However, it is best to provide directions to the location rather than referencing from an address. If the address is in a rural location, please check “Yes” and indicate the town closest to the location in the directions field. If the address is a Highway address, please include driving direction. If it is rural, also indicate the town closest to the location Any address outside the city limits will require driving directions from the nearest main intersection. (A main intersection is defined as a Hwy intersection or a section line road intersection). If you are working at a new address (such as installing new services), it is a good idea to include driving directions. This will possibly keep us from sending you an email requesting more information. Nearby Major Intersection: Please provide the closest major intersection to your job site. Major intersections are defined as Hwy intersections, section line road intersections. Driving Directions: Start all driving directions from nearest major intersection; preferably no more than 5 miles away from dig site. Directions should include compass directions (spelled out) and mileages to the location, ending with which side of road and a description of the property. o If County Road or highway is known by another name, please include that information with directions section of the request.