Milestones in Oncology: Events That Changed the Course of Cancer Therapy and Implications for the Future
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Issue
Cell Circuitry || Science Teaches English || The Chicken Genome Is Hot || Magnets in Medicine SEPTEMBER 2002 www.hhmi.org/bulletin Leading Doublea Life It’s a stretch, but doctors who work bench to bedside say they wouldn’t do it any other way. FEATURES 14 On Human Terms 24 The Evolutionary War A small—some say too small—group of Efforts to undermine evolution education have physician-scientists believes the best science evolved into a 21st-century marketing cam- requires patient contact. paign that relies on legal acumen, manipulation By Marlene Cimons of scientific literature and grassroots tactics. 20 Engineering the Cell By Trisha Gura Adam Arkin sees the cell as a mechanical system. He hopes to transform molecular 28 Call of the Wild biology into a kind of cellular engineering Could quirky, new animal models help scien- and in the process, learn how to move cells tists learn how to regenerate human limbs or from sickness to health. avert the debilitating effects of a stroke? By M. Mitchell Waldrop By Kathryn Brown 24 In front of a crowd of 1,500, Ohio’s Board of Education heard testimony on whether students should learn about intelligent design in science class. DEPARTMENTS 2 NOTA BENE 33 PERSPECTIVE ulletin Intelligent Design Is a Cop-Out 4 LETTERS September 2002 || Volume 15 Number 3 NEWS AND NOTES HHMI TRUSTEES PRESIDENT’S LETTER 5 JAMES A. BAKER, III, ESQ. 34 Senior Partner, Baker & Botts A Creative Influence In from the Fields ALEXANDER G. BEARN, M.D. Executive Officer, American Philosophical Society 35 Lost on the Tip of the Tongue Adjunct Professor, The Rockefeller University UP FRONT Professor Emeritus of Medicine, Cornell University Medical College 36 Biology by Numbers FRANK WILLIAM GAY 6 Follow the Songbird Former President and Chief Executive Officer, SUMMA Corporation JAMES H. -

2007 Keio Medical Science Prize Winner Announcement
FOR IMMEDIATE RELEASE http://www.keio.ac.jp/ September 26, 2007 2007 Keio Medical Science Prize Winner Announcement Keio University presents the “Keio Medical Science Prize” to researchers in recognition of their outstanding achievements in the fields of medical or life sciences. It is the only prize of its kind to be awarded by a Japanese university. The 12th Keio Medical Science Prize will be awarded to Dr. Brian J. Druker and Dr. Hiroaki Mitsuya. Brian J. Druker, M.D. Investigator, Howard Hughes Medical Institute Director, Oregon Health & Science University Cancer Institute JELD-WEN Chair of Leukemia Research For the development of a molecular-targeted drug for chronic myelogenous leukemia Hiroaki Mitsuya, M.D., Ph.D. Professor, Department of Hematology, Department of Rheumatology and Clinical Immunology, Division of Infections Diseases, Graduate School of Medical and Pharmaceutical Sciences, Kumamoto University Chief and Principal Investigator, Experimental Retrovirology Section Center for Cancer Research National Cancer Institute For the development of anti-AIDS drugs Award Ceremony and Commemorative Symposium The award ceremony and a commemorative lecture given by the prize winners will be held on December 4, 2007 and a commemorative symposium will take place on December 5. Both events will be held at the Keio University School of Medicine (Shinanomachi Campus). Please see the contact information below to inquire about interviews or photographs. Attachments : (1) About the Keio University Medical Science Fund (2)2007 Prize Winner: Brian J. Druker(Theme, CV, other information) (3)2007 Prize Winner: Hiroaki Mitsuya(Theme, CV, other information) (4)2007 Keio Medical Science Prize Award Ceremony/Commemorative Lecture/ Commemorative Symposium Inquiries: Keio University Medical Science Fund(Ms. -

Precision Cancer Medicine: Achievements and Prospects
Precision Cancer Medicine: Achievements and Prospects John Mendelsohn, MD President Emeritus Tang Prize Award Ceremony September 22, 2018 Presented by Mien-Chie Hung, PhD Dr. John Mendelsohn with M.D. Anderson’s Hospital Education • Harvard College, Cambridge, MA, B.A., 1958, Biochemical Science • University of Glasgow, Glasgow, Scotland, Fulbright Scholar, 1959, Research in Molecular Biology • Harvard Medical School, M.D. 1963 Academic Administrative Appointments/Responsibilities •Founding Director of Cancer Center, University of California, San Diego, CA, 1976-85 •Chairman, Department of Medicine, Memorial Sloan- Kettering Cancer Center, New York, NY, 1985-96 •President, The University of Texas M. D. Anderson Cancer Center, Houston, TX, 1996- 2011 •Director, Sheikh Khalifa Bin Zayed Al Nahyan Institute for Personalized Cancer Therapy, The University of Texas M. D. Anderson Cancer Center, Houston, TX, 2011-18 Scientific Achievements • First hypothesis, with Dr. Gordon Sato, that inhibition of EGF receptors and of a tyrosine kinase might be an effective anticancer treatment. 1980 • First creation of an anti-EGF receptor/anti-tyrosine kinase agent that blocked receptor kinase activation and inhibited cell growth. 1983-84 • First clinical trial with an agent targeting a growth factor receptor and a tyrosine kinase, demonstrating safety and feasibility. 1990 • First studies demonstrating mechanisms by which inhibition of EGF receptor tyrosine kinase inhibits cell proliferation and other cellular functions. 1996 • First clinical trial providing proof of concept that an antireceptor agent (Herceptin) used alone could produce a clinically useful response rate (10%) in patients. 1996 • First clinical trial demonstrating that addition of an EGF receptor inhibitor could overcome resistance to a chemotherapeutic agent (cisplatin in head and neck cancer). -

The COVID-19 Issue a New Career Center Browse Jobs, Post Positions, Have Your Resume Critiqued and More
Vol.Vol. 19 19 / / No. No. 5 4 / / May April 2020 2020 THETHE MEMBERMEMBER MAGAZINEMAGAZINE OFOF THETHE AMERICANAMERICAN SOCIETYSOCIETY FORFOR BIOCHEMISTRYBIOCHEMISTRY ANDAND MOLECULARMOLECULAR BIOLOGYBIOLOGY The COVID-19 issue A new career center Browse jobs, post positions, have your resume critiqued and more. careers.asbmb.org NEWS FEATURES PERSPECTIVES 2 22 50 EDITOR’S NOTE A LEGACY OF TYROSINE ON THE FRONT LINE: Breaking the news PANDEMIC INSIGHT FROM 3 A HEALTH CARE WORKER MEMBER UPDATE COVID19 52 30 A small army of researchers 7 races to build a coronavirus QUARANTINED THOUGHTS IN MEMORIAM interactome 32 Could an old malaria drug 54 10 help fight SARS-COV02? JOURNAL NEWS A NEW CITY, A NEW JOB 10 Yeast as a detective’s assistabt 34 Anatomy of a molecule: what AND A GLOBAL PANDEMIC 12 Cow born in Japan after removal, makes remdesivir promising? replacement of placental cells 13 How is myelin made? 36 Slipping past the proofreader 16 Review delves into 59 44 Scientist uses community proximity proteomics IS MORE SCIENCE THE MEDICINE organizing skills to mobilize 17 From the journals WE NEED TO CURE THE WORLD’S researchers against COVID-19 STRUGGLING ECONOMY? 46 Researchers retool genomics labs to provide virus 2 testing 48 “We are doers. We want to get involved.” 12 22 13 54 MAY 2020 ASBMB TODAY 1 EDITOR’S NOTE THE MEMBER MAGAZINE OF THE AMERICAN SOCIETY FOR BIOCHEMISTRY AND MOLECULAR BIOLOGY Breaking the news OFFICERS COUNCIL MEMBERS By Comfort Dorn Gerald Hart Suzanne Barbour President Joan Broderick Toni M. Antalis Matt Gentry President-elect Blake Hill Audrey Lamb Wei Yang James M. -

Gleevec's Glory Days
Diabetes Detectives || $$$ to Databases || Anthrax 101 || Fighting Parasites in Bangladesh DECEMBER 2001 Gleevec’s Glory Days The Long Journey of a Celebrated Anticancer Drug FEATURES Gleevec’s Glory Days Mirpur’s Children 10 22 An apparent overnight success, this new A slum in Bangladesh yields clues about leukemia drug has decades of research behind it. immunity, infection and an illness that afflicts By Jill Waalen millions worldwide. By David Jarmul 16 Confronting Diabetes From All Angles 26 Scientific Outliers To combat this growing epidemic, researchers are hunting for genes, exploring cell-signaling How teachers and students in rural America pathways and looking at obesityÕs role. can learn good science. By Karen Hopkin By Mitch Leslie 16 In Starr County, Texas, an alarming 2,500 Mexican- American residents have type 2 diabetes. These women, at the Starr County Health Studies Office, undergo regular monitoring of their disease, which has strong genetic and evironmental components. DEPARTMENTS 2 NOTA BENE 30 HANDS ON Howard Hughes Medical Institute Bulletin ulletin Building Interest in the December 2001 || Volume 14 Number 5 3 PRESIDENT’S LETTER Human Body HHMI TRUSTEES Biomedical Research in a James A. Baker, III, Esq. Changed World Senior Partner, Baker & Botts NEWS AND NOTES Alexander G. Bearn, M.D. Executive Officer, American Philosophical Society 32 To Think Like a Scientist Adjunct Professor, The Rockefeller University UP FRONT Professor Emeritus of Medicine, Cornell University Medical College Frank William Gay 4 Mouse Model Closely 33 Undergraduate Taps Into Former President and Chief Executive Officer, summa Corporation James H. Gilliam, Jr., Esq. Mimics Human Cancer Tomato Communication Former Executive Vice President and General Counsel, Beneficial Corporation 6 Database Science Forcing New Hanna H. -

Weill Medical College of Cornell University Required Format For
CHARLES L. SAWYERS, MD Address: Phone: Fax: Email: EDUCATIONAL BACKGROUND Degree Institution name and location Dates attended Year awarded B.A. Princeton University, Princeton, NJ 1977–1981 1981 M.D. Johns Hopkins, Baltimore, MD 1981–1985 1985 PROFESSIONAL POSITIONS AND EMPLOYMENT Post-doctoral training (residency/fellowships) Title Institution name and location Dates held Internship & University of California, San Francisco 1985 – 1988 Residency Dept. of Medicine, San Francisco, CA Fellow University of California, Los Angeles 1988 – 1991 Division of Hematology-Oncology, Department of Medicine, Los Angeles, CA Post-doctoral UCLA/Howard Hughes Medical Institute 1989 – 1993 training Dr. Owen N. Witte, Professor of Microbiology & Molecular Genetics Los Angeles, CA Academic positions (teaching and research) Title Institution name and location Dates held Clinical University of California, Los Angeles 1991 – 1993 Instructor Division of Hematology-Oncology, Department of Medicine Assistant University of California, Los Angeles 1993 – 1997 Professor Division of Hematology-Oncology, Department of Medicine 1 Member University of California, Los Angeles 1993 – 2006 Jonsson Comprehensive Cancer Center Full Member University of California, Los Angeles 1993 – 2006 Molecular Biology Institute Associate University of California, Los Angeles 1996 – 2006 Chief Basic Research, Division of Hematology- Oncology, Department of Medicine Associate University of California, Los Angeles 1997 – 2000 Professor Division of Hematology-Oncology Department of Medicine -

2009 Annual Report
2009 ANNUAL REPORT CURE LEUKEMIA, LympHOMA, H ODGKIN’ S D I S EA S E A N D my ELO M A , A N D I mp R O V E T H E Q U A L I T Y O F L I F E O F PATIENTS AND THEIR FAMILIES. MISSION PRESIDENT & CHAIRMAN’S MESSAGE n looking back on The Leukemia & Lymphoma Society’s (LLS) 60 years, there is one defining characteristic that shows up in everything we do: Innovation. It is evident in every area of our mission, from our research track record, through innovative patient services programs and in new legislative victories that address the needs of the blood cancer population. This year’s report will highlight some of the innovations that have helped patients with blood cancers live better, longer lives and show some of the survivors who have benefited from LLS innovations. More than anything else, this 60th anniversary is a time when we are looking forward. The landscape in which we live and work is going through powerful changes and we grasp the need to adapt quickly, moving toward a culture that supports and nurtures fresh perspectives and solutions at every level of our organization, from the local chapter to the national board room. We have created a legacy of innovation. Now, it’s time to re-commit, with new vigor and resolve, as we remember the words of the German poet and intellectual, Goethe: “Whatever you can do or dream you can, begin it. Boldness has a genius, power and magic in it.” John E. -

Future of Genomic Medicine March 2 - 3, 2017 X Scripps Institution of Oceanography X La Jolla, CA
10th Annual Future of Genomic Medicine March 2 - 3, 2017 x Scripps Institution of Oceanography x La Jolla, CA Presented in partnership with Course Introduction Course Overview Course Highlights In collaboration with AAAS/Science Translational Medicine we • Voice of the patient represented throughout invite you to another exciting two day program on Thursday, the conference March 2 and Friday, March 3, 2017 in beautiful San Diego, • Renowned faculty representing the country’s California. The 2017 program will again be held at Scripps leading institutions Institution of Oceanography. • Multiple panel discussion segments with ample question and answer time with faculty The 10th annual Future of Genomic Medicine course will be the • Additional networking opportunities next iteration of taking genomic knowledge to transform the daily practice of medicine. To do this, we have patients present Educational Objectives their story of how genomics affected their medical status, and After attending this activity, participants should be able to: have a faculty of experts in genomics, science and medical • journalism, and the life science industry provide critical Demonstrate the unmet needs of medicine today with respect to more targeted, perspective. This year we will be paying particular attention to individualized prevention and treatments. the exciting area of genomic editing to treat particular diseases, • Discuss the opportunities of the genome, cancer (a disease of the genome), and the genomics of rare proteome, and metabolome discovery to and unknown diseases. Furthermore, we will delve into to the change medical practice as it exists today. hot topics of the microbiome, genomic-guided drug therapies • Assess how changes and advances in and genomic analytics. -
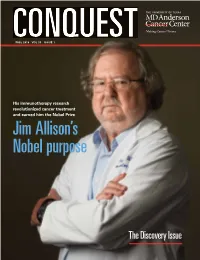
Conquest Fall 2018
CONQUESTFALL 2018 VOL 33 ISSUE 1 His immunotherapy research revolutionized cancer treatment and earned him the Nobel Prize Jim Allison’s Nobel purpose The Discovery Issue VOL 33 ISSUE 1 MISSION The mission of The University of Texas MD Anderson Cancer Center CONQUESTFALL 2018 VOL 33 ISSUE 1 is to eliminate cancer in Texas, the nation and the world through outstanding programs that integrate patient care, research and Photo: Nathan Lindstrom Nathan Photo: prevention, and through education for undergraduate and His immunotherapy research graduate students, trainees, professionals, employees and the public. revolutionized cancer treatment and earned him the Nobel Prize Jim Allison’s Nobel purpose VISION We shall be the premier cancer center in the world, based on the excellence of our people, our research-driven patient care and our science. The Discovery Issue We are Making Cancer History ®. ON THE COVER Jim Allison, Ph.D., is a blues-loving scientist CORE VALUES from the small town of Alice, Texas, who shook off immunotherapy naysayers and made believers out of everyone when he Caring figured out how to turn the immune system By our words and actions, we create a caring environment against tumors. for everyone. Integrity We work together to merit the trust of our colleagues and those we serve. Join our community MD Anderson Cancer Center Discovery We embrace creativity and seek new knowledge. @MDAndersonNews MDAnderson mdandersoncc MDAndersonCC +MDAnderson MDAndersonCancerCenter #endcancer VISIT THE CONQUEST WEBSITE AT WWW.MDANDERSON.ORG/CONQUEST CONTENTS FALL 2018 Photo: Adolfo Chavez III 8 4 THERAPEUTICS DISCOVERY sclerosis. One MD Anderson researcher is working This unique model for drug development allows to change that. -

How Someday Becomes Today
2015 ANNUAL REPORT how someday becomes today MICAYLA WYNN CHRONIC MYELOID LEUKEMIA SURVIVOR President and Every day brings more Chairman’s proof of The Leukemia & Message Lymphoma Society’s impact on the cancer treatment landscape, and our leadership was especially apparent in Fiscal Year 2015. New therapies for blood cancers are being Louis J. DeGennaro, PhD President & CEO discovered faster than ever before and those same treatments are also being tested for patients with other cancers like breast, colon and pancreatic cancer, and serious diseases like rheumatoid arthritis. And we continue to work diligently every day to ensure that all blood cancer patients have access to the James H. Davis, PhD, JD Chairman of the Board treatments they so desperately need. Thanks to you, The Leukemia & Lymphoma Society (LLS) is a driving force in making someday today for the more than 1.2 million people in the United States living with a blood cancer. From the strong science and advances in research you are helping us to spearhead, to wins in advocating for patients with legislators and policymakers, to helping newly diagnosed patients navigate their treatment, we continue to earn our leadership mantle as the voice for all blood cancer patients. Patients, caregivers and donors continually inspire us to keep investing in lifesaving breakthroughs. We raised awareness about blood cancers and the LLS mission through a wide array of media and communications channels in Fiscal Year 2015. You’ll see this, for example, in our support of the PBS documentary, “Ken Burns Presents Cancer: The Emperor of All Maladies,” which allowed LLS to showcase our historic role in advancing blood cancer treatments. -

OHSU Knight Cancer Institute Your 2017 Guide to Patient Referral
ONCOLOGY OHSU Knight Cancer Institute Your 2017 Guide to Patient Referral To refer a patient or consult with our team, please call 1 503-494-4567 or toll-free 800-245-6748. www.ohsuknightcancer.com 2DiagnosticTo radiologist, refer a patient Karen forOh, a M.D.,consult, consults call: with patient. 503-494-4567 or 800-245-6478 toll-free Message from department chair Dear Colleague, At the OHSU Knight Cancer Institute, collaboration is the source of many success stories. Through our partnership with you, we are proud to help provide the best possible oncology care for your patients. That, in turn, moves our communities forward. This referral guide is designed to help you easily connect with our adult oncology services. We’ve included a listing of our oncologists by subspecialty and multidisciplinary team, as well as a summary of multidisciplinary cancer clinics and oncology programs and services. To receive this book electronically, or a printed hard copy, go to www.ohsuknightcancer.com/referralguide. Please note the following, which will help you find answers quickly and serve your patients more effectively: Consult with any OHSU physician using one central phone number: 800-245-6478. Our Physician Consult & Referral Service is dedicated to connecting you to the right physician quickly and easily, 24 hours a day, with just one phone call. Fax referrals to 503-346-6854. View your patients’ OHSU medical records online through OHSU Connect. Our web-based provider portal allows you to follow the progress of your patients’ care at OHSU and improves coordination of ongoing care by providing: • Real-time access to their OHSU medical records (lab results, chart notes, medications and treatment plans). -

Every Day, Hhmi Supports the Pursuit of Knowledge and the Application Of
every day, HHMI supports the pursuit of knowledge and the application of that knowledge to benefit humanity.w e have structured the institute—physically, programmatically, philosophically—to empower the world’s finest scientists and educators. these individuals are also architects of discovery: shaping their laboratories and classrooms, guiding their teams, and conceiving the pioneering experiments that lead to innovations of lasting consequence. howard hughes medical institute 2010 annual report ARCHITECTS OF DISCOVERY from the presidenT Forty-nine years separated framework, which is taking processes that protect chromo- identification of the p“ hiladelphia literal form in the construction somal tips during replication.) chromosome” in patients with of a laboratory building to house more than bragging rights were at chronic myelogenous leukemia the KwaZulu-natal research stake in tackling such a complex from the 2009 lasker award institute for tuberculosis and structure: many antibiotics work ceremony honoring three scien- HIV (K-RITH) in durban, by shutting down bacterial ribo- tists for their work in developing south africa. our 10-year com- somes. new drugs are desperately drugs that target the protein pro- mitment to K-RITH recognizes needed, and novel antibiotics duced by the aberrant gene. the that solutions to human needs based on steitz’s discoveries are time span illustrates the complex- demand patience and time. now in development; two of the ity of transforming fundamental patience and urgency are twin newest have the potential to treat biological knowledge—acquired poles that define a scientist’s life, drug-resistant infections like in many labs over many years— as HHMI investigator Jim allison tuberculosis.