SEXUAL ASSAULT: an Acute Care Protocol for Medical/Forensic Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chain of Custody
BY KEITH G. CHVAL Chain of Custody Recent incidents have shown how important it is for colleges and universities to preserve evidence — including digital evidence — that may be required in a legal investigation. ey Jon, I need the “ chain of custody.” H “The what?” Your general counsel has just stopped by your office and dropped that bombshell on you as you were drinking your morning cup of coffee. “Remember all those e-mails and other electronic files you gave us in connection with that internal investigation of Smith last summer? Well, the case is going to trial, and we need the chain of custody to prove that Smith really wrote all those things. Without the chain of custody, the judge won’t admit any of that information, and we’ll get killed at trial.” While chain of custody is a legal is challenging the authenticity of If “chain of custody” is a new or term of art — meaning it has a evidence — particularly where digital vague concept to you, you’re not alone. specific meaning in the law and can evidence is involved — I’ve found that AEL HENDERSON AEL In simplest terms, a proper chain have legal consequences — it has there are very few who adequately L of custody establishes the integrity significant practical implications for account for the chain of custody, let of a piece of evidence, showing that IT managers and other professionals. alone appreciate its importance,” it wasn’t tampered with or otherwise “Although it plays a critical function observes Scott Carlson, a partner in altered since it was first collected. -
In-Town Business Listing - October 2020 This List Is Based on Informa�On Provided by the Public and Is Only Updated Periodically
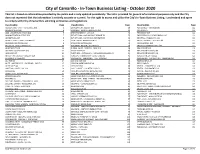
City of Camarillo - In-Town Business Listing - October 2020 This list is based on informaon provided by the public and is only updated periodically. The list is provided for general informaonal purposes only and the City does not represent that the informaon is enrely accurate or current. For the right to access and ulize the City's In-Town Business Lisng, I understand and agree to comply with City of Camarillo's soliciting ordinances and regulations. Classification Page Classification Page Classification Page ACCOUNTING - CPA - TAX SERVICE (93) 2 EMPLOYMENT AGENCY (10) 69 PET SERVICE - TRAINER (39) 112 ACUPUNCTURE (13) 4 ENGINEER - ENGINEERING SVCS (34) 70 PET STORE (7) 113 ADD- LOCATION/BUSINESS (64) 5 ENTERTAINMENT - LIVE (17) 71 PHARMACY (13) 114 ADMINISTRATION OFFICE (53) 7 ESTHETICIAN - HAS MASSAGE PERMIT (2) 72 PHOTOGRAPHY / VIDEOGRAPHY (10) 114 ADVERTISING (14) 8 ESTHETICIAN - NO MASSAGE PERMIT (35) 72 PRINTING - PUBLISHING (25) 114 AGRICULTURE - FARM - GROWER (5) 9 FILM - MOVIE PRODUCTION (2) 73 PRIVATE PATROL - SECURITY (4) 115 ALCOHOLIC BEVERAGE (16) 9 FINANCIAL SERVICES (44) 73 PROFESSIONAL (33) 115 ANTIQUES - COLLECTIBLES (18) 10 FIREARMS - REPAIR / NO SALES (2) 74 PROPERTY MANAGEMENT (39) 117 APARTMENTS (36) 10 FLORAL-SALES - DESIGNS - GRW (10) 74 REAL ESTATE (18) 118 APPAREL - ACCESSORIES (94) 12 FOOD STORE (43) 75 REAL ESTATE AGENT (180) 118 APPRAISER (7) 14 FORTUNES - ASTROLOGY - HYPNOSIS(NON-MED) (3) 76 REAL ESTATE BROKER (31) 124 ARTIST - ART DEALER - GALLERY (32) 15 FUNERAL - CREMATORY - CEMETERIES (2) 76 REAL ESTATE -
19-Cr-00008-NR Document 2581 Filed 12/21/20 Page 1 of 3
Case 2:19-cr-00008-NR Document 2581 Filed 12/21/20 Page 1 of 3 IN THE UNITED STATES DISTRICT COURT FOR THE WESTERN DISTRICT OF PENNSYLVANIA UNITED STATES OF AMERICA ) ) v. ) 2:19-cr-8-NR ) OMARI PATTON, ) ) ) Defendant. ) MEMORANDUM ORDER Omari Patton and 47 co-defendants are charged with engaging in a large-scale conspiracy to traffic a variety of Schedule I, II, and III controlled substances, including heroin, cocaine, fentanyl, and synthetic cannabinoids. Mr. Patton has requested leave to file a motion to suppress certain laboratory test results and other items that the Federal Bureau of Prisons seized, including card stock and other paper that was believed to have been soaked in controlled substances. ECF 1774; ECF 1810. After carefully considering the parties’ submissions, the Court will grant Mr. Patton leave to file his motion to suppress, but will deny the motion without prejudice to Mr. Patton reasserting his objections at or around the time of trial. Mr. Patton’s primary argument is that “the Government failed to properly preserve” the cards and paper seized and later lab tested because of “numerous and serious errors in the chain of custody.” ECF 1810, ¶¶ 4-6. Mr. Patton claims that “[p]hysical evidence must be authenticated before being admitted into evidence.” Id. at ¶ 7. He also claims that the substantial “break” in the chain of custody here makes this authentication impossible. Id. at ¶ 31. The government, however, correctly points out that “[a]uthentication objections, like other trial objections, are assessed according to the applicable Federal Rules of Evidence, including Rules 104(a) and 901(a),” and there is “no requirement that the proponent [of evidence] do so before the evidence is presented at trial[.]” ECF 1879, at ¶ 22. -

Chain of Custody Specimen Collection Instructions
DEPARTMENT OF PATHOLOGY AND LABORATORY MEDICINE CHAIN OF CUSTODY SPECIMEN COLLECTION INSTRUCTIONS Chain of custody specimens can be used as evidence in court as the specimen is collected in the presence of a witness, sealed to prevent tampering and all handling/possession of specimen is recorded on the form from collection to testing. Testing Available Drugs of Abuse Microbiology Drugs of Abuse Screen 5, CoC, Meconium, LAB7379 Chlamydia trachomatis and Neisseria gonorrhea PCR (CTNG PCR), Urine, LAB7166 Confirmed Drug Abuse Panel 9, CoC, Urine, LAB8020 Rapid Plasma Reagin w/ Reflex Titer (RPR), Blood, LAB7452 All Specimen Types 1. Place appropriate Chain of Custody test order in Epic 2. Microbiology samples can be ordered with or without Chain of Custody. Compete the following items in Epic when ordering testing for Chain of Custody: • Chain of Custody? Mark box “Yes” 3. Obtain Chain of Custody kit from the Laboratory: Anschutz Campus – 720-777-6711 North Campus – 720-478-5250 South Campus – 720-478-6711; 303-201-0155 (after-hours pager) Receive Chain of Custody Kit. Ensure all required items are included. Meconium Kit: Urine Kit: Blood Kit: • Chain of custody bag • Chain of custody bag • Chain of custody bag • Stool specimen container • Plastic cup • Red top vacutainer tube • Security label • 60-mL bottle • Security label • Chain of custody form • Security tape • Chain of custody form • Temperature slip • Chain of custody form 4. Complete Chain of Custody Form 5. Identify witness and obtain witness signature 6. Collect specimen: Meconium: Urine: Blood: • Place 1.0 to 5.0 • Collect specimen in provided cup or pediatric bag • Venipuncture or grams meconium in • Pour specimen into 60-mL transport bottle. -

Case: 4:11-Cv-00454-DCN Doc #: 40 Filed: 03/28/14 1 of 46. Pageid
Case: 4:11-cv-00454-DCN Doc #: 40 Filed: 03/28/14 1 of 46. PageID #: <pageID> UNITED STATES DISTRICT COURT NORTHERN DISTRICT OF OHIO EASTERN DIVISION JOHN E. WOLFF, JR., ) CASE NO. 4:11-cv-0454 ) Petitioner, ) JUDGE NUGENT ) v. ) MAGISTRATE JUDGE VECCHIARELLI ) TERRY TIBBALS, ) ) REPORT AND RECOMMENDATION Respondent. ) This matter is before the magistrate judge pursuant to Local Rule 72.2(b)(2). Before the court is the petition of John E. Wolff, Jr., (“Petitioner”) for a writ of habeas corpus filed pursuant to 28 U.S.C. § 2254. Petitioner is in the custody of the Ohio Department of Rehabilitation and Correction pursuant to journal entry of sentence in the case of State of Ohio vs. Wolff, Case No. 06-CR-978 (Mahoning County Aug. 29, 2007). (Doc. No. 23-10.) For the reasons set forth below, it is recommended that the petition be dismissed with prejudice. I. Relevant Factual Background The state appellate court that reviewed Petitioner’s conviction and sentence recited the following facts: On September 14, 2006, Wolff was indicted on ten counts of rape, in violation of R.C. 2907.02(A)(1)(b)(B), special felony (Counts 1-10); three counts of rape, in violation of R.C. 2907.02(A)(2)(B), 1st degree felony (Counts 11-13); five counts of gross sexual imposition, in violation of R.C. 2907.05(A)(4)(B), 3rd degree felony (Counts 14-18); and two counts of gross sexual imposition, in violation of R.C. Case: 4:11-cv-00454-DCN Doc #: 40 Filed: 03/28/14 2 of 46. -

Ray Bradbury Creative Contest Literary Journal
32nd Annual Ray Bradbury Creative Contest Literary Journal 2016 Val Mayerik Val Ray Bradbury Creative Contest A contest of writing and art by the Waukegan Public Library. This year’s literary journal is edited, designed, and produced by the Waukegan Public Library. Table of Contents Elementary School Written page 1 Middle School Written page 23 High School Written page 52 Adult Written page 98 Jennifer Herrick – Designer Rose Courtney – Staff Judge Diana Wence – Staff Judge Isaac Salgado – Staff Judge Yareli Facundo – Staff Judge Elementary School Written The Haunted School Alexis J. In one wonderful day there was a school-named “Hyde Park”. One day when, a kid named Logan and his friend Mindy went to school they saw something new. Hyde Park is hotel now! Logan and Mindy Went inside to see what was going on. So they could not believe what they say. “Hyde Park is also now haunted! When Logan took one step they saw Slender Man. Then they both walk and there was a scary mask. Then mummies started coming out of the grown and zombies started coming from the grown and they were so stinky yuck! Ghost came out all over the school and all the doors were locked. Now Mindy had a plan to scare all the monsters away. She said “we should put all the monsters we saw all together. So they make Hyde Park normal again. And they live happy ever after and now it is back as normal. THE END The Haunted House Angel A. One day it was night. And it was so dark a lot of people went on a house called “dead”. -
Gene Expression Profile in Different Age Groups and Its Association With
cells Article Gene Expression Profile in Different Age Groups and Its Association with Cognitive Function in Healthy Malay Adults in Malaysia Nur Fathiah Abdul Sani 1 , Ahmad Imran Zaydi Amir Hamzah 1, Zulzikry Hafiz Abu Bakar 1 , Yasmin Anum Mohd Yusof 2, Suzana Makpol 1 , Wan Zurinah Wan Ngah 1 and Hanafi Ahmad Damanhuri 1,* 1 Department of Biochemistry, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Center, Jalan Yaacob Latif, Cheras, Kuala Lumpur 56000, Malaysia; [email protected] (N.F.A.S.); [email protected] (A.I.Z.A.H.); zulzikryhafi[email protected] (Z.H.A.B.); [email protected] (S.M.); [email protected] (W.Z.W.N.) 2 Faculty of Medicine and Defence Health, National Defence University of Malaysia, Kem Sungai Besi, Kuala Lumpur 57000, Malaysia; [email protected] * Correspondence: hanafi[email protected] Abstract: The mechanism of cognitive aging at the molecular level is complex and not well under- stood. Growing evidence suggests that cognitive differences might also be caused by ethnicity. Thus, this study aims to determine the gene expression changes associated with age-related cognitive decline among Malay adults in Malaysia. A cross-sectional study was conducted on 160 healthy Malay subjects, aged between 28 and 79, and recruited around Selangor and Klang Valley, Malaysia. Citation: Abdul Sani, N.F.; Amir Gene expression analysis was performed using a HumanHT-12v4.0 Expression BeadChip microarray Hamzah, A.I.Z.; Abu Bakar, Z.H.; kit. The top 20 differentially expressed genes at p < 0.05 and fold change (FC) = 1.2 showed that Mohd Yusof, Y.A.; Makpol, S.; Wan PAFAH1B3, HIST1H1E, KCNA3, TM7SF2, RGS1, and TGFBRAP1 were regulated with increased Ngah, W.Z.; Damanhuri, H.A. -

GUIDE to NEW YORK EVIDENCE ARTICLE 11 REAL and DEMONSTRATIVE EVIDENCE TABLE of CONTENTS 11.01 Real Evidence 11.03 Demonstrative
GUIDE TO NEW YORK EVIDENCE ARTICLE 11 REAL AND DEMONSTRATIVE EVIDENCE TABLE OF CONTENTS 11.01 Real Evidence 11.03 Demonstrative Evidence 11.05 Anatomically Correct Dolls 11.07 Childs Age 11.09 Demonstrations and Experiments 11.11 Personal Appearance & Capability 11.13 Photographs 11.15 Viewing of Premises 11.17 Exhibits to the Jury 11.01. Real Evidence (1) Definition. Real Evidence refers to any tangible object or sound recording of a conversation that is offered in evidence. (2) Admissibility. Real evidence is admissible upon a showing that it is relevant to an issue in the proceeding, is what it purports to be, and has not been tampered with. Proof that an object has not been tampered with and is what it purports to be depends on the nature of the object and, in particular, whether the object is patently identifiable, or fungible. (a) Patently identifiable evidence. When real evidence possesses unique or distinctive characteristics or markings and is not subject to material alteration that is not readily apparent, evidence identifying the object normally will constitute the requisite proof. (b) Fungible evidence. When real evidence is fungible, capable of being altered, contaminated, or replaced, or is a sound recording, in addition to testimony identifying the object, proof that the proffered evidence has not been tampered with is required and may be satisfied by: (i) a chain of custody (i.e. testimony of those persons who handled the object or recording from the time it was obtained or recorded to the time it is presented in court to identify the object or recording and attest to its unchanged condition); or (ii) proof of circumstances that provide reasonable assurances of the identity and unchanged condition of the object or recording. -

WHO Background Paper Obstacles to Women Accessing Forensic Medical Exams in Cases of Sexual Violence by A. Widney Brown, Advocac
WHO Background Paper Obstacles to Women Accessing Forensic Medical Exams in Cases of Sexual Violence By A. Widney Brown, Advocacy Director, Women’s Rights Division, Human Rights Watch Final Version Introduction The international community awoke to the realization that “women’s rights are human rights” when women’s rights activists from all over the world took center stage at the World Conference on Human Rights held in Vienna in 1993. They seized the initiative at the conference by focusing on violence against women and the failure of states to provide redress for the violence suffered. At a tribunal held at the NGO parallel conference, women from numerous countries stepped forward to describe their experiences as victims of sexual and gender based violence. They also described the failure of the state to condemn the violence, to protect women from further violence and to provide redress through the criminal justice system. The pervasiveness of violence against women is breathtaking in developing and developed countries alike.1 The litany of harms inflicted is long: female genital mutilation, forced marriages, trafficking into forced labor, domestic violence, so-called honor killings, acid burning, dowry deaths, and finally, in every culture, rape and other crimes of sexual violence. The U.N. Convention on the Elimination of all forms of Discrimination against Women adopted in 1979, called on States to “take in all fields appropriate measures, including legislation, to ensure the full development and advancement of women, for the purpose -

Thesis, the Songs of 10 Rappers Were Analyzed
ABSTRACT Get Rich or Die Tryin’: A Semiotic Approach to the Construct of Wealth in Rap Music Kristine Ann Davis, M.A. Mentor: Sara J. Stone, Ph.D. For the past 30 years, rap music has made its way into the mainstream of America, taking an increasingly prominent place in popular culture, particularly for youth, its main consumers. This thesis looks at wealth through the lens of semiotics, an important component of critical/cultural theory, using a hermeneutical analysis of 11 rap songs, spanning the last decade of rap music to find signification and representation of wealth in the rap song lyrics. The research finds three important themes of wealth - relationship between wealth and the opposite sex, wealth that garners respect from other people, and wealth as a signifier for “living the good life” - and five signifiers of wealth – money, cars, attire, liquor, and bling. Get Rich or Die Tryin': A Semiotic Approach to the Construct of Wealth in Rap Music by Kristine Ann Davis, B.A. A Thesis Approved by the Department of Journalism ___________________________________ Clark Baker, Ph.D., Chairperson Submitted to the Graduate Faculty of Baylor University in Partial Fulfillment of the Requirements for the Degree of Master of Arts Approved by the Thesis Committee ___________________________________ Sara J. Stone, Ph.D., Chairperson ___________________________________ Mia Moody-Ramirez, Ph.D. ___________________________________ Tony L.Talbert, Ed.D. Accepted by the Graduate School August 2011 ___________________________________ J. Larry Lyon, Ph.D., Dean Page bearing signatures is kept on file in the Graduate School. Copyright ! 2011 by Kristine Ann Davis All rights reserved! CONTENTS ACKNOWLEDGMENTS v Chapter 1. -
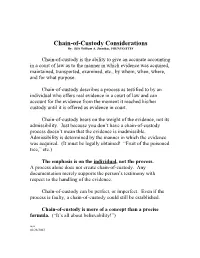
Chain-Of-Custody Considerations By: SSA William A
Chain-of-Custody Considerations By: SSA William A. Zinnikas, FBI/NYO/JTTF Chain-of-custody is the ability to give an accurate accounting in a court of law as to the manner in which evidence was acquired, maintained, transported, examined, etc., by whom, when, where, and for what purpose. Chain-of-custody describes a process as testified to by an individual who offers real evidence in a court of law and can account for the evidence from the moment it reached his/her custody until it is offered as evidence in court. Chain-of-custody bears on the weight of the evidence, not its admissibility. Just because you don’t have a chain-of-custody process doesn’t mean that the evidence is inadmissible. Admissibility is determined by the manner in which the evidence was acquired. (It must be legally obtained! “Fruit of the poisoned tree,” etc.) The emphasis is on the individual, not the process. A process alone does not create chain-of-custody. Any documentation merely supports the person’s testimony with respect to the handling of the evidence. Chain-of-custody can be perfect, or imperfect. Even if the process is faulty, a chain-of-custody could still be established. Chain-of-custody is more of a concept than a precise formula. (“It’s all about believability!”) waz 02/26/2003 Technically, chain-of-custody only applies to sworn law enforcement officers. However, if a laboratory is assisting law enforcement in an investigation, the laboratory could be construed by the court as an “agent” of law enforcement. -

Hip-Hop and Cultural Interactions: South Korean and Western Interpretations
HIP-HOP AND CULTURAL INTERACTIONS: SOUTH KOREAN AND WESTERN INTERPRETATIONS. by Danni Aileen Lopez-Rogina, B.A. A thesis submitted to the Graduate Council of Texas State University in partial fulfillment of the requirements for the degree of Master of Arts with a Major in Sociology May 2017 Committee Members: Nathan Pino, Chair Rachel Romero Rafael Travis COPYRIGHT by Danni Aileen Lopez-Rogina 2017 FAIR USE AND AUTHOR’S PERMISSION STATEMENT Fair Use This work is protected by the Copyright Laws of the United States (Public Law 94-553, section 107). Consistent with fair use as defined in the Copyright Laws, brief quotations from this material are allowed with proper acknowledgement. Use of this material for financial gain without the author’s express written permission is not allowed. Duplication Permission As the copyright holder of this work I, Danni Aileen Lopez-Rogina, refuse permission to copy in excess of the “Fair Use” exemption without my written permission. DEDICATION To Frankie and Holly for making me feel close to normal. ACKNOWLEDGEMENTS I want to acknowledge my mom, dad, and sister first and foremost. Without their love and support over the years, I would not have made it this far. They are forever my cheerleaders, no matter how sassy I may be. Professor Nathan Pino was my chosen mentor who took me under his wing when I chose him like a stray cat. His humor and dedication to supporting me helped me keep my head up even when I felt like I was drowning. Professor Rachel Romero was the one to inspire me to not only study sociology, but also to explore popular culture as a key component of society.