Human Granulocytic Anaplasmosis - in This Issue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Official Nh Dhhs Health Alert
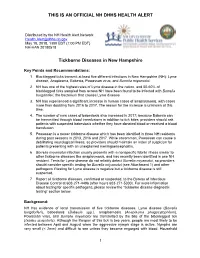
THIS IS AN OFFICIAL NH DHHS HEALTH ALERT Distributed by the NH Health Alert Network [email protected] May 18, 2018, 1300 EDT (1:00 PM EDT) NH-HAN 20180518 Tickborne Diseases in New Hampshire Key Points and Recommendations: 1. Blacklegged ticks transmit at least five different infections in New Hampshire (NH): Lyme disease, Anaplasma, Babesia, Powassan virus, and Borrelia miyamotoi. 2. NH has one of the highest rates of Lyme disease in the nation, and 50-60% of blacklegged ticks sampled from across NH have been found to be infected with Borrelia burgdorferi, the bacterium that causes Lyme disease. 3. NH has experienced a significant increase in human cases of anaplasmosis, with cases more than doubling from 2016 to 2017. The reason for the increase is unknown at this time. 4. The number of new cases of babesiosis also increased in 2017; because Babesia can be transmitted through blood transfusions in addition to tick bites, providers should ask patients with suspected babesiosis whether they have donated blood or received a blood transfusion. 5. Powassan is a newer tickborne disease which has been identified in three NH residents during past seasons in 2013, 2016 and 2017. While uncommon, Powassan can cause a debilitating neurological illness, so providers should maintain an index of suspicion for patients presenting with an unexplained meningoencephalitis. 6. Borrelia miyamotoi infection usually presents with a nonspecific febrile illness similar to other tickborne diseases like anaplasmosis, and has recently been identified in one NH resident. Tests for Lyme disease do not reliably detect Borrelia miyamotoi, so providers should consider specific testing for Borrelia miyamotoi (see Attachment 1) and other pathogens if testing for Lyme disease is negative but a tickborne disease is still suspected. -

Anaplasma Species of Veterinary Importance in Japan
Veterinary World, EISSN: 2231-0916 REVIEW ARTICLE Available at www.veterinaryworld.org/Vol.9/November-2016/4.pdf Open Access Anaplasma species of veterinary importance in Japan Adrian Patalinghug Ybañez1 and Hisashi Inokuma2 1. Biology and Environmental Studies Program, Sciences Cluster, University of the Philippines Cebu, Lahug, Cebu City 6000, Philippines; 2. Department of Veterinary Clinical Science, Obihiro University of Agriculture and Veterinary Medicine, Obihiro, Inada Cho, Hokkaido 080-8555, Japan. Corresponding author: Adrian Patalinghug Ybañez, e-mail: [email protected], HI: [email protected] Received: 14-06-2016, Accepted: 28-09-2016, Published online: 04-11-2016 doi: 10.14202/vetworld.2016.1190-1196 How to cite this article: Ybañez AP, Inokuma H (2016) Anaplasma species of veterinary importance in Japan, Veterinary World, 9(11): 1190-1196. Abstract Anaplasma species of the family Anaplasmataceae, order Rickettsiales are tick-borne organisms that can cause disease in animals and humans. In Japan, all recognized species of Anaplasma (except for Anaplasma ovis) and a potentially novel Anaplasma sp. closely related to Anaplasma phagocytophilum have been reported. Most of these detected tick- borne pathogens are believed to be lowly pathogenic in animals in Japan although the zoonotic A. phagocytophilum has recently been reported to cause clinical signs in a dog and in humans. This review documents the studies and reports about Anaplasma spp. in Japan. Keywords: Anaplasma spp., Japan, tick-borne pathogen. Introduction A. phagocytophilum sequences [10-15]. Phylogenetic Anaplasma species are Gram-negative, obligate inferences have suggested that 2 clades exist within intracellular bacteria of the order Rickettsiales, fam- the genus Anaplasma: (1) Erythrocytic (A. -

Habitat Associations of Ixodes Scapularis (Acari: Ixodidae) in Syracuse, New York
SUNY College of Environmental Science and Forestry Digital Commons @ ESF Honors Theses 5-2016 Habitat Associations of Ixodes Scapularis (Acari: Ixodidae) in Syracuse, New York Brigitte Wierzbicki Follow this and additional works at: https://digitalcommons.esf.edu/honors Part of the Entomology Commons Recommended Citation Wierzbicki, Brigitte, "Habitat Associations of Ixodes Scapularis (Acari: Ixodidae) in Syracuse, New York" (2016). Honors Theses. 106. https://digitalcommons.esf.edu/honors/106 This Thesis is brought to you for free and open access by Digital Commons @ ESF. It has been accepted for inclusion in Honors Theses by an authorized administrator of Digital Commons @ ESF. For more information, please contact [email protected], [email protected]. HABITAT ASSOCIATIONS OF IXODES SCAPULARIS (ACARI: IXODIDAE) IN SYRACUSE, NEW YORK By Brigitte Wierzbicki Candidate for Bachelor of Science Environmental and Forest Biology With Honors May,2016 APPROVED Thesis Project Advisor: Af ak Ck M issa K. Fierke, Ph.D. Second Reader: ~~ Nicholas Piedmonte, M.S. Honors Director: w44~~d. William M. Shields, Ph.D. Date: ~ / b / I & r I II © 2016 Copyright B. R. K. Wierzbicki All rights reserved. 111 ABSTRACT Habitat associations of Jxodes scapularis Say were described at six public use sites within Syracuse, New York. Adult, host-seeking blacklegged ticks were collected using tick flags in October and November, 2015 along two 264 m transects at each site, each within a distinct forest patch. We examined the association of basal area, leaf litter depth, and percent understory cover with tick abundance using negative binomial regression models. Models indicated tick abundance was negatively associated with percent understory cover, but was not associated with particular canopy or understory species. -

Ehrlichiosis
Ehrlichiosis What is ehrlichiosis and can also have a wide range of signs Who should I contact, if I what causes it? including loss of appetite, weight suspect ehrlichiosis? Ehrlichiosis (air-lick-ee-OH-sis) is a loss, prolonged fever, weakness, and In Animals – group of similar diseases caused by bleeding disorders. Contact your veterinarian. In Humans – several different bacteria that attack Can I get ehrlichiosis? the body’s white blood cells (cells Contact your physician. Yes. People can become infected involved in the immune system that with ehrlichiosis if they are bitten by How can I protect my animal help protect against disease). The an infected tick (vector). The disease organisms that cause ehrlichiosis are from ehrlichiosis? is not spread by direct contact with found throughout the world and are Ehrlichiosis is best prevented by infected animals. However, animals spread by infected ticks. Symptoms in controlling ticks. Inspect your pet can be carriers of ticks with the animals and humans can range from frequently for the presence of ticks bacteria and bring them into contact mild, flu-like illness (fever, body aches) and remove them promptly if found. with humans. Ehrlichiosis can also to severe, possibly fatal disease. Contact your veterinarian for effective be transmitted through blood tick control products to use on What animals get transfusions, but this is rare. your animal. ehrlichiosis? Disease in humans varies from How can I protect myself Many animals can be affected by mild infection to severe, possibly fatal ehrlichiosis, although the specific infection. Symptoms may include from ehrlichiosis? bacteria involved may vary with the flu-like signs (chills, body aches and The risk for infection is decreased animal species. -

And Toxoplasmosis in Jackass Penguins in South Africa
IMMUNOLOGICAL SURVEY OF BABESIOSIS (BABESIA PEIRCEI) AND TOXOPLASMOSIS IN JACKASS PENGUINS IN SOUTH AFRICA GRACZYK T.K.', B1~OSSY J.].", SA DERS M.L. ', D UBEY J.P.···, PLOS A .. ••• & STOSKOPF M. K .. •••• Sununary : ReSlIlIle: E x-I1V\c n oN l~ lIrIUSATION D'Ar\'"TIGENE DE B ;IB£,'lA PH/Re El EN ELISA ET simoNi,cATIVlTli t'OUR 7 bxo l'l.ASMA GONIJfI DE SI'I-IENICUS was extracted from nucleated erythrocytes Babesia peircei of IJEMIiNSUS EN ArRIQUE D U SUD naturally infected Jackass penguin (Spheniscus demersus) from South Africo (SA). Babesia peircei glycoprotein·enriched fractions Babesia peircei a ele extra it d 'erythrocytes nue/fies p,ovenanl de Sphenicus demersus originoires d 'Afrique du Sud infectes were obto ined by conca navalin A-Sepharose affinity column natulellement. Des fractions de Babesia peircei enrichies en chromatogrophy and separated by sod ium dodecyl sulphate glycoproleines onl ele oblenues par chromatographie sur colonne polyacrylam ide gel electrophoresis (SDS-PAGE ). At least d 'alfinite concona valine A-Sephorose et separees par 14 protein bonds (9, 11, 13, 20, 22, 23, 24, 43, 62, 90, electrophorese en gel de polyacrylamide-dodecylsuJfale de sodium 120, 204, and 205 kDa) were observed, with the major protein (SOS'PAGE) Q uotorze bandes proleiques au minimum ont ete at 25 kDa. Blood samples of 191 adult S. demersus were tes ted observees (9, 1 I, 13, 20, 22, 23, 24, 43, 62, 90, 120, 204, by enzyme-linked immunosorbent assoy (ELISA) utilizing B. peircei et 205 Wa), 10 proleine ma;eure elant de 25 Wo. -

Tick Borne Diseases Nebraska 2018 HAN FINAL DRAFT APRIL 19 2018
TO: Primary care providers, infectious disease, laboratories, infection control, and public health FROM Thomas J. Safranek, M.D. Jeff Hamik State Epidemiologist Vector-borne Disease Epidemiologist 402-471-2937 PHONE 402-471-1374 PHONE 402-471-3601 FAX 402-471-3601 FAX Thomas Williams, M.D. Chief Medical Officer Director, Division of Public Health Department of Health and Human Services RE: TICK-BORNE DISEASES IN NEBRASKA DATE: April 20, 2018 The arrival of spring marks the beginning of another tick season. In the interest of public health and prevention, our office seeks to inform Nebraska health care providers about the known tick- borne diseases in our state. Key messages for Nebraska clinicians: Spotted fever rickettsia including Rocky Mountain spotted fever (RMSF) Our office receives reports of from 6 to 31 patients with spotted fever rickettsia every year. Health care providers risk overlooking this diagnosis because of its rarity. RMSF NEEDS TO BE A DIAGNOSTIC CONSIDERATION IN ANY PERSON WITH A FEVER AND A HISTORY OF EXPOSURE TO ENVIRONMENTS WHERE TICKS MIGHT BE PRESENT. The skin rash is not always present when the patient first presents to a physician. This disease is frequently overlooked or misdiagnosed, with numerous reports of serious and sometimes fatal consequences. Nebraska experienced a fatal case of RMSF in 2015 where the diagnosis was missed and treatment was delayed until the disease was well advanced. Laboratory diagnosis is made by detecting a rise in antibody titer to Rickettsia rickettsii between acute and convalescent sera. Treatment requires tetracycline-class of antibiotics or chloramphenicol. Tetracycline-class treatment is recommended for persons of all ages, including children. -
Bitten Enhance.Pdf
bitten. Copyright © 2019 by Kris Newby. All rights reserved. Printed in the United States of America. No part of this book may be used or reproduced in any manner whatsoever without written permission except in the case of brief quotations embodied in critical articles and reviews. For information, address HarperCollins Publishers, 195 Broadway, New York, NY 10007. HarperCollins books may be purchased for educational, business, or sales pro- motional use. For information, please email the Special Markets Department at [email protected]. first edition Frontispiece: Tick research at Rocky Mountain Laboratories, in Hamilton, Mon- tana (Courtesy of Gary Hettrick, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases [NIAID], National Institutes of Health [NIH]) Maps by Nick Springer, Springer Cartographics Designed by William Ruoto Library of Congress Cataloging- in- Publication Data Names: Newby, Kris, author. Title: Bitten: the secret history of lyme disease and biological weapons / Kris Newby. Description: New York, NY: Harper Wave, [2019] Identifiers: LCCN 2019006357 | ISBN 9780062896278 (hardback) Subjects: LCSH: Lyme disease— History. | Lyme disease— Diagnosis. | Lyme Disease— Treatment. | BISAC: HEALTH & FITNESS / Diseases / Nervous System (incl. Brain). | MEDICAL / Diseases. | MEDICAL / Infectious Diseases. Classification: LCC RC155.5.N49 2019 | DDC 616.9/246—dc23 LC record available at https://lccn.loc.gov/2019006357 19 20 21 22 23 lsc 10 9 8 7 6 5 4 3 2 1 Appendix I: Ticks and Human Disease Agents -

Dengue in Florida (USA)
Insects 2014, 5, 991-1000; doi:10.3390/insects5040991 OPEN ACCESS insects ISSN 2075-4450 www.mdpi.com/journal/insects/ Article Dengue in Florida (USA) Jorge R. Rey Florida Medical Entomology Laboratory, University of Florida-IFAS, 200 9th Street S.E., Vero Beach, FL 32962, USA; E-Mail: [email protected]; Tel.: +1-772-778-7200 (ext. 136); Fax +1-772-7787205 External Editor: C. Roxanne Connelly Received: 30 October 2014; in revised form: 4 December 2014 / Accepted: 9 December 2014 / Published: 16 December 2014 Abstract: Florida (USA), particularly the southern portion of the State, is in a precarious situation concerning arboviral diseases. The geographic location, climate, lifestyle, and the volume of travel and commerce are all conducive to arbovirus transmission. During the last decades, imported dengue cases have been regularly recorded in Florida, and the recent re-emergence of dengue as a major public health concern in the Americas has been accompanied by a steady increase in the number of imported cases. In 2009, there were 28 cases of locally transmitted dengue in Key West, and in 2010, 65 cases were reported. Local transmission was also reported in Martin County in 2013 (29 cases), and isolated locally transmitted cases were also reported from other counties in the last five years. Dengue control and prevention in the future will require close cooperation between mosquito control and public health agencies, citizens, community and government agencies, and medical professionals to reduce populations of the vectors and to condition citizens and visitors to take personal protection measures that minimize bites by infected mosquitoes. -

The Emergence of Epidemic Dengue Fever and Dengue Hemorrhagic
Editorial The emergence of A global pandemic of dengue fever (DF) and dengue hemorrhagic fever (DHF) began in Southeast Asia during World War II and in the years following that con- epidemic dengue flict (1). In the last 25 years of the 20th century the pandemic intensified, with increased geographic spread of both the viruses and the principal mosquito vec- fever and dengue tor, Aedes aegypti. This led to larger and more frequent epidemics and to the emergence of DHF as tropical countries and regions became hyperendemic with hemorrhagic fever the co-circulation of multiple virus serotypes. With the exception of sporadic epidemics in the Caribbean islands, in the Americas: dengue and yellow fever were effectively controlled in the Americas from 1946 a case of failed until the late 1970s as a result of the Ae. aegypti eradication program conducted by the Pan American Health Organization (PAHO) (1, 2). This was a vertically struc- public health policy tured, paramilitary program that focused on mosquito larval control using source reduction and use of insecticides, primarily dichlorodiphenyltrichloroethane (DDT). This highly successful program, however, was disbanded in the early 1970s because there was no longer a perceived need and there were competing 1 Duane Gubler priorities for resources; control of dengue and yellow fever was thereafter merged with malaria control. Another major policy change at that time was the use of ultra-low-volume space sprays for killing adult mosquitoes (adulticides) as the rec- ommended method to control Ae. aegypti and thus prevent and control DF and DHF. Both of these decisions were major policy failures because they were inef- fective in preventing the re-emergence of epidemic DF and the emergence of DHF in the Region. -

Zoonotic Significance and Prophylactic Measure Against Babesiosis
Int.J.Curr.Microbiol.App.Sci (2015) 4(7): 938-953 International Journal of Current Microbiology and Applied Sciences ISSN: 2319-7706 Volume 4 Number 7 (2015) pp. 938-953 http://www.ijcmas.com Review Article Zoonotic significance and Prophylactic Measure against babesiosis Faryal Saad, Kalimullah Khan, Shandana Ali and Noor ul Akbar* Department of Zoology, Kohat University of Science and Technology, Kohat, Khyber Pakhtunkhwa, Pakistan *Corresponding author ABSTRACT Babesiosis is a vector borne disease by the different species of genus Babesia, affecting a large no of mammals worldwide. Babesiosis has zoonotic significance all over the world, causing huge loss to livestock industry and health hazards in human population. The primary zoonotic vector of babesia is ixodes ticks. Keywo rd s Different species have different virulence, infectivity and pathogenicity. Literature was collected from the individual researchers published papers. Table was made in Babesiosis , the MS excel. The present study review for the current knowledge about the Prophylactic, babesia species ecology, host specificity, life cycle and pathogenesis with an Tick borne, emphasis on the zoonotic significance and prophylactic measures against Vector, Babesiosis. Prophylactic measure against Babesiosis in early times was hindered Zoonosis. but due to advancement in research, the anti babesial drugs and vaccines have been developed. This review emphasizes on the awareness of public sector, rural communities, owners of animal husbandry and health department about the risk of infection in KPK and control measure should be implemented. Vaccines of less price tag should be designed to prevent the infection of cattles and human population. Introduction Babesiosis is a tick transmitted disease, At specie level there is considerable infecting a wide variety of wild and confusion about the true number of zoonotic domestic animals, as well as humans. -

Expert Meeting on Chikungunya Modelling
MEETING REPORT Expert meeting on chikungunya modelling Stockholm, April 2008 www.ecdc.europa.eu ECDC MEETING REPORT Expert meeting on chikungunya modelling Stockholm, April 2008 Stockholm, March 2009 © European Centre for Disease Prevention and Control, 2009 Reproduction is authorised, provided the source is acknowledged, subject to the following reservations: Figures 9 and 10 reproduced with the kind permission of the Journal of Medical Entomology, Entomological Society of America, 10001 Derekwood Lane, Suite 100, Lanham, MD 20706-4876, USA. MEETING REPORT Expert meeting on chikungunya modelling Table of contents Content...........................................................................................................................................................iii Summary: Research needs and data access ...................................................................................................... 1 Introduction .................................................................................................................................................... 2 Background..................................................................................................................................................... 3 Meeting objectives ........................................................................................................................................ 3 Presentations ................................................................................................................................................. -

Anaplasmosis: an Emerging Tick-Borne Disease of Importance in Canada
IDCases 14 (2018) xxx–xxx Contents lists available at ScienceDirect IDCases journal homepage: www.elsevier.com/locate/idcr Case report Anaplasmosis: An emerging tick-borne disease of importance in Canada a, b,c d,e e,f Kelsey Uminski *, Kamran Kadkhoda , Brett L. Houston , Alison Lopez , g,h i c c Lauren J. MacKenzie , Robbin Lindsay , Andrew Walkty , John Embil , d,e Ryan Zarychanski a Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, University of Manitoba, Winnipeg, MB, Canada b Cadham Provincial Laboratory, Government of Manitoba, Winnipeg, MB, Canada c Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Medical Microbiology and Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada d Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Medical Oncology and Hematology, University of Manitoba, Winnipeg, MB, Canada e CancerCare Manitoba, Department of Medical Oncology and Hematology, Winnipeg, MB, Canada f Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Pediatrics and Child Health, Section of Infectious Diseases, Winnipeg, MB, Canada g Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada h Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Community Health Sciences, University of Manitoba, Winnipeg, MB, Canada i Public Health Agency of Canada, National Microbiology Laboratory, Zoonotic Diseases and Special Pathogens, Winnipeg, MB, Canada A R T I C L E I N F O A B S T R A C T Article history: Human Granulocytic Anaplasmosis (HGA) is an infection caused by the intracellular bacterium Received 11 September 2018 Anaplasma phagocytophilum.