Psychology Internship Training Program 2022-2023
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The History and Philosophy of Health Psychology And
Revista Psicologia e Saúde. DOI: hƩ p://dx.doi.org/10.20435/pssa.v10i2.693 25 Mind the Gap: The History and Philosophy of Health Psychology and Mindfulness Atenção aos Detalhes: A História e Filosofi a da Psicologia da Saúde e Mindfulness Ojo a los Detalles: Historia y Filosoİ a de la Psicología de la Salud y Mindfulness Shayna Fox Lee1 York University, Canada Jacy L. Young Abstract The recent surge in popularity of the concept ‘mindfulness’ in academic, professional, and popular psychology has been remarkable. The ease with which mindfulness has gained trac on in the health sciences and cultural imagina on makes it apparent mindfulness is well-suited to our current social climate, appealing to both, experts and laypeople. As a subdiscipline established rela vely late in the twen eth century, health psychology has a unique rela onship to mindfulness. This ar cle elucidates the shared roots between health psychology and mindfulness as a psychological construct and fi eld of research, providing a frame of reference for the ways in which health psychology and mindfulness share similar theore cal and methodological challenges that aff ect their integra on into health, social systems, and services. Keywords: mindfulness, history, philosophy Resumo O recente aumento na popularidade do conceito mindfulness (plena atenção) tem sido notado signifi ca vamente na área acadêmica e professional da psicologia. O termo tem se fortalecido nas ciências da saúde, além do imaginário cultural para expressar um contexto contemporâneo da sociedade, atraindo tanto especialistas quanto leigos. Sendo uma sub-área estabelecida rela vamente tardia no fi nal do século XX, a psicologia da saúde tem uma relação singular com o conceito. -

When Psychometrics Meets Epidemiology and the Studies V1.Pdf
When psychometrics meets epidemiology, and the studies which result! Tom Booth [email protected] Lecturer in Quantitative Research Methods, Department of Psychology, University of Edinburgh Who am I? • MSc and PhD in Organisational Psychology – ESRC AQM Scholarship • Manchester Business School, University of Manchester • Topic: Personality psychometrics • Post-doctoral Researcher • Centre for Cognitive Ageing and Cognitive Epidemiology, Department of Psychology, University of Edinburgh. • Primary Research Topic: Cognitive ageing, brain imaging. • Lecturer Quantitative Research Methods • Department of Psychology, University of Edinburgh • Primary Research Topics: Individual differences and health; cognitive ability and brain imaging; Psychometric methods and assessment. Journey of a talk…. • Psychometrics: • Performance of likert-type response scales for personality data. • Murray, Booth & Molenaar (2015) • Epidemiology: • Allostatic load • Measurement: Booth, Starr & Deary (2013); (Unpublished) • Applications: Early life adversity (Unpublished) • Further applications Journey of a talk…. • Methodological interlude: • The issue of optimal time scales. • Individual differences and health: • Personality and Physical Health (review: Murray & Booth, 2015) • Personality, health behaviours and brain integrity (Booth, Mottus et al., 2014) • Looking forward Psychometrics My spiritual home… Middle response options Strongly Agree Agree Neither Agree nor Disagree Strong Disagree Disagree 1 2 3 4 5 Strongly Agree Agree Unsure Disagree Strong Disagree -

Health Psychology 19
PSY_C19.qxd 1/2/05 3:52 pm Page 408 Health Psychology 19 CHAPTER OUTLINE LEARNING OBJECTIVES INTRODUCTION HEALTH BELIEFS AND BEHAVIOURS Behaviour and mortality The role of health beliefs Integrated models ILLNESS BELIEFS The dimensions of illness beliefs A model of illness behaviour Health professionals’ beliefs THE STRESS–ILLNESS LINK Stress models Does stress cause illness? CHRONIC ILLNESS Profile of an illness Psychology’s role FINAL THOUGHTS SUMMARY REVISION QUESTIONS FURTHER READING PSY_C19.qxd 1/2/05 3:52 pm Page 409 Learning Objectives By the end of this chapter you should appreciate that: n health psychologists study the role of psychology in health and wellbeing; n they examine health beliefs as possible predictors of health-related behaviours; n health psychology also examines beliefs about illness and how people conceptualize their illness; n a health professional’s beliefs about the symptoms, the illness or the patient can have important implications; n stress is the product of the interaction between the person and their environment – it can influence illness and the stress–illness link is influenced by coping and social support; n beliefs and behaviours can influence whether a person becomes ill in the first place, whether they seek help and how they adjust to their illness. INTRODUCTION Health psychology is a relatively recent yet fast- reflects the biopsychosocial model of health and growing sub-discipline of psychology. It is best illness that was developed by Engel (1977, understood by answering the following questions: 1980). Because, in this model, illness biopsychosocial the type of inter- n What causes illness and who is responsible is regarded as the action between biological factors (e.g. -

Clinical Health Psychology Fellowship
Clinical Health Psychology Fellowship APA-ACCREDITED CLINICAL HEALTH PSYCHOLOGY FELLOWSHIP AT THE MAYO CLINIC APA-Accredited Clinical Health Psychology Fellowship at the Mayo Clinic The Clinical Health Psychology Fellowship is one of three tracks offered in the Medical Psychology Post-Doctoral Fellowship at Mayo Clinic. This APA-Accredited Fellowship is the Department of Psychiatry and Psychology, which is one of the largest psychiatric treatment groups in the United States, with more than 80 psychologists and psychiatrists. The two-year fellowship includes clinical activities, 30% protected time for research, educational activities, as well as opportunities for teaching/leadership. The Clinical Health Psychology Fellowship offers both breadth and depth in health psychology training. Fellows choose a specialty area (“major rotation”) in which they focus the majority of their clinical and research work. Fellows receive their clinical supervision and research mentorship in their specialty area. In addition, fellows can obtain broad training through several minor rotations. The rotational schedule is flexible based on the fellows’ interests and goals. All major rotation areas are also offered as minor rotations. “Fellows are able to complete minor rotations in each specialty area during the two-year fellowship, or they may choose to focus on their major area of concentration.” Many of our faculty hold leadership positions in the department and the institution, offering our fellows formal and informal professional development opportunities to learn about the role of the Clinical Health Psychologist within an academic medical center setting. Our faculty includes individuals from diverse cultural and clinical training backgrounds. We strongly encourage diverse applicants to apply to our program, including international applicants. -

Social Justice: What Has Health Psychology Contributed?
3 THE EUROPEAN HEALTH PSYCHOLOGIST Volume 13, March 2011 ask the expert Social Justice: What Has Health Psychology Contributed? Anthony Montgomery University of Macedonia, Greece The current economic crisis in Europe behoves all organisations to re-examine the contribution that they make to society. Put simply, society wants to know if it is getting value for money from the services and organisations they fund. The EHPS is predominately populated by university employees whose salaries are (typically) funded by taxpay- ers. Thus, the need for Health Psychology to be relevant has never been more important. The present article was prompted, in some part, by the thought provoking keynote speech by Prof. Michael Murray (EHPS Cluj; 2010), whereby Michael suggested that Health Psychology has a weak ego and challenged us all to ruminate on how our ac- tivities impact upon society. This is a good question, and deserves an answer. With all the aforementioned in mind, I have approached a sample of senior health psychologists to ascertain their personal experiences of how their own careers have contributed to social justice in the world. The following arti- cle represents their responses to the following question: “Looking back on your career, in what way has your own work contributed to social justice in the world?” What is social justice? Social justice involves creat- ing a society based on principles of equality and solidarity, that understands and values human rights, and that recog- nises the dignity of every human being. At its 2007 World Summit for Social Development, the United Nations pro- claimed 20 February as World Day of Social Justice. -

Schonfeld, I. S. and Chang, C.: Occupational Health Psychology. Springer Publishing Company, New York, 2017, 355 Pp, $50.20 (Softbound)
Journal of Occupational Rehabilitation (2019) 29:239 https://doi.org/10.1007/s10926-018-9817-3 BOOK REVIEW Schonfeld, I. S. and Chang, C.: Occupational Health Psychology. Springer Publishing Company, New York, 2017, 355 pp, $50.20 (softbound) Bruce A. Barron1 Published online: 31 October 2018 © Springer Science+Business Media, LLC, part of Springer Nature 2018 The psychology of work is critical to employee mental and a wealth of relevant information regarding workplace vio- physical health. Occupational health psychology (OHP) is lence, organizational climate and leadership, occupational a complex subject because the mental health of employees safety, work–life balance, and practical primary, secondary, not only impacts workplace performance and productivity; and tertiary OHP interventions. workplace stressors can adversely affect worker psychologi- Overall, the text is expertly written by authoritative cal and physical well-being. Therefore, understanding occu- authors. Although published for undergraduate and gradu- pational health psychology is critically important regarding ate survey courses, the authors’ assessment of depression, employee primary, secondary, and tertiary prevention of burnout, and other employee health conditions in addition work-related injuries and illnesses. One of the major goals to workplace factors such as organization and leadership of Occupational Health Psychology is to provide the reader should prove useful to most occupational health profession- with relevant information that will further their knowledge als, disability case managers, and others interested in maxi- in this interdisciplinary subfield of psychology. mizing employee well-being, performance, and productivity Occupational Health Psychology is a comprehensive text as well as minimizing work-related injury, illness, and dis- that is logically organized into 11 chapters. -

American Board of Clinical Health Psychology Candidate Manual
American Board of Clinical Health Psychology Candidate Manual American Board of Professional Psychology (ABPP) September 2018 Table of Contents Introduction .......................................................................................................................... 4 Definition of the Specialty .................................................................................................... 4 Functional Competency Domains ........................................................................................ 4 Assessment ............................................................................................................. 4 Intervention .............................................................................................................. 5 Consultation ............................................................................................................. 5 Management/Administration .................................................................................... 6 Research and/or Evaluation …………………………………………………………….6 Supervision………………………………………………………………………………...6 Teaching…………………………………………………………………………………...6 Advocacy…………………………………………………………………………………..7 Foundational Competency Domains .................................................................................... 7 Professionalism ........................................................................................................ 7 Reflective Practice, Self-Assessment, and Self-Care .............................................. 7 Scientific -

Chapter 6 Understanding and Promoting Physical Activity
CHAPTER 6 UNDERSTANDING AND PROMOTING PHYSICAL ACTIVITY Contents Introduction . 211 Theories and Models Used in Behavioral and Social Science Research on Physical Activity . 211 Learning Theories . 211 Health Belief Model . 213 Transtheoretical Model . 213 Relapse Prevention Model . 213 Theory of Reasoned Action and Theory of Planned Behavior . 213 Social Learning/Social Cognitive Theory . 214 Social Support . 214 Ecological Approaches . 214 Summary . 215 Behavioral Research on Physical Activity among Adults . 215 Factors Influencing Physical Activity among Adults . 215 Modifiable Determinants . 215 Determinants for Population Subgroups . 216 Summary . 217 Interventions to Promote Physical Activity among Adults . 217 Individual Approaches . 217 Interventions in Health Care Settings . 226 Community Approaches . 227 Worksite Programs . 229 Communications Strategies . 231 Special Population Programs . 232 Racial and Ethnic Minorities . 232 People Who Are Overweight . 232 Contents, continued Older Adults . 233 People with Disabilities . 233 Summary . 234 Behavioral Research on Physical Activity among Children and Adolescents . 234 Factors Influencing Physical Activity among Children and Adolescents . 234 Modifiable Determinants . 234 Determinants for Population Subgroups . 235 Summary . 236 Interventions to Promote Physical Activity among Children and Adolescents . 236 School Programs . 236 School-Community Programs . 242 Interventions in Health Care Settings . 242 Special Population Programs . 243 Summary . 243 Promising Approaches, Barriers, and Resources . 243 Environmental and Policy Approaches . 244 Community-Based Approaches . 245 Societal Barriers . 246 Societal Resources . 247 Summary . 248 Chapter Summary . 248 Conclusions . 249 Research Needs . 249 Determinants of Physical Activity . 249 Physical Activity Interventions . 249 References . 249 CHAPTER 6 UNDERSTANDING AND PROMOTING PHYSICAL ACTIVITY Introduction some of these have been applied extensively in inter- s the benefits of moderate, regular physical vention research as well. -

Compensatory Health Beliefs: Scale Development and Psychometric Properties
Psychology and Health October 2004, Vol. 19, No. 5, pp. 607–624 COMPENSATORY HEALTH BELIEFS: SCALE DEVELOPMENT AND PSYCHOMETRIC PROPERTIES BA¨RBEL KNA¨UPER*, MARJORIE RABIAU, OSHRA COHEN and NICHOLAS PATRICIU Department of Psychology, McGill University, 1205 Dr. Penfield Avenue, Montreal, QC, Canada H3A 1B1 (Received 18 June 2003; In final form 14 November 2003) Compensatory Health Beliefs (CHBs) are beliefs that the negative effects of an unhealthy behavior can be compensated for, or ‘‘neutralised,’’ by engaging in a healthy behavior. ‘‘I can eat this piece of cake now because I will exercise this evening’’ is an example of such beliefs. The present research describes a psycho- metric scale to measure CHBs (Study 1) and provides data on its reliability and validity (Studies 2 and 3). The results show that scores on the scale are uniquely associated with health-related risk behaviors and symp- tom reports and can be differentiated from a number of related constructs, including irrational health beliefs. Holding CHBs may hinder individuals from acquiring healthier lifestyles, for example lose weight or exercise. Keywords: Compensatory health beliefs; Irrational health beliefs; Anticipated pleasure; Self-efficacy; Dissonance; Health behavior INTRODUCTION In the past few decades, much attention has been focused on health behaviors and their consequences for health outcomes. Ample empirical evidence demonstrates that behavioral and life-style factors such as smoking, being overweight or obese, and lack of exercise are major determinants of morbidity and mortality (see McGinnis and Foege, 1993). People are quite knowledgeable about the maladaptive effects of over-consumption of food, nicotine, alcohol, and lack of exercise (cf. -
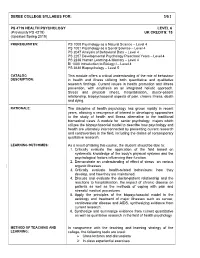
Deree College Syllabus For: 3/0/ 3
DEREE COLLEGE SYLLABUS FOR: 3/0/ 3 PS 4 719 HEALTH PSYCHOLOGY LEVEL 6 (Previously PS 4219) UK CREDITS: 15 (Updated Spring 2019) PREREQUISITES: PS 1000 Psychology as a Natural Science – Level 4 PS 1001 Psychology as a Social Science – Level 4 PS 2047 Analysis of Behavioral Data – Level 4 PS 2207 Developmental Psychology Preschool Years – Level 4 PS 2236 Human Learning & Memory – Level 4 BI 1000 Introduction to Biology I – Level 4 PS 3630 Biopsychology – Level 5 CATALOG This module offers a critical understanding of the role of behaviour DESCRIPTION: in health and illness utilizing both quantitative and qualitative research findings. Current issues in health promotion and illness prevention, with emphasis on an integrated holistic approach. Stress and physical illness, hospitalisation, doctor-patient relationship, biopsychosocial aspects of pain, chronic illness, death and dying. RATIONALE: The discipline of health psychology has grown rapidly in recent years, allowing a resurgence of interest in developing approaches to the study of health and illness alternative to the traditional biomedical views. A module for senior psychology majors which utilizes the biopsychosocial model to describe how psychology and health are ultimately interconnected by presenting current research and controversies in the field, including the claims of contemporary qualitative research. LEARNING OUTCOMES: As a result of taking this course, the student should be able to: 1. Critically evaluate the application of the field based on systematic knowledge of the body's physical systems and the psychological factors influencing their function. 2. Demonstrate an understanding of effect of stress on various organic illnesses 3. Critically evaluate health-related behaviours: how they develop, and how they are maintained. -

Perceived Self-Efficacy Self-Efficacy and Health Behavior Theories
Self-Efficacy, p. 1 Perceived Self-Efficacy Ralf Schwarzer Freie Universitat Berlin, Germany & Aleksandra Luszczynska University of Sussex, UK Self-Efficacy and Health Behavior Theories Most prominent health behavior theories include self-efficacy (or similar constructs). Self-efficacy is a proximal and direct predictor of intention and of behavior. According to Social Cognitive Theory (SCT; Bandura, 1997), a personal sense of control facilitates a change of health behavior. Self-efficacy pertains to a sense of control over one’s environment and behavior. Self-efficacy beliefs are cognitions that determine whether health behavior change will be initiated, how much effort will be expended, and how long it will be sustained in the face of obstacles and failures. Self-efficacy influences the effort one puts forth to change risk behavior and the persistence to continue striving despite barriers and setbacks that may undermine motivation. Self-efficacy is directly related to health behavior, but it also affects health behaviors indirectly through its impact on goals. Self-efficacy influences the challenges that people take on as well as how high they set their goals (e.g., “I intend to reduce my smoking,” or “I intend to quit smoking altogether”). Individuals with strong self-efficacy select more challenging goals (DeVellis & DeVellis, 2000). They focus on opportunities, not on obstacles (e.g., “At my university there is a smoking ban, anyway,” instead of “There are still a lot of ashtrays at my university.”). According to the Theory of Planned Behavior (TPB; Ajzen, 1991), intention is the most proximal predictor of behavior. Cognitions that affect a specific intention are attitudes, Self-Efficacy, p. -

The Pre-History of Health Psychology in the UK: from Natural Science and Psychoanalysis to Social Science, Social Cognition and Beyond Introduction
The pre-history of health psychology in the UK: From natural science and psychoanalysis to social science, social cognition and beyond Introduction Michael Murray Keele University, UK To be published in Journal of Health Psychology 10 January 2017 1 Abstract Health psychology formally came of age in the UK in the 1980s but it was prefigured by much discussion about challenges to the dominance of biomedicine in healthcare and debates about the role of individual behaviour change in promoting population health. Despite current progress and accomplishments it is important to reflect upon earlier attempts to explore the psychological dimensions of health and illness. It is through such exploration that we can begin to reveal the connection between ideas and the social context. This paper focuses on what could be termed the pre-history of health psychology in the UK. This was the period in the earlier twentieth century when psychological approaches were dominated by psychoanalysis which was in tension with more positivist approaches. In the post WWII period the classical form of psychoanalysis turned to a concern with relationships. This was the period which also saw the rise of behaviourism and then cognitivism each of which had a strong influence on the new profession of clinical psychology and then health psychology. 2 The pre-history of health psychology in the UK: From natural science and psychoanalysis to social science, social cognition and beyond Introduction Psychological theory and practice are not constructed in isolation from the social world but rather are shaped by it and contribute to our interpretation of reality.