FEMARA (Letrozole) 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

X FACT SHEET
Letrozole For the Patient: Letrozole Other names: FEMARA • Letrozole (LET-roe-zole) is a drug that is used to treat breast cancer. It only works in women who are post-menopausal and producing estrogen outside the ovaries. Many cancers are hormone sensitive (estrogen or progesterone receptor positive) and their growth can be affected by lowering estrogen levels in the body. Letrozole is used to help reduce the amount of estrogen produced by your body and decrease the growth of hormone sensitive tumors. Letrozole is a tablet that you take by mouth. The tablet may contain lactose. • It is important to take letrozole exactly as directed by your doctor. Make sure you understand the directions. • Letrozole may be taken with food or on an empty stomach. • If you miss a dose of letrozole, take it as soon as you can if it is within 12 hours of the missed dose. If it is over 12 hours since your missed dose, skip the missed dose and go back to your usual dosing times. • Other drugs such as tamoxifen (NOLVADEX) and raloxifen (EVISTA) may interact with letrozole. Because letrozole works by reducing the amount of estrogen produced by your body, it is recommended that you avoid taking estrogen replacement therapy such as conjugated estrogens (PREMARIN, C.E.S., ESTRACE, ESTRACOMB, ESTRADERM, ESTRING). Tell your doctor if you are taking this or any other drugs as you may need extra blood tests or your dose may need to be changed. Check with your doctor or pharmacist before you start taking any new drugs. • The drinking of alcohol (in small amounts) does not appear to affect the safety or usefulness of letrozole. -

Aromatase Inhibitors
FACTS FOR LIFE Aromatase Inhibitors What are aromatase inhibitors? Aromatase Inhibitors vs. Tamoxifen Aromatase inhibitors (AIs) are a type of hormone therapy used to treat some breast cancers. They AIs and tamoxifen are both hormone therapies, are taken in pill form and can be started after but they act in different ways: surgery or radiation therapy. They are only given • AIs lower the amount of estrogen in the body to postmenopausal women who have a hormone by stopping certain hormones from turning receptor-positive tumor, a tumor that needs estrogen into estrogen. If estrogen levels are low to grow. enough, the tumor cannot grow. AIs are used to stop certain hormones from turning • Tamoxifen blocks estrogen receptors on breast into estrogen. In doing so, these drugs lower the cancer cells. Estrogen is still present in normal amount of estrogen in the body. levels, but the breast cancer cells cannot get enough of it to grow. Generic/Brand names of AI’s As part of their treatment plan, some post- Generic name Brand name menopausal women will use AIs alone. Others anastrozole Arimidex will use tamoxifen for 1-5 years and then begin exemestane Aromasin using AIs. letrozole Femara Who can use aromatase inhibitors? Postmenopausal women with early stage and metastatic breast cancer are often treated with AIs. After menopause, the ovaries produce only a small amount of estrogen. AIs stop the body from making estrogen, and as a result hormone receptor-positive tumors do not get fed by estrogen and die. AIs are not given to premenopausal women because their ovaries still produce estrogen. -

Acupuncture Plus Herbal Medicine PCOS Finding
Acupuncture Plus Herbal Medicine PCOS Finding Published by HealthCMI on 18 February 2018. Acupuncture plus herbal medicine increase the clinical effective rate of drug therapy for the treatment of polycystic ovary syndrome (PCOS). In research conducted at the Hubei Maternal and Child Care Service Center, drug therapy using cyproterone acetate/ethinylestradiol and letrozole produced an 72.5% total effective rate. Using both drugs and herbal medicine produced an 85.0% total effective rate, and the rate increased to 95.0% when acupuncture was added to the treatment regimen. Cyproterone acetate/ethinylestradiol is a commonly used medicine for the treatment of PCOS. Letrozole is an aromatase inhibitor used to stimulate ovulation in women with PCOS. The following parameters were used to evaluate treatment efficacy: menstruation improvements, body weight, body mass index (BMI), luteal hormone (LH), follicle stimulating hormone (FSH), LH/FSH ratio, total testosterone (T), and estradiol (E2)]. An enzyme linked immunosorbent assay was adopted to determine the content of anti-Mullerian hormone (AMH) and inhibin B (IHNB). In Traditional Chinese Medicine, PCOS falls under the Yue Jing Hou Qi (delayed menstruation), Bi Jing (amenorrhea), or the Bu Yun (infertility) class of disorders. Kidney deficiency is one primary cause. Binding of qi, phlegm, and stasis is a secondary cause. The treatment principle is to supplement the kidney essence, boost the liver and spleen, promote blood circulation, and dispel phlegm. Let’s take a look at the treatment protocols that achieved clinical success in the study. A total of 120 patients from Hubei Maternal and Child Care Service Center participated in the study. -

Letrozole (Femara)
Letrozole (Femara) Letrozole (Femara) is a medication that was first reported to be effective for ovulation induction in 2000. It is classified as an Aromatase Inhibitor (AI) and was developed to reduce the risk of recurrence of breast cancer. Even though its use is considered “off label” for fertility treatment, there is good evidence supporting its efficacy and safety for ovulation induction. How does it work? Letrozole works by binding to aromatase, an enzyme needed to make Estrogen. By temporarily decreasing Estrogen levels at the beginning of a menstrual cycle, Letrozole signals the pituitary gland to release more Follicle Stimulating Hormone (FSH). FSH stimulates the development of ovarian follicles, the fluid filled structure in which eggs reside and mature. Letrozole may lead to one or more eggs being ovulated and regulate the menstrual cycle. Ovulation typically occurs 5-8 days after the last letrozole tablet. When a mature follicle is present, a surge of LH hormone is released by the pituitary which causes the egg to be released from the follicle. Ovulation will occur 24-48 hours after the surge. What is the standard dose? The Letrozole dosage is 2.5mg for five consecutive days – typically cycle Day 3 to 7 (with cycle day 1 being the first day of full menstrual flow). It is taken orally at approximately the same time each day. How do I know when I am going to get an LH surge? The easiest way to detect your LH surge is with an ovulation predictor kit (OPK). This is a urine test that is done daily beginning a couple of days before you expect to ovulate. -

Letrozole Use for Fertility Has Been Widely Studied
(802)655-8888 nrmvt.com Letrozole Letrozole is an aromatase inhibitor used to induce ovulation in patients with irregular menses or no menses at all. Letrozole works to induce ovulation by blocking estrogen production, leading to increases in follicle-stimulating hormone (FSH) release. You may be prescribed this medication if you have polycystic ovary syndrome (PCOS) or problems with ovulation. The use of letrozole for ovulation induction is off-label, meaning the FDA has not approved this indication. However, letrozole use for fertility has been widely studied. Most recently, the National Institutes of Health evaluated the effect of letrozole in patients with ovulatory infertility or PCOS. Dr Peter Casson was one of the principal investigators of this national, multi-center, randomized-controlled trial published in the New England Journal of Medicine that analyzed letrozole head to head with another commonly used medication, clomiphene citrate, and found letrozole to be superior. Who may be a candidate for letrozole? 1. Patients with PCOS or ovulatory infertility. 2. Patients with other types of infertility that have side effects or contraindications to Clomid. What is the success rate? Success rates differ by female age and fertility diagnosis. In general, successful ovulation occurs in 60% of cycles, and live birth rate for patients with PCOS who are <35 years old is 15-17% per cycle. What about twins? Triplets? The risk of twins with letrozole is estimated to be approximately 3-5%, which appears to be lower than the risk of twins with clomiphene citrate (7-8%), but is still higher than the risk of twins in a spontaneous pregnancy (2-3%). -

A Randomized Phase II Study of Letrozole Versus Observation in Patients with Newly Diagnosed Uterine Leiomyosarcoma 2006-0453
2006-0453 Revised 4/29/2009 Page 1 Protocol Page A Randomized Phase II Study of Letrozole Versus Observation in Patients with Newly Diagnosed Uterine Leiomyosarcoma 2006-0453 Core Protocol Information Short Title Letrozole versus observation in patients with newly diagnosed uterine leiomyosarcoma Study Chair: Robert Coleman Additional Contact: Aileen Maloney Jacalyn B. Gano PDOL OPR DMC Addl Cont Department: Gynecologic Oncology Phone: 713-794-1422 Unit: 1352 Full Title: A Randomized Phase II Study of Letrozole Versus Observation in Patients with Newly Diagnosed Uterine Leiomyosarcoma Protocol Type: Standard Protocol Protocol Phase: Phase II Version Status: Terminated 07/24/2017 Version: 08 Submitted by: Aileen Maloney--6/8/2009 10:18:41 AM OPR Action: Accepted by: Leola M. Jones -- 6/16/2009 1:06:28 PM Which Committee will review this protocol? The Clinical Research Committee - (CRC) 2006-0453 Revised 4/29/2009 Page 2 Protocol Body 1.0 Objectives To prolong the time to recurrence for patients with clinical stage I and II uterine LMS assigned to letrozole therapy. The primary endpoint of this study will be a prolongation of time to disease recurrence. 2.0 Background Letrozole (4,4'-(1H-1,2,4-Triazol-1-ylmethylene)bis-benzonitrile) is a synthetic achiral benzydryltriazole derivative. It is an orally active highly selective non-steroidal competitive inhibitor of the aromatase enzyme system [1,2]. Aromatase inhibitors block the aromatase enzyme, consequently lowering estrogen levels and thereby deprive the tumor of its growth stimulus. Letrozole effectively inhibits the conversion of androgens to estrogens in both in vitro and in vivo [1]. -

Cancer Drug Costs for a Month of Treatment at Initial Food and Drug
Cancer drug costs for a month of treatment at initial Food and Drug Administration approval Year of FDA Monthly Cost Monthly cost Generic name Brand name(s) approval (actual $'s) (2014 $'s) vinblastine Velban 1965 $78 $586 thioguanine, 6-TG Thioguanine Tabloid 1966 $17 $124 hydroxyurea Hydrea 1967 $14 $99 cytarabine Cytosar-U, Tarabine PFS 1969 $13 $84 procarbazine Matulane 1969 $2 $13 testolactone Teslac 1969 $179 $1,158 mitotane Lysodren 1970 $134 $816 plicamycin Mithracin 1970 $50 $305 mitomycin C Mutamycin 1974 $5 $23 dacarbazine DTIC-Dome 1975 $29 $128 lomustine CeeNU 1976 $10 $42 carmustine BiCNU, BCNU 1977 $33 $129 tamoxifen citrate Nolvadex 1977 $44 $170 cisplatin Platinol 1978 $125 $454 estramustine Emcyt 1981 $420 $1,094 streptozocin Zanosar 1982 $61 $150 etoposide, VP-16 Vepesid 1983 $181 $430 interferon alfa 2a Roferon A 1986 $742 $1,603 daunorubicin, daunomycin Cerubidine 1987 $533 $1,111 doxorubicin Adriamycin 1987 $521 $1,086 mitoxantrone Novantrone 1987 $477 $994 ifosfamide IFEX 1988 $1,667 $3,336 flutamide Eulexin 1989 $213 $406 altretamine Hexalen 1990 $341 $618 idarubicin Idamycin 1990 $227 $411 levamisole Ergamisol 1990 $105 $191 carboplatin Paraplatin 1991 $860 $1,495 fludarabine phosphate Fludara 1991 $662 $1,151 pamidronate Aredia 1991 $507 $881 pentostatin Nipent 1991 $1,767 $3,071 aldesleukin Proleukin 1992 $13,503 $22,784 melphalan Alkeran 1992 $35 $59 cladribine Leustatin, 2-CdA 1993 $764 $1,252 asparaginase Elspar 1994 $694 $1,109 paclitaxel Taxol 1994 $2,614 $4,176 pegaspargase Oncaspar 1994 $3,006 $4,802 -
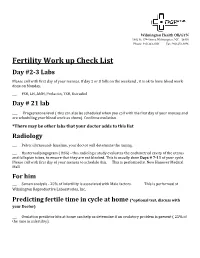
Fertility Work up Check List
Wilmington Health OB/GYN 1802 So 17th Street, Wilmington, NC 28401 Phone: 910-343-1031 Fax: 910-251-8896 Fertility Work up Check List Day #2-3 Labs Please call with first day of your menses. If day 2 or 3 falls on the weekend , it is ok to have blood work done on Monday. ___ FSH, LH, AMH, Prolactin, TSH, Estradiol Day # 21 lab ___ Progesterone level ( this can also be scheduled when you call with the first day of your menses and are scheduling your blood work as above). Confirms ovulation. *There may be other labs that your doctor adds to this list Radiology ___ Pelvic ultrasound- baseline, your doctor will determine the timing. ___ Hysterosalpingogram ( HSG) - this radiologic study evaluates the endometrial cavity of the uterus and fallopian tubes, to ensure that they are not blocked. This is usually done Days # 7-11 of your cycle. Please call with first day of your menses to schedule this. This is performed at New Hanover Medical Mall. For him ___ Semen analysis - 25% of infertility is associated with Male factors. This is performed at Wilmington Reproductive Laboratories, Inc. Predicting fertile time in cycle at home (*optional test, discuss with your Doctor) ___ Ovulation predictor kits at home can help us determine if an ovulatory problem is present ( 25% of the time in infertility). Here is a list of ACCURATE and FREE menstrual cycle tracking apps • Clue • Day After • FemCal Lite • The Flow • Glow • Groove • iPeriod Period Tracker Free • It's a Girl Thing • Lily • LoveCycles Menstrual, Ovulation & Period Tracker • Menstruation & Ovulation (now known as the "Menstrual Period Tracker") • Mom and Baby to Be • MonthPal ("Touchable Period Tracker") • Period Tracker • GP Apps • Period Tracker, Free Menstrual Calendar • Pink Pad Period & Fertility Tracker Pro Wilmington Health OB/GYN 1802 So 17th Street, Wilmington, NC 28401 Phone: 910-343-1031 Fax: 910-251-8896 Femara (Letrozole) Protocol • Letrozole is commonly used for infertility treatment to induce an egg to develop and to be released in women who are not ovulating on their own. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

NIOSH List of Antineoplastic and Other Hazardous Drugs in Healthcare Settings 2010
NIOSH List of Antineoplastic and Other Hazardous Drugs in Healthcare Settings 2010 DEPARTMENT OF HEALTH AND HUMAN SERVICES Centers for Disease Control and Prevention National Institute for Occupational Safety and Health NIOSH List of Antineoplastic and Other Hazardous Drugs in Healthcare Settings 2010 DEPARTMENT OF HEALTH AND HUMAN SERVICES Centers for Disease Control and Prevention National Institute for Occupational Safety and Health This document is in the public domain and may be freely copied or reprinted. DISCLAIMER Mention of any company or product does not constitute endorsement by the National Institute for Occupational Safety and Health (NIOSH). In addition, citations to Web sites external to NIOSH do not constitute NIOSH endorsement of the sponsoring organizations or their programs or products. Furthermore, NIOSH is not responsible for the content of these Web sites. ORDERING INFORMATION To receive documents or other information about occupational safety and health topics, contact NIOSH at Telephone: 1–800–CDC–INFO (1–800–232–4636) TTY:1–888–232–6348 E-mail: [email protected] or visit the NIOSH Web site at www.cdc.gov/niosh For a monthly update on news at NIOSH, subscribe to NIOSH eNews by visiting www.cdc.gov/niosh/eNews. DHHS (NIOSH) Publication Number 2010−167 September 2010 Preamble: The National Institute for Occupational Safety and Health (NIOSH) Alert: Preventing Occupational Exposures to Antineoplastic and Other Hazardous Drugs in Health Care Settings was published in September 2004 (http://www.cdc.gov/niosh/docs/2004-165/). In Appendix A of the Alert, NIOSH identified a sample list of major hazardous drugs. The list was compiled from infor- mation provided by four institutions that have generated lists of hazardous drugs for their respec- tive facilities and by the Pharmaceutical Research and Manufacturers of America (PhRMA) from the American Hospital Formulary Service Drug Information (AHFS DI) monographs [ASHP/ AHFS DI 2003]. -

Letrozole Once a Week Normalizes Serum Testosterone in Obesity-Related Male Hypogonadism
European Journal of Endocrinology (2008) 158 741–747 ISSN 0804-4643 CLINICAL STUDY Letrozole once a week normalizes serum testosterone in obesity-related male hypogonadism Sandra Loves1, Janneke Ruinemans-Koerts2 and Hans de Boer1 Departments of 1Internal Medicine and 2Clinical Chemistry, Ziekenhuis Rijnstate, Wagnerlaan 55, 6800 TA Arnhem, The Netherlands (Correspondence should be addressed to H de Boer; Email: [email protected]) Abstract Objective: Isolated hypogonadotropic hypogonadism (IHH) is frequently observed in severely obese men, probably as a result of increased estradiol (E2) production and E2-mediated negative feedback on pituitary LH secretion. Aromatase inhibitors can reverse this process. This study evaluates whether letrozole once a week can normalize serum testosterone in severely obese men and maintain its long term effect. Design: Open, uncontrolled 6-month pilot study in 12 severely obese men (body mass indexO 35.0 kg/m2) with obesity-related IHH and free testosterone levels !225 pmol/l, treated with 2.5 mg letrozole once a week for 6 months. Results: Six weeks of treatment reduced total E2 from 123G11 to 58G7 pmol/l (P!0.001, meanG S.E.M.), and increased serum LH from 4.4G0.6 to 11.1G1.5 U/l (P!0.001). Total testosterone rose from 5.9G0.5 to 19.6G1.4 nmol/l (P!0.001), and free testosterone from 163G13 to 604G 50 pmol/l (P!0.001). Total testosterone rose to within the normal range in all subjects, whereas free testosterone rose to supraphysiological levels in 7 out of 12 men. The testosterone and E2 levels were stable throughout the week and during the 6-month treatment period. -

Effects of Raloxifene Against Letrozole-Induced Bone Loss in Chemically-Induced Model of Menopause in Mice
Proceedings of the British Pharmacological Society at http://www.pA2online.org/abstracts/Vol16Issue1abst005P.pdf Effects of raloxifene against letrozole-induced bone loss in chemically-induced model of menopause in mice D. Vohora, A. Kalam. Pharmacology, Hamdard University, New Delhi, New Delhi, INDIA. Introduction: The deleterious effects of letrozole, an aromatase inhibitor, used in the adjuvant treatment of breast cancer in postmenopausal women, on bone are well-documented and represent a major drawback to its clinical use. Raloxifene, a selective estrogen receptor modulator and a clinically approved anti-osteoporotic drug, has been recently demonstrated to be efficacious in women with breast cancer. The present study evaluated the effects of preventive and curative treatment with raloxifene on letrozole-induced alterations of bone microarchitecture and turnover markers in a chemically-induced menopause model in mice. Method: Swiss strain albino female mice were made menopausal by inducing ovotoxicity using vinyl cyclohexene di epoxide (VCD, 160mg/kg for 15 days followed by 30 days drug-free period) confirmed by ovarian histology and serum estradiol levels. Effects on femoral and lumbar bones were evaluated by micro CT determination of bone volume, trabecular number, separation, thickness, connective density and trabecular pattern factor and bone turnover markers including ALP, TRAP5b, hydroxyproline and RANKL. In addition to these, markers of Wnt signaling (sclerostin and dickkopf-1) were also evaluated. To rule out the involvement of pharmacokinetic interaction, plasma levels of letrozole and raloxifene were measured following drugs alone and in combination. Results: Though bone loss was observed in VCD treated mice (as indicated by micro CT measurements), it was further enhanced with letrozole administration (1 mg/kg) for one month particularly in epiphysis of femoral bones but also in lumbar vertebrae.