Osteoid Osteoma of Mandibular Bone Case Report and Review of The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bone and Soft Tissue Tumors Have Been Treated Separately
EPIDEMIOLOGY z Sarcomas are rare tumors compared to other BONE AND SOFT malignancies: 8,700 new sarcomas in 2001, with TISSUE TUMORS 4,400 deaths. z The incidence of sarcomas is around 3-4/100,000. z Slight male predominance (with some subtypes more common in women). z Majority of soft tissue tumors affect older adults, but important sub-groups occur predominantly or exclusively in children. z Incidence of benign soft tissue tumors not known, but Fabrizio Remotti MD probably outnumber malignant tumors 100:1. BONE AND SOFT TISSUE SOFT TISSUE TUMORS TUMORS z Traditionally bone and soft tissue tumors have been treated separately. z This separation will be maintained in the following presentation. z Soft tissue sarcomas will be treated first and the sarcomas of bone will follow. Nowhere in the picture….. DEFINITION Histological z Soft tissue pathology deals with tumors of the classification connective tissues. of soft tissue z The concept of soft tissue is understood broadly to tumors include non-osseous tumors of extremities, trunk wall, retroperitoneum and mediastinum, and head & neck. z Excluded (with a few exceptions) are organ specific tumors. 1 Histological ETIOLOGY classification of soft tissue tumors tumors z Oncogenic viruses introduce new genomic material in the cell, which encode for oncogenic proteins that disrupt the regulation of cellular proliferation. z Two DNA viruses have been linked to soft tissue sarcomas: – Human herpes virus 8 (HHV8) linked to Kaposi’s sarcoma – Epstein-Barr virus (EBV) linked to subtypes of leiomyosarcoma z In both instances the connection between viral infection and sarcoma is more common in immunosuppressed hosts. -

Osteoid Osteoma: Contemporary Management
eCommons@AKU Section of Orthopaedic Surgery Department of Surgery 2018 Osteoid osteoma: Contemporary management Shahryar Noordin Aga Khan University, [email protected] Salim Allana Emory University Kiran Hilal Aga Khan University, [email protected] Riaz Hussain Lukhadwala Aga Khan University, [email protected] Anum Sadruddin Pidani Aga Khan University, [email protected] See next page for additional authors Follow this and additional works at: https://ecommons.aku.edu/pakistan_fhs_mc_surg_orthop Part of the Orthopedics Commons, Radiology Commons, and the Surgery Commons Recommended Citation Noordin, S., Allana, S., Hilal, K., Lukhadwala, R. H., Pidani, A. S., Ud Din, N. (2018). Osteoid osteoma: Contemporary management. Orthopedic Reviews, 10(3), 108-119. Available at: https://ecommons.aku.edu/pakistan_fhs_mc_surg_orthop/92 Authors Shahryar Noordin, Salim Allana, Kiran Hilal, Riaz Hussain Lukhadwala, Anum Sadruddin Pidani, and Nasir Ud Din This article is available at eCommons@AKU: https://ecommons.aku.edu/pakistan_fhs_mc_surg_orthop/92 Orthopedic Reviews 2018; volume 10:7496 Osteoid osteoma: Contemporary management Epidemiology Correspondence: Shahryar Noordin, Orthopaedic Surgery, Aga Khan University, Osteoid osteoma accounts for around Karachi, Pakistan. Shahryar Noordin,1 Salim Allana,2 5% of all bone tumors and 11% of benign Tel.: 021.3486.4384. 4 Kiran Hilal,3 Naila Nadeem,3 bone tumors. Osteoid osteoma is the third E-mail: [email protected] Riaz Lakdawala,1 Anum Sadruddin,4 most common biopsy analyzed benign bone 5 tumor after osteochondroma and nonossify- Key words: Osteoid osteoma; tumor; benign; Nasir Uddin imaging; pathogenesis; management. 1 ing fibroma. Two to 3% of excised primary Orthopaedic Surgery, Aga Khan bone tumors are osteoid osteomas.5 Males University, Karachi, Pakistan; Contributions: SN, SA, study design, data col- are more commonly affected with an lection, manuscript writing; KH, NU, data col- 2 5 Department of Epidemiology, Rollins approximate male/female ratio of 2 to 1. -
View Presentation Notes
When is a musculoskeletal condition a tumor? Recognizing common bone and soft tissue tumors Christian M. Ogilvie, MD Assistant Professor of Orthopaedic Surgery University of Pennsylvania University of Pennsylvania Department of Orthopaedic Surgery Purpose • Recognize that tumors can present in the extremities of patients treated by athletic trainers • Know that tumors may present as a lump, pain or both • Become familiar with some bone and soft tissue tumors University of Pennsylvania Department of Orthopaedic Surgery Summary • Introduction – Pain – Lump • Bone tumors – Malignant – Benign • Soft tissue tumors – Malignant – Benign University of Pennsylvania Department of Orthopaedic Surgery Summary • Presentation • Imaging • History • Similar conditions –Injury University of Pennsylvania Department of Orthopaedic Surgery Introduction •Connective tissue tumors -Bone -Cartilage -Muscle -Fat -Synovium (lining of joints, tendons & bursae) -Nerve -Vessels •Malignant (cancerous): sarcoma •Benign University of Pennsylvania Department of Orthopaedic Surgery Introduction: Pain • Malignant bone tumors: usually • Benign bone tumors: some types • Malignant soft tissue tumors: not until large • Benign soft tissue tumors: some types University of Pennsylvania Department of Orthopaedic Surgery Introduction: Pain • Bone tumors – Not necessarily activity related – May be worse at night – Absence of trauma, mild trauma or remote trauma • Watch for referred patterns – Knee pain for hip problem – Arm and leg pains in spine lesions University of Pennsylvania -

Osteoid Osteoma and Your Everyday Practice
n Review Article Instructions 1. Review the stated learning objectives at the beginning cme ARTICLE of the CME article and determine if these objectives match your individual learning needs. 2. Read the article carefully. Do not neglect the tables and other illustrative materials, as they have been selected to enhance your knowledge and understanding. 3. The following quiz questions have been designed to provide a useful link between the CME article in the issue Osteoid Osteoma and your everyday practice. Read each question, choose the correct answer, and record your answer on the CME Registration Form at the end of the quiz. Petros J. Boscainos, MD, FRCSEd; Gerard R. Cousins, MBChB, BSc(MedSci), MRCS; 4. Type or print your full name and address and your date of birth in the space provided on the CME Registration Form. Rajiv Kulshreshtha, MBBS, MRCS; T. Barry Oliver, MBChB, MRCP, FRCR; 5. Indicate the total time spent on the activity (reading article and completing quiz). Forms and quizzes cannot be Panayiotis J. Papagelopoulos, MD, DSc processed if this section is incomplete. All participants are required by the accreditation agency to attest to the time spent completing the activity. educational objectives 6. Complete the Evaluation portion of the CME Regi stration Form. Forms and quizzes cannot be processed if the Evaluation As a result of reading this article, physicians should be able to: portion is incomplete. The Evaluation portion of the CME Registration Form will be separated from the quiz upon receipt at ORTHOPEDICS. Your evaluation of this activity will in no way affect educational1. -

What Is New in Orthopaedic Tumor Surgery?
15.11.2018 What is new in orthopaedic tumor surgery? Marko Bergovec, Andreas Leithner Department of Orhtopaedics and Trauma Medical University of Graz, Austria 1 15.11.2018 Two stories • A story about the incidental finding • A scary story with a happy end The story about the incidental finding • 12-year old football player • Small trauma during sport • Still, let’s do X-RAY 2 15.11.2018 The story about the incidental finding • Panic !!! • A child has a tumor !!! • All what a patient and parents hear is: – bone tumor = death – amputation – will he ever do sport again? • Still – what now? 3 15.11.2018 A scary story with a happy end • 12-year old football player • Small trauma during sport • 3 weeks pain not related to physical activity • “It is nothing, just keep it cool, take a rest” 4 15.11.2018 A scary story with a happy end • A time goes by • After two weeks of rest, pain increases... • OK, let’s do X-RAY 5 15.11.2018 TUMORS benign vs malign bone vs soft tissue primary vs metastasis SARCOMA • Austria – cca 200 patients / year – 1% of all malignant tumors • (breast carcinoma = 5500 / year) 6 15.11.2018 Distribution of the bone tumoris according to patients’ age and sex 250 200 150 100 broj bolesnika broj 50 M Ž 0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 80+ dob 7 15.11.2018 WHO Histologic Classification of Bone Tumors Bone-forming tumors Benign: Osteoma; Osteoid osteoma; Osteoblastoma Intermediate; Aggressive (malignant) osteoblastoma Malignant: Conventional central osteosarcoma; Telangiectatic osteosarcoma; Intraosseous well -

Primary Tumors of the Spine
280 Primary Tumors of the Spine Sebnem Orguc, MD1 Remide Arkun, MD1 1 Department of Radiology, Celal Bayar University, Manisa, Türkiye Address for correspondence Sebnem Orguc, MD, Department of 2 Department of Radiology, Ege University, İzmir, Türkiye Radiology, Celal Bayar University, Manisa, Türkiye (e-mail: [email protected]; [email protected]). Semin Musculoskelet Radiol 2014;18:280–299. Abstract Spinal tumors consist of a large spectrum of various histologic entities. Multiple spinal lesions frequently represent known metastatic disease or lymphoproliferative disease. In solitary lesions primary neoplasms of the spine should be considered. Primary spinal tumors may arise from the spinal cord, the surrounding leptomeninges, or the extradural soft tissues and bony structures. A wide variety of benign neoplasms can involve the spine including enostosis, osteoid osteoma, osteoblastoma, aneurysmal bone cyst, giant cell tumor, and osteochondroma. Common malignant primary neo- plasms are chordoma, chondrosarcoma, Ewing sarcoma or primitive neuroectodermal Keywords tumor, and osteosarcoma. Although plain radiographs may be useful to characterize ► spinal tumor some spinal lesions, magnetic resonance imaging is indispensable to determine the ► extradural tumor extension and the relationship with the spinal canal and nerve roots, and thus determine ► magnetic resonance the plan of management. In this article we review the characteristic imaging features of imaging extradural spinal lesions. Spinal tumors consist of a large spectrum of various histo- Benign Tumors of the Osseous Spine logic entities. Primary spinal tumors may arise from the spinal cord (intraaxial or intramedullary space), the sur- Enostosis rounding leptomeninges (intradural extramedullary space), Enostosis, also called a bone island, is a frequent benign or the extradural soft tissues and bony structures (extra- hamartomatous osseous spinal lesion with a developmental dural space). -

Peripheral Osteoma of the Mandible a Report of Two Cases and Review of Literature
Journal of Research in Medical and Dental Science 2020, Volume 8, Issue 6, Page No: 176-179 Copyright CC BY-NC 4.0 Available Online at: www.jrmds.in eISSN No. 2347-2367: pISSN No. 2347-2545 Peripheral Osteoma of the Mandible a Report of Two Cases and Review of Literature Jawahar Anand*, Anil Kumar Desai, Sayali Desai Department of Oral and Maxillofacial Surgery, Craniofacial Unit and Research Centre, SDM College of Dental Sciences, Dharwad, Karnataka, India ABSTRACT Osteoma is a benign osteogenic tumour, commonly involving the craniofacial bones. It is characterized by excessive proliferation of cortical or cancellous bone. It can be of the central, peripheral or extraskeletal variety. Peripheral osteoma arises from the periosteum and is usually asymptomatic, however, can attain large size in the involved bone. In this paper, we report two cases of peripheral osteoma and review the literature related to the pathological condition. Two patients reported with a chief complaint of asymptomatic slow-growing swelling over the mandibular body region. Radiographic examination revealed a lobulated pedunculated radiopaque mass. It was excised surgically, and no recurrence was noted on follow-up visits. Osteoma involving the jaws is not common and can be associated with Gardner’s syndrome thereby requiring regular follow-up and thorough examination. Surgical excision is the treatment of choice and recurrence is rare. Key words: Peripheral osteoma, Mandibular osteoma, Benign tumour, Osteogenic tumour. HOW TO CITE THIS ARTICLE Review of Literature, J Res Med Dent Sci, 2020, 8 (6): 176-179. : Jawahar Anand, Anil Kumar Desai, Sayali Desai, Peripheral Osteoma of the Mandible a Report of Two Cases and Corresponding author: Jawahar Anand purpose of this paper is to report two cases of e-mail: [email protected] osteomas involving the mandibular body and Received: 27/08/2020 present a review of the literature. -
Epiphyseal Chondromyxoid Fibroma with Prominent Adipose Tissue: an Unusual Radiologic and Histologic Presentation
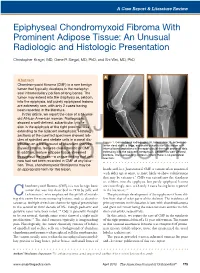
A Case Report & Literature Review Epiphyseal Chondromyxoid Fibroma With Prominent Adipose Tissue: An Unusual Radiologic and Histologic Presentation Christopher Kragel, MD, Gene P. Siegal, MD, PhD, and Shi Wei, MD, PhD A B Abstract Chondromyxoid fibroma (CMF) is a rare benign tumor that typically develops in the metaphy- seal intramedullary portion of long bones. The tumor may extend into the diaphysis or, seldom, into the epiphysis, but purely epiphyseal lesions are extremely rare, with only 2 cases having been reported in the literature. In this article, we report the case of a 51-year- old African American woman. Radiographs showed a well-defined, subarticular lytic le- sion in the epiphysis of the right proximal tibia extending to the adjacent metaphysis.AJO Histologic sections of the curetted specimen showed lob- ules of spindled and stellate cells in a zonal dis- Figure 1. Conventional radiographs (A, lateral view; B, anteropos- tribution on a background of abundant chondro- terior view) show a large, expansile subarticular lytic lesion with myxoid stroma, features characteristic of CMF. internal bony septations in the epiphysis of the right proximal tibia In addition, mature adipose tissue streamed extending into the adjacent metaphysis. Lesion has well-defined borders. The surrounding cortex is intact; there is no periosteal throughout the lesion—a unique finding that until reaction. DOnow had not been recorded NOT in CMF at any loca- COPY tion. Thus, chondromyxoid fibrolipoma may be an appropriate term for this lesion. hands and -

FOS Expression in Osteoid Osteoma and Osteoblastoma
Amary et al FOS Expression in Osteoid Osteoma and Osteoblastoma FOS Expression in Osteoid Osteoma and Osteoblastoma A Valuable Ancillary Diagnostic Tool Fernanda Amary, MD, PhD,*† Eva Markert, MD,* Fitim Berisha, MSc,* Hongtao Ye, PhD,* Craig Gerrand, MD,* Paul Cool, MD,‡ Roberto Tirabosco, MD,* Daniel Lindsay, MD,* Nischalan Pillay, MD, PhD,*† Paul O’Donnell, MD,* Daniel Baumhoer, MD, PhD,§ and Adrienne M. Flanagan, MD, PhD*† light of morphologic, clinical, and radiologic features. Abstract: Osteoblastoma and osteoid osteoma together are the Key Words: bone tumor, osteoblastoma, osteoid osteoma, most frequent benign bone-forming tumor, arbitrarily separated by FOS, c-FOS, immunohistochemistry, FISH, osteosarcoma size. In some instances, it can be difficult to differentiate osteo- blastoma from osteosarcoma. Following our recent description of Osteoid osteoma and osteoblastoma together are FOS gene rearrangement in these tumors, the aim of this study is to the most common bone-forming tumors. Arbitrarily evaluate the value of immunohistochemistry in osteoid osteoma, separated by size, osteoid osteoma is defined as measuring osteoblastoma, and osteosarcoma for diagnostic purposes. A total <2 cm diameter, and usually with a classic clinical pre- of 337 cases were tested with antibodies against c-FOS: 84 osteo- sentation of nocturnal pain that is relieved with the use of blastomas, 33 osteoid osteomas, 215 osteosarcomas, and 5 samples non–steroidal anti-inflammatory drugs.1,2 Osteoblastoma of reactive new bone formation. In all, 83% of osteoblastomas and is less common than osteoid osteoma and represents 1% of 73% of osteoid osteoma showed significant expression of c-FOS in all benign bone tumors, being by definition 2 cm or more 3,4 the osteoblastic tumor cell component. -
Musculoskeletal Tumor Pathology
is pleased to announce: October 22-24, 2015 The 6th Joint MSK / HSS / IOR Course on Musculoskeletal Tumor Pathology PRESENTED IN COLLABORATION WITH CONFERENCE LOCATION MEMORIAL SLOAN KETTERING CANCER CENTER ZUCKERMAN RESEARCH CENTER NEW YORK To register or for more information, please go to: www.mskcc.org/musculoskeletal The 6th Joint MSK / HSS / IOR Course on Musculoskeletal Tumor Pathology 2015 COURSE OVERVIEW This course is designed to give a current review of musculoskeletal tumor pathology to orthopaedic surgeons, radiation oncologists, medical oncologists, radiologists and pathologists. TOPICS BENIGN NON MALIGNANT TUMORS VARIOUS SURGICAL AND Adamantinoma Biological prognostic SURGICAL LESIONS Chondrosarcomas and therapeutic Aneurysmal bone cyst markers Chordoma Bone cyst Bone allografts Ewing’s sarcoma Chondromyxoid in skeletal fibroma Lymphoma reconstruction Chondroblastoma Myeloma Chemotherapy issues and future trends Chondromas Osteosarcomas Integrated treatment of Desmoplastic fibroma Secondary malignancies soft tissue sarcomas Eosinophilic granuloma Spindle and Reconstruction in pleomorphic children Fibrous dysplasia sarcomas Giant cell tumor Staging and biopsy and Vascular tumors margins Histiocytic fibroma Bone Metastases Surgical principles of Myositis ossificans benign lesions Osteoblastoma SOFT TISSUE TUMORS Surgical treatment of Osteochondromas Lipoma and other spine tumors Osteoid osteoma benign soft tissue tumors SPECIAL SESSIONS Liposarcoma Basic Research Fibrosarcoma Molecular Biology in the Malignant fibrous Diagnosis -

Bone Tumors Amber Kazi PGY-1 3/19/20 HPI: a Previously Healthy 7 Year Old Female Comes to Your Office for Left Leg Pain
Pediatric Bone Tumors Amber Kazi PGY-1 3/19/20 HPI: A previously healthy 7 year old female comes to your office for left leg pain. Onset: Yesterday on the playground,she was sitting on the stairs and another kid fell on top of her. She developed a lot of redness and pain close to her knee, which Mom said was more than expected given the impact. Because she was limping for a day, Mom brought her in. Location: Left femur, closer to knee Duration: Constant since yesterday Characteristics: Redness/swelling above knee joint Associated symptoms: Besides the pain and swelling, Mom denies weight loss, night sweats, fevers, neurologic changes in numbness/tingling. Able to limp. Resolving factors: none Timing: constant Severity: Limping with pain On exam, you palpate a small mass over left femur with some tenderness to palpation. She also has an antalgic gait. Otherwise normal exam. What would you like to do next? Your imaging you asked for…. Your X-ray of Probably her left leg prompted that looks like CT that looks this... like this... Bony Masses in Kids The Presentation: ● Bony tumors usually present as an incidental finding ● Your symptoms can include: pain, swelling, refusal to use part, decreased range of motion, or a hard/fixed mass ○ Malignant? Tend to be more painful, with pain present while resting at night without relief from NSAID’s ○ HOWEVER: Your benign tumors can also have some similar presentations. The Workup Consider this work up from the AAP as a good starting point. Would you want labs? You could find an elevated LDH, alkaline phosphatase, and ESR that can help with diagnosis, but a picture is worth a thousand words. -

Osteoid Osteoma: Multimodality Imaging with Focus on Hybrid Imaging
European Journal of Nuclear Medicine and Molecular Imaging (2019) 46:1019–1036 https://doi.org/10.1007/s00259-018-4181-2 REVIEW ARTICLE Osteoid osteoma: multimodality imaging with focus on hybrid imaging Ujwal Bhure1 & Justus E. Roos1 & Klaus Strobel1 Received: 1 June 2018 /Accepted: 25 September 2018 /Published online: 19 October 2018 # Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Osteoid osteoma is a painful, benign, osteoblastic lesion that occurs in younger patients and affects the extremities or the axial skeleton. While plain film findings may suggest the diagnosis, in complex anatomical regions such as the spine, pelvis, wrist and foot advanced imaging modalities are often required. A typical nidus surrounded by sclerosis or cortical thickening characterizes osteoid osteoma on plain radiography and CT. MR is the cross-sectional imaging modality of choice for most musculoskeletal disorders. Unfortunately, extensive accompanying bone marrow oedema, soft-tissue alterations, difficulty detecting the nidus, and lesion locations close to a joint (with reactive arthritis) may make a confident diagnosis of osteoid osteoma by MR imaging difficult. Hybrid imaging with bone- seeking tracers such as SPECT/CT with 99mTc-labelled bisphosphonates or PET/CT with 18F-labelled sodium fluoride (18F-NaF) combines high radionuclide uptake with morphological details and provides accurate diagnosis of osteoid osteoma and additional information for treatment planning. FDG is not the recommended PET tracer because osteoid osteoma is normally FDG-negative, although some osteoid osteomas may show increased FDG uptake. Osteoblastoma, Brodie’s abscess and stress fractures may mimic osteoid osteoma on imaging and clinical presenta- tion. Once identified as the pain generator, destruction of the osteoid osteoma nidus by ablation or resection techniques usually leads to complete healing.