Eating Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

First Episode Psychosis an Information Guide Revised Edition
First episode psychosis An information guide revised edition Sarah Bromley, OT Reg (Ont) Monica Choi, MD, FRCPC Sabiha Faruqui, MSc (OT) i First episode psychosis An information guide Sarah Bromley, OT Reg (Ont) Monica Choi, MD, FRCPC Sabiha Faruqui, MSc (OT) A Pan American Health Organization / World Health Organization Collaborating Centre ii Library and Archives Canada Cataloguing in Publication Bromley, Sarah, 1969-, author First episode psychosis : an information guide : a guide for people with psychosis and their families / Sarah Bromley, OT Reg (Ont), Monica Choi, MD, Sabiha Faruqui, MSc (OT). -- Revised edition. Revised edition of: First episode psychosis / Donna Czuchta, Kathryn Ryan. 1999. Includes bibliographical references. Issued in print and electronic formats. ISBN 978-1-77052-595-5 (PRINT).--ISBN 978-1-77052-596-2 (PDF).-- ISBN 978-1-77052-597-9 (HTML).--ISBN 978-1-77052-598-6 (ePUB).-- ISBN 978-1-77114-224-3 (Kindle) 1. Psychoses--Popular works. I. Choi, Monica Arrina, 1978-, author II. Faruqui, Sabiha, 1983-, author III. Centre for Addiction and Mental Health, issuing body IV. Title. RC512.B76 2015 616.89 C2015-901241-4 C2015-901242-2 Printed in Canada Copyright © 1999, 2007, 2015 Centre for Addiction and Mental Health No part of this work may be reproduced or transmitted in any form or by any means electronic or mechanical, including photocopying and recording, or by any information storage and retrieval system without written permission from the publisher—except for a brief quotation (not to exceed 200 words) in a review or professional work. This publication may be available in other formats. For information about alterna- tive formats or other CAMH publications, or to place an order, please contact Sales and Distribution: Toll-free: 1 800 661-1111 Toronto: 416 595-6059 E-mail: [email protected] Online store: http://store.camh.ca Website: www.camh.ca Disponible en français sous le titre : Le premier épisode psychotique : Guide pour les personnes atteintes de psychose et leur famille This guide was produced by CAMH Publications. -

Resource Document on Social Determinants of Health
APA Resource Document Resource Document on Social Determinants of Health Approved by the Joint Reference Committee, June 2020 "The findings, opinions, and conclusions of this report do not necessarily represent the views of the officers, trustees, or all members of the American Psychiatric Association. Views expressed are those of the authors." —APA Operations Manual. Prepared by Ole Thienhaus, MD, MBA (Chair), Laura Halpin, MD, PhD, Kunmi Sobowale, MD, Robert Trestman, PhD, MD Preamble: The relevance of social and structural factors (see Appendix 1) to health, quality of life, and life expectancy has been amply documented and extends to mental health. Pertinent variables include the following (Compton & Shim, 2015): • Discrimination, racism, and social exclusion • Adverse early life experiences • Poor education • Unemployment, underemployment, and job insecurity • Income inequality • Poverty • Neighborhood deprivation • Food insecurity • Poor housing quality and housing instability • Poor access to mental health care All of these variables impede access to care, which is critical to individual health, and the attainment of social equity. These are essential to the pursuit of happiness, described in this country’s founding document as an “inalienable right.” It is from this that our profession derives its duty to address the social determinants of health. A. Overview: Why Social Determinants of Health (SDOH) Matter in Mental Health Social determinants of health describe “the causes of the causes” of poor health: the conditions in which individuals are “born, grow, live, work, and age” that contribute to the development of both physical and psychiatric pathology over the course of one’s life (Sederer, 2016). The World Health Organization defines mental health as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community” (World Health Organization, 2014). -
The Impact of Trauma and Attachment on Eating Disorder Symptomology
Loma Linda University TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works Loma Linda University Electronic Theses, Dissertations & Projects 9-2014 The mpI act of Trauma and Attachment on Eating Disorder Symptomology Julie A. Hewett Follow this and additional works at: http://scholarsrepository.llu.edu/etd Part of the Clinical Psychology Commons Recommended Citation Hewett, Julie A., "The mpI act of Trauma and Attachment on Eating Disorder Symptomology" (2014). Loma Linda University Electronic Theses, Dissertations & Projects. 210. http://scholarsrepository.llu.edu/etd/210 This Dissertation is brought to you for free and open access by TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works. It has been accepted for inclusion in Loma Linda University Electronic Theses, Dissertations & Projects by an authorized administrator of TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works. For more information, please contact [email protected]. LOMA LINDA UNIVERSITY School of Behavioral Health in conjunction with the Faculty of Graduate Studies _______________________ The Impact of Trauma and Attachment on Eating Disorder Symptomology by Julie A. Hewett _______________________ A Dissertation submitted in partial satisfaction of the requirements for the degree Doctor of Philosophy in Clinical Psychology _______________________ September 2014 © 2014 Julie A. Hewett All Rights Reserved Each person whose signature appears below certifies that this dissertation in his/her opinion is adequate, in scope and quality, as a dissertation for the degree Doctor of Philosophy. , Chairperson Sylvia Herbozo, Assistant Professor of Psychology Jeffrey Mar, Assistant Clinical Professor, Psychiatry, School of Medicine Jason Owen, Associate Professor of Psychology David Vermeersch, Professor of Psychology iii ACKNOWLEDGEMENTS I would like to express my deepest gratitude to Dr. -
Spanish Clinical Language and Resource Guide
SPANISH CLINICAL LANGUAGE AND RESOURCE GUIDE The Spanish Clinical Language and Resource Guide has been created to enhance public access to information about mental health services and other human service resources available to Spanish-speaking residents of Hennepin County and the Twin Cities metro area. While every effort is made to ensure the accuracy of the information, we make no guarantees. The inclusion of an organization or service does not imply an endorsement of the organization or service, nor does exclusion imply disapproval. Under no circumstances shall Washburn Center for Children or its employees be liable for any direct, indirect, incidental, special, punitive, or consequential damages which may result in any way from your use of the information included in the Spanish Clinical Language and Resource Guide. Acknowledgements February 2015 In 2012, Washburn Center for Children, Kente Circle, and Centro collaborated on a grant proposal to obtain funding from the Hennepin County Children’s Mental Health Collaborative to help the agencies improve cultural competence in services to various client populations, including Spanish-speaking families. These funds allowed Washburn Center’s existing Spanish-speaking Provider Group to build connections with over 60 bilingual, culturally responsive mental health providers from numerous Twin Cities mental health agencies and private practices. This expanded group, called the Hennepin County Spanish-speaking Provider Consortium, meets six times a year for population-specific trainings, clinical and language peer consultation, and resource sharing. Under the grant, Washburn Center’s Spanish-speaking Provider Group agreed to compile a clinical language guide, meant to capture and expand on our group’s “¿Cómo se dice…?” conversations. -

Posttraumatic Stress Disorder in Anorexia Nervosa
NIH Public Access Author Manuscript Psychosom Med. Author manuscript; available in PMC 2012 July 1. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Psychosom Med. 2011 July ; 73(6): 491±497. doi:10.1097/PSY.0b013e31822232bb. Post traumatic stress disorder in anorexia nervosa Mae Lynn Reyes-Rodríguez, Ph.D.1, Ann Von Holle, M.S.1, T. Frances Ulman, Ph.D.1, Laura M. Thornton, Ph.D.1, Kelly L. Klump, Ph.D.2, Harry Brandt, M.D.3, Steve Crawford, M.D.3, Manfred M. Fichter, M.D.4, Katherine A. Halmi, M.D.5, Thomas Huber, M.D.6, Craig Johnson, Ph.D.7, Ian Jones, M.D.8, Allan S. Kaplan, M.D., F.R.C.P. (C)9,10,11, James E. Mitchell, M.D. 12, Michael Strober, Ph.D.13, Janet Treasure, M.D.14, D. Blake Woodside, M.D.9,11, Wade H. Berrettini, M.D.15, Walter H. Kaye, M.D.16, and Cynthia M. Bulik, Ph.D.1,17 1 Department of Psychiatry, University of North Carolina, Chapel Hill, NC 2 Department of Psychology, Michigan State University, East Lansing, MI 3 Department of Psychiatry, University of Maryland School of Medicine, Baltimore, MD 4 Klinik Roseneck, Hospital for Behavioral Medicine, Prien and University of Munich (LMU), Munich, Germany 5 New York Presbyterian Hospital-Westchester Division, Weill Medical College of Cornell University, White Plains, NY 6 Klinik am Korso, Bad Oeynhausen, Germany 7 Eating Recovery Center, Denver, CO 8 Department of Psychological Medicine, University of Birmingham, United Kingdom 9 Department of Psychiatry, The Toronto Hospital, Toronto, Canada 10 Center for -

Eating Disorders: About More Than Food
Eating Disorders: About More Than Food Has your urge to eat less or more food spiraled out of control? Are you overly concerned about your outward appearance? If so, you may have an eating disorder. National Institute of Mental Health What are eating disorders? Eating disorders are serious medical illnesses marked by severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may be signs of an eating disorder. These disorders can affect a person’s physical and mental health; in some cases, they can be life-threatening. But eating disorders can be treated. Learning more about them can help you spot the warning signs and seek treatment early. Remember: Eating disorders are not a lifestyle choice. They are biologically-influenced medical illnesses. Who is at risk for eating disorders? Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Although eating disorders often appear during the teen years or young adulthood, they may also develop during childhood or later in life (40 years and older). Remember: People with eating disorders may appear healthy, yet be extremely ill. The exact cause of eating disorders is not fully understood, but research suggests a combination of genetic, biological, behavioral, psychological, and social factors can raise a person’s risk. What are the common types of eating disorders? Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. If you or someone you know experiences the symptoms listed below, it could be a sign of an eating disorder—call a health provider right away for help. -

Neural Correlates and Treatments Binge Eating Disorder
Running head: Binge Eating Disorder: Neural correlates and treatments Binge Eating Disorder: Neural correlates and treatments Bachelor Degree Project in Cognitive Neuroscience Basic level 22.5 ECTS Spring term 2019 Malin Brundin Supervisor: Paavo Pylkkänen Examiner: Stefan Berglund Running head: Binge Eating Disorder: Neural correlates and treatments Abstract Binge eating disorder (BED) is the most prevalent of all eating disorders and is characterized by recurrent episodes of eating a large amount of food in the absence of control. There have been various kinds of research of BED, but the phenomenon remains poorly understood. This thesis reviews the results of research on BED to provide a synthetic view of the current general understanding on BED, as well as the neural correlates of the disorder and treatments. Research has so far identified several risk factors that may underlie the onset and maintenance of the disorder, such as emotion regulation deficits and body shape and weight concerns. However, neuroscientific research suggests that BED may characterize as an impulsive/compulsive disorder, with altered reward sensitivity and increased attentional biases towards food cues, as well as cognitive dysfunctions due to alterations in prefrontal, insular, and orbitofrontal cortices and the striatum. The same alterations as in addictive disorders. Genetic and animal studies have found changes in dopaminergic and opioidergic systems, which may contribute to the severities of the disorder. Research investigating neuroimaging and neuromodulation approaches as neural treatment, suggests that these are innovative tools that may modulate food-related reward processes and thereby suppress the binges. In order to predict treatment outcomes of BED, future studies need to further examine emotion regulation and the genetics of BED, the altered neurocircuitry of the disorder, as well as the role of neurotransmission networks relatedness to binge eating behavior. -
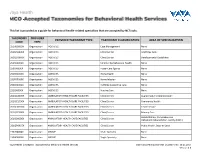
This List Is Provided As a Guide for Behavioral Health-Related Specialties That Are Accepted by Nctracks
This list is provided as a guide for behavioral health-related specialties that are accepted by NCTracks. TAXONOMY PROVIDER PROVIDER TAXONOMY TYPE TAXONOMY CLASSIFICATION AREA OF SPECIALIZATION CODE TYPE 251B00000X Organization AGENCIES Case Management None 261QA0600X Organization AGENCIES Clinic/Center Adult Day Care 261QD1600X Organization AGENCIES Clinic/Center Developmental Disabilities 251S00000X Organization AGENCIES Community/Behavioral Health None 253J00000X Organization AGENCIES Foster Care Agency None 251E00000X Organization AGENCIES Home Health None 251F00000X Organization AGENCIES Home Infusion None 253Z00000X Organization AGENCIES In-Home Supportive Care None 251J00000X Organization AGENCIES Nursing Care None 261QA3000X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Augmentative Communication 261QC1500X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Community Health 261QH0100X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Health Service 261QP2300X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Primary Care Rehabilitation, Comprehensive 261Q00000X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Outpatient Rehabilitation Facility (CORF) 261QP0905X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Public Health, State or Local 193200000X Organization GROUP Multi-Specialty None 193400000X Organization GROUP Single-Specialty None Vaya Health | Accepted Taxonomies for Behavioral Health Services Claims and Reimbursement | Content rev. 10.01.2017 Version -

Eating Disorders
Eating Disorders NDSCS Counseling Services hopes the following information will help you gain a better understanding of eating disorders. If you believe you or someone you know is experiencing related concerns and would like to visit with a counselor, please call NDSCS Counseling Services for an appointment - 701.671.2286. Definition There is a commonly held view that eating disorders are a lifestyle choice. Eating disorders are actually serious and often fatal illnesses that cause severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may also signal an eating disorder. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. Signs and Symptoms Anorexia nervosa People with anorexia nervosa may see themselves as overweight, even when they are dangerously underweight. People with anorexia nervosa typically weigh themselves repeatedly, severely restrict the amount of food they eat, and eat very small quantities of only certain foods. Anorexia nervosa has the highest mortality rate of any mental disorder. While many young women and men with this disorder die from complications associated with starvation, others die of suicide. In women, suicide is much more common in those with anorexia than with most other mental disorders. Symptoms include: • Extremely restricted eating • Extreme thinness (emaciation) • A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight • Intense fear of gaining weight • Distorted body image, a self-esteem -

Understanding Mental Health
UNDERSTANDING MENTAL HEALTH WHAT IS MENTAL HEALTH? Our mental health directly influences how we think, feel and act: it also affects our physical health. Work, in fact, is actually one of the best things for protecting our mental health, but it can also adversely affect it. Good mental health and well-being is not an on-off A person’s mental health moves back and forth along this range during experience. We can all have days, weeks or months their lifetime, in response to different stressors and circumstances. At where we feel resilient, strong and optimistic, the green end of the continuum, people are well; showing resilience regardless of events or situations. Often that can and high levels of wellbeing. Moving into the yellow area, people be mixed with or shift to a very different set of may start to have difficulty coping. In the orange area, people have thoughts, feelings and behaviours; or not feeling more difficulty coping and symptoms may increase in severity and resilient and optimistic in just one or two areas of frequency. At the red end of the continuum, people are likely to be our life. For about twenty-five per cent of us, that experiencing severe symptoms and may be at risk of self-harm or may shift to having a significant impact on how suicide. we think, feel and act in many parts of our lives, including relationships, experiences at work, sense of connection to peer groups and our personal sense of worth, physical health and motivation. This could lead to us developing a mental health condition such as anxiety, depression, substance misuse. -

Eating Disorders and Sexual Function Reviewed: a Trans-Diagnostic, Dimensional Perspective
Current Sexual Health Reports (2020) 12:1–14 https://doi.org/10.1007/s11930-020-00236-w CLINICAL THERAPEUTICS (B MCCARTHY, R SEGRAVES AND R BALON, SECTION EDITORS) Eating Disorders and Sexual Function Reviewed: A Trans-diagnostic, Dimensional Perspective Cara R. Dunkley1,2 & Yana Svatko1 & Lori A. Brotto2,3 Published online: 18 January 2020 # Springer Science+Business Media, LLC, part of Springer Nature 2020 Abstract Purpose of Review Clinical observation and a growing body of empirical research point to an association between disordered eating and sexual function difficulties. The present review identifies and connects the current knowledge on sexual dysfunction in the eating disorders, and provides a theoretical framework for conceptualizing the association between these important health conditions. Recent Findings Research on sexuality and eating pathology has focused on clinical samples of women with anorexia nervosa (AN) and bulimia nervosa (BN). All aspects of sexual response can be impacted in women with an eating disorder, with sexual function in women with AN appearing to be more compromised than in women with BN. Research of this nature is extremely limited with respect to BED, non-clinical samples, men, and individuals with non-binary gender identities. Summary Sexuality should be examined and addressed within the context of eating disorder treatment. Sexual dysfunction and eating disorders, along with commonly comorbid disorders of anxiety and mood, can be seen as separate but frequently overlapping manifestations of internalizing psychopathology. Psychological, developmental, sociocultural, etiological, and bio- physical factors likely represent risk and maintenance factors for internalizing disorders. A dimensional, trans-diagnostic ap- proach to disordered eating and sexuality has promising implications for future research and clinical interventions. -

A Case–Control Study Investigating Food Addiction in Parkinson Patients Ingrid De Chazeron1*, F
www.nature.com/scientificreports OPEN A case–control study investigating food addiction in Parkinson patients Ingrid de Chazeron1*, F. Durif2, C. Lambert3, I. Chereau‑Boudet1, M. L. Fantini4, A. Marques2, P. Derost2, B. Debilly2, G. Brousse1, Y. Boirie5,6 & P. M. Llorca1,2,3,4,5,6 Eating disorders (EDs) in patients with Parkinson’s disease (PD) are mainly described through impulse control disorders but represent one end of the spectrum of food addiction (FA). Although not formally recognized by DSM‑5, FA is well described in the literature on animal models and humans, but data on prevalence and risk factors compared with healthy controls (HCs) are lacking. We conducted a cross‑ sectional study including 200 patients with PD and 200 age‑ and gender‑matched HCs. Characteristics including clinical data (features of PD/current medication) were collected. FA was rated using DSM‑5 criteria and the Questionnaire on Eating and Weight Patterns‑Revised (QEWP‑R). Patients with PD had more EDs compared to HCs (27.0% vs. 13.0%, respectively, p < 0.001). They mainly had FA (24.5% vs. 12.0%, p = 0.001) and night eating syndrome (7.0% vs. 2.5% p = 0.03). In PD patients, FA was associated with female gender (p = 0.04) and impulsivity (higher attentional non‑planning factor) but not with the dose or class of dopaminergic therapy. Vigilance is necessary, especially for PD women and in patients with specifc impulsive personality traits. Counterintuitively, agonist dopaminergic treatment should not be used as an indication for screening FA in patients with PD. In Parkinson’s disease (PD), compulsive eating is part of the spectrum of impulse control disorders (ICDs) that also include pathologic gambling, compulsive buying and hypersexuality1.