Treatment of Alcoholic Hepatitis: Is This a “Dead-End”?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(Trental) Does Not Inhibit Dipyridamole-Induced Coronary Hyperemia: Implications for Dipyridamole-Thaffium-20 1 Myocardial Imaging
Pentoxifyffine (Trental) Does Not Inhibit Dipyridamole-Induced Coronary Hyperemia: Implications for Dipyridamole-Thaffium-20 1 Myocardial Imaging Kenneth A. Brown and Bryan K. Slinker Cardiology Unit ofihe University of Vermont College ofMedicine, Burlington, Vermont been found to be efficacious in the treatment of inter Dipyndamole-thallium-201imagingis often performedin mittent claudication because of its unique hemorrheo patientsunableto exercisebecauseof peripheralvascular logic effects (9). Thus, many patients with peripheral disease.Manyof these patientsare taking pentoxifylline vascular disease who undergo dipyridamole-thallium (Trental),a methylxanthinederivativewhichmayimprove 201 imaging may be taking pentoxifylline at the time intermittent claudication. Whether pentoxifylline inhibits di of their study. Although in vitro data from rat fat cells pyndamole-inducedcoronaryhyperamialike other math and hippocampal slices suggest that pentoxifylline is a ylxanthinas such as theophyllina and should be stopped much weaker adenosine antagonist than theophylline prior to dipyndamole-thallium-201 imaging is unknown. (7), it is not known whetherpentoxifylline significantly Therefore,we studiedthe hyperemicresponseto dipyn damolein sevenopen-chestanesthetizeddogs after pre inhibits dipyridamole-induced coronary hyperemia in treatmentwith either pantoxifylline(0, 7.5, or i 5 mg/kg vivo and should, therefore, be stopped prior to dipyri i.v.) or theophyllina(3 mg/kg i.v.). Baseline circumflex damole-thallium-20l imaging. Hence, we studied the -

TRENTAL (Pentoxifylline) Should Be Used During Pregnancy Only If the Potential Benefit Justifies the Potential Risk to the Fetus
TRENTAL® (pentoxifylline) Extended-Release Tablets, 400 mg DESCRIPTION TRENTAL® (pentoxifylline) extended-release tablets for oral administration contain 400 mg of the active drug and the following inactive ingredients: FD&C Red No. 3, hypromellose USP, magnesium stearate NF, polyethylene glycol NF, povidone USP, talc USP, titanium dioxide USP, and hydroxyethyl cellulose USP in an extended-release formulation. TRENTAL is a tri-substituted xanthine derivative designated chemically as 1-(5-oxohexyl)-3, 7 dimethylxanthine that, unlike theophylline, is a hemorrheologic agent, i.e. an agent that affects blood viscosity. Pentoxifylline is soluble in water and ethanol, and sparingly soluble in toluene. The CAS Registry Number is 6493-05-6. The chemical structure is: CLINICAL PHARMACOLOGY Mode of Action Pentoxifylline and its metabolites improve the flow properties of blood by decreasing its viscosity. In patients with chronic peripheral arterial disease, this increases blood flow to the affected microcirculation and enhances tissue oxygenation. The precise mode of action of pentoxifylline and the sequence of events leading to clinical improvement are still to be defined. Pentoxifylline administration has been shown to produce dose-related hemorrheologic effects, lowering blood viscosity, and improving erythrocyte flexibility. Leukocyte properties of hemorrheologic importance have been modified in animal and in vitro human studies. Pentoxifylline has been shown to increase leukocyte deformability and to inhibit neutrophil adhesion and activation. Tissue oxygen levels have been shown to be significantly increased by therapeutic doses of pentoxifylline in patients with peripheral arterial disease. Pharmacokinetics and Metabolism After oral administration in aqueous solution pentoxifylline is almost completely absorbed. It undergoes a first-pass effect and the various metabolites appear in plasma very soon after dosing. -

(12) Patent Application Publication (10) Pub. No.: US 2005/0142174A1 Assmus Et Al
US 2005O142174A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2005/0142174A1 ASSmus et al. (43) Pub. Date: Jun. 30, 2005 (54) ADHESIVE AND BINDING AGENT FOR (30) Foreign Application Priority Data DERMAL OR TRANSIDERMAL TREATMENT SYSTEMS Jan. 9, 2002 (DE)........................................ 10200578.8 (75) Inventors: Manfred Assmus, Bickenbach (DE); Publication Classification Erna Roth, Darmstadt (DE), Antoni (51) Int. Cl." .......................... A61K 31/485; A61 K 9/70 Boix, St. Joan (ES); Isabel Reig, St. (52) U.S. Cl. ............................................ 424/449; 514/282 Joan Despi (ES) s (57) ABSTRACT Correspondence Address: The invention relates to an adhesive and binding agent for OBLON, SPIVAK, MCCLELLAND, MAIER & dermal or transdermal treatment Systems, said agent con NEUSTADT, P.C. taining (a) a (meth)acrylate copolymer consisting of radi 1940 DUKE STREET cally polymerised C-sb>1</sb>to C-sb>4</sb>alkyl esters ALEXANDRIA, VA 22314 (US) of acrylic or methacrylic acid and (meth)acrylate monomers having a cationic ammonium group in the alkyl radical; (b) between 0.1 and 45 wt.%, in relation to (a), of an organic (73) Assignee: Roehm GMBH & Co. KG dicarboxylic or tricarboxylic acid, or of acrylate or (meth )acrylate polymers or copolymers containing acid groups; (21) Appl. No.: 10/499,818 (c) a skin penetration enhancer; and (d) optionally a phar maceutical active ingredient, a Softener and/or at least one (22) PCT Filed: Dec. 19, 2002 Standard addition agent. The inventive adhesive and binding agent is characterised in that the penetration enhancer (c) is (86) PCT No.: PCT/EPO2/14556 an alcohol comprising between 10 and 12 carbon atoms. -

1 Package Leaflet: Information for the Patient Pentoxifyllin-Tchaikapharma
Package Leaflet: Information for the patient Pentoxifyllin-Tchaikapharma 400 mg prolonged-release tablets pentoxifylline Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor or pharmacist. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours. - If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section4. What is in this leaflet: 1. What Pentoxifyllin-Tchaikapharma is and what it is used for 2. What you need to know before you take Pentoxifyllin-Tchaikapharma 3. How to take Pentoxifyllin-Tchaikapharma 4. Possible side effects 5. How to store Pentoxifyllin-Tchaikapharma 6. Contents of the pack and other information 1. What Pentoxifyllin-Tchaikapharma is and what it is used for Pentoxifylline acts on the viscosity of the blood by reducing the binding of its components and increases the deformability of erythrocytes. This has a beneficial effect on blood circulation in diseases of the peripheral and cerebral arteries. This has a beneficial effect on blood circulation in diseases of the peripheral and cerebral arteries. This has a beneficial effect on the circulatory system diseases of the peripheral and cerebral arteries. Improves the blood supply to small blood vessels and the supply of tissues with oxygen. This medicine is used in: - Advanced disorders of peripheral arterial circulation of the limbs caused by atherosclerosis and diabetes and vascular spasms (intermittent claudication, diabetic macro- and microangiopathy, Raynaud's syndrome); - Diseases associated with venous circulation disorders; - Treatment of impaired blood supply to the brain and eyes. -

Methylxanthines and Neurodegenerative Diseases: an Update
nutrients Review Methylxanthines and Neurodegenerative Diseases: An Update Daniel Janitschke 1,† , Anna A. Lauer 1,†, Cornel M. Bachmann 1, Heike S. Grimm 1, Tobias Hartmann 1,2 and Marcus O. W. Grimm 1,2,* 1 Experimental Neurology, Saarland University, 66421 Homburg/Saar, Germany; [email protected] (D.J.); [email protected] (A.A.L.); [email protected] (C.M.B.); [email protected] (H.S.G.); [email protected] (T.H.) 2 Deutsches Institut für DemenzPrävention (DIDP), Saarland University, 66421 Homburg/Saar, Germany * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: Methylxanthines (MTX) are purine derived xanthine derivatives. Whereas naturally occurring methylxanthines like caffeine, theophylline or theobromine are widely consumed in food, several synthetic but also non-synthetic methylxanthines are used as pharmaceuticals, in particular in treating airway constrictions. Besides the well-established bronchoprotective effects, methylxanthines are also known to have anti-inflammatory and anti-oxidative properties, mediate changes in lipid homeostasis and have neuroprotective effects. Known molecular mechanisms include adenosine receptor antagonism, phosphodiesterase inhibition, effects on the cholinergic system, wnt signaling, histone deacetylase activation and gene regulation. By affecting several pathways associated with neurodegenerative diseases via different pleiotropic mechanisms and due to its moderate side effects, intake of methylxanthines have been suggested to be an interesting approach in dealing with neurodegeneration. Especially in the past years, the impact of methylxanthines in neurodegenerative diseases has been extensively studied and several new aspects have been elucidated. In this review Citation: Janitschke, D.; Lauer, A.A.; Bachmann, C.M.; Grimm, H.S.; we summarize the findings of methylxanthines linked to Alzheimer´s disease, Parkinson’s disease Hartmann, T.; Grimm, M.O.W. -
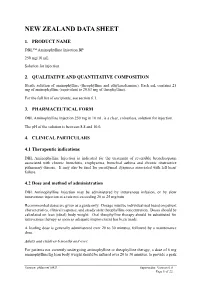
Data Sheet Template
NEW ZEALAND DATA SHEET 1. PRODUCT NAME DBL™ Aminophylline Injection BP 250 mg/10 mL Solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Sterile solution of aminophylline (theophylline and ethylenediamine). Each mL contains 25 mg of aminophylline (equivalent to 20.63 mg of theophylline). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM DBL Aminophylline Injection 250 mg in 10 mL is a clear, colourless, solution for injection. The pH of the solution is between 8.8 and 10.0. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications DBL Aminophylline Injection is indicated for the treatment of reversible bronchospasm associated with chronic bronchitis, emphysema, bronchial asthma and chronic obstructive pulmonary disease. It may also be used for paroxysmal dyspnoea associated with left heart failure. 4.2 Dose and method of administration DBL Aminophylline Injection may be administered by intravenous infusion, or by slow intravenous injection at a rate not exceeding 20 to 25 mg/min. Recommended doses are given as a guide only. Dosage must be individualised based on patient characteristics, clinical response, and steady state theophylline concentration. Doses should be calculated on lean (ideal) body weight. Oral theophylline therapy should be substituted for intravenous therapy as soon as adequate improvement has been made. A loading dose is generally administered over 20 to 30 minutes, followed by a maintenance dose. Adults and children 6 months and over: For patients not currently undergoing aminophylline or theophylline therapy, a dose of 6 mg aminophylline/kg lean body weight should be infused over 20 to 30 minutes, to provide a peak Version: pfdamini10421 Supercedes: Version 6.0 Page 1 of 22 serum theophylline concentration of approximately 10 microgram/mL (55 micromole/L). -

1 Original Article 1 Modulatory Effects of Caffeine and Pentoxifylline On
Modulatory Effects of Caffeine and Pentoxifylline on Aromatic Antibiotics: A Role for Heterocomplex Formation Anna Woziwodzka ( [email protected] ) Laboratory of Biophysics, Intercollegiate Faculty of Biotechnology University of Gdansk and Medical University of Gdansk, Gdansk, Poland Marta Krychowiak-Maśnicka Laboratory of Biologically Active Compounds, Intercollegiate Faculty of Biotechnology University of Gdansk and Medical University of Gdansk, Gdansk, Poland Grzegorz Gołuński Laboratory of Biophysics, Intercollegiate Faculty of Biotechnology University of Gdansk and Medical University of Gdansk, Gdansk, Poland Anna Felberg Laboratory of Biophysics, Intercollegiate Faculty of Biotechnology University of Gdansk and Medical University of Gdansk, Gdansk, Poland Agnieszka Borowik Laboratory of Biophysics, Intercollegiate Faculty of Biotechnology University of Gdansk and Medical University of Gdansk, Gdansk, Poland Dariusz Wyrzykowski Department of Inorganic Biological Chemistry, Faculty of Chemistry, University of Gdansk, Gdansk, Poland Jacek Piosik Laboratory of Biophysics, Intercollegiate Faculty of Biotechnology University of Gdansk and Medical University of Gdansk, Gdansk, Poland Research Article Keywords: antibacterial agent, caffeine, ciprooxacin, drug repositioning, tetracycline Posted Date: January 5th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-138878/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Trental® Pentoxifylline Extended Release Tablets USP
For the use only of a Registered Medical Practitioner or a Hospital or a Laboratory This package insert is continually updated. Please read carefully before using a new pack Trental® Pentoxifylline Extended Release Tablets USP DESCRIPTION Active Ingredient Pentoxifylline Therapeutic or Pharmacological Class Haemorheologic agent Pharmaceutical Form(s) Extended-release film coated tablets Composition Trental 400 Each extended-release film coated tablet contains Pentoxifylline B.P. 400 mg Pentoxifylline extended-release tablets U.S.P comply to U.S.P Drug Release Test 2. Indications • Peripheral arterial occlusive disease (PAOD) of arteriosclerotic or diabetic origin (e.g. with intermittent claudication and rest pain). • Trophic lesions (e.g. leg ulcers and gangrene) • Cerebral vascular disease. • Circulatory disturbances of the eye in conjunction with degenerative vascular disorders. DOSAGE AND ADMINISTRATION General In principle, dosage and mode of administration (oral or i.v.) is based on the type and severity of the circulatory disorders and on how the individual patient tolerates the drug. Dosage is generally based on the following guidelines: • PAOD Stage II (intermittent claudication) and circulatory disturbances of the eye; to start treatment or in support of oral therapy It is recommended that an infusion of 100 to 600 mg pentoxifylline be given once or twice daily. It is recommended that pentoxifylline infusion be administered in a suitable infusion solution; depending on the accompanying diseases (e.g. congestive heart failure), it may be necessary to keep the infusion volume small. In such circumstances, in particular, a controlled volume infusion pump may be useful. When low-dose infusion therapy is combined with oral therapy, the recommended total daily dose is 1200 mg pentoxifylline (intravenous plus oral). -

Cytotoxic, Cell Cycle, and Chromosomal Effects of Methylxanthines in Human Tumor Cells Treated with Alkylating Agents1
[CANCER RESEARCH 46, 2463-2467. May 1986] Cytotoxic, Cell Cycle, and Chromosomal Effects of Methylxanthines in Human Tumor Cells Treated with Alkylating Agents1 Howard J. Fingert,2 James D. Chang, and Arthur B. Pardee Surgical Oncology Unit, Massachusetts General Hospital Cancer Center, Boston, Massachusetts 02114 [H. J. F.], and Department of Pharmacology, Harvard Medical School and Division of Cell Growth and Regulation, Dana-Farber Cancer Institute, Boston, Massachusetts 02115 [H. J. F., J. D. C, A. B. P.] ABSTRACT cells to undergo mitosis before the completion of DNA repair (13, 14). The G2 phase of the cell cycle has been generally Human tumor cells, like rodent cells, are sensitive to effects of meth- observed to lengthen in many normal or malignant cells exposed ylxanthines (MEX) on lethality, cell cycle delays, and chromosome aberrations after DNA damage by anticancer drugs. Enhanced cytotox- to radiation, alkylating agents, or other antineoplastic drugs (15-17). According to this model, MEX do not necessarily icity of ;ilk\luting agents was observed when T24 human bladder tumor cells in culture were exposed to nontoxic concentrations of MEX such as inhibit biochemical DNA repair processes per se; instead, they caffeine or pentoxifylline. Tumor cell lethality was increased up to 10- act by reducing time available for repair, possibly through a fold by either caffeine or pentoxifylline (1 HIM) present during the first protein which is altered directly or indirectly by DNA damage cell cycle (16-24 h) after exposure to nitrogen mustard (HN2) or thiotepa. and which controls the transit from G2 to mitosis (14, 15). In Cycloheximide, a protein synthesis inhibitor, abolished the enhanced BHK cells, MEX allowed G2-delayed cells to reach mitosis lethality produced by MEX. -

Potential Role of Methylxanthines As an Adjuvant to COVID-19 Treatment
Potential role of methylxanthines as an adjuvant to COVID-19 treatment: A review of Pentoxifylline and caffeine as the case of any port in the storm Faezeh Monji1, Abrar Siddiquee2, and Farshad Hashemian1 1Faculty of Pharmacy, Tehran Medical Sciences, Islamic Azad University 2Institute of Molecular and Cell Biology (IMCB), Agency for Science, Technology and Research (ASTAR) May 22, 2020 Abstract COVID-19 pandemic presents an unprecedented challenge to identify effective drugs for treatment. Despite multiple clinical trials using different agents, there is still a lack of specific treatment for COVID-19. Having the possible role in suppressing inflammation, immune modulation, antiviral and improving respiratory symptoms, this review discusses the potential role of methylxanthine drugs like pentoxifylline and caffeine in the management of COVID-19 patients. COVID-19 pathogenesis for clinical features like severe pneumonia, acute lung injury (ALI) / acute respiratory distress syndrome (ARDS), and multi-organ failures are excessive inflammation, oxidation, and cytokine storm by the exaggerated immune response. Drugs like pentoxifylline have already shown improvement of the symptoms of ARDS and caffeine has been in clinical use for decades to treat apnea of prematurity (AOP) in preterm infants and improve respiratory function. Both pentoxifylline and caffeine are well-known anti-inflammatory and anti-oxidative molecules that have already shown to suppress Tumor Necrosis Factor (TNF-a) as well as other inflammatory cytokines in pulmonary diseases, and this may be beneficial for better clinical outcomes in COVID-19 patients. Pentoxifylline enhances blood flow, improves microcirculation and tissue oxygenation, and caffeine also efficiently improves microcirculation, reduces cardiovascular disease, and an effective analgesic. -

Phosphodiesterase Inhibitors in Acute Lung Injury: What Are the Perspectives?
International Journal of Molecular Sciences Review Phosphodiesterase Inhibitors in Acute Lung Injury: What Are the Perspectives? Daniela Mokra 1,* and Juraj Mokry 2 1 Department of Physiology, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, 03601 Martin, Slovakia 2 Department of Pharmacology, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, 03601 Martin, Slovakia; [email protected] * Correspondence: [email protected] Abstract: Despite progress in understanding the pathophysiology of acute lung damage, currently approved treatment possibilities are limited to lung-protective ventilation, prone positioning, and supportive interventions. Various pharmacological approaches have also been tested, with neuro- muscular blockers and corticosteroids considered as the most promising. However, inhibitors of phosphodiesterases (PDEs) also exert a broad spectrum of favorable effects potentially beneficial in acute lung damage. This article reviews pharmacological action and therapeutical potential of nonselective and selective PDE inhibitors and summarizes the results from available studies focused on the use of PDE inhibitors in animal models and clinical studies, including their adverse effects. The data suggest that xanthines as representatives of nonselective PDE inhibitors may reduce acute lung damage, and decrease mortality and length of hospital stay. Various (selective) PDE3, PDE4, and PDE5 inhibitors have also demonstrated stabilization of the pulmonary epithelial–endothelial barrier