Sequential Organ Failure Assessment (SOFA) Score
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Glasgow Coma Scale
CalculatedPOWERED BY Decisions Clinical Decision Support for Pediatric Emergency Medicine Practice Subscribers Glasgow Coma Scale Introduction: The Glasgow Coma Scale (GCS) estimates coma severity based on eye, verbal, and motor criteria. Click the thumbnail above to access the calculator. Points & Pearls • The Glasgow Coma Scale (GCS) allows provid- agreement between providers, training and ers in multiple settings and with varying levels education are available online from the GCS of training to communicate succinctly about a creators at www.glasgowcomascale.org. patient’s mental status. • Simpler scores that have been shown to per- • The GCS has been shown to have statistical form as well as the GCS in the prehospital and correlation with a broad array of adverse neuro- emergency department setting (for initial evalu- logic outcomes, including brain injury, need for ation); these are often contracted versions of the neurosurgery, and mortality. GCS itself. For example, the Simplified Motor • The GCS score has been incorporated into Score (SMS) uses the motor portion of the GCS numerous guidelines and assessment scores only. THE SMS and other contracted scores are (eg, Advanced Cardiac Life Support, Advanced less well studied than the GCS for outcomes Trauma Life Support, Acute Physiology and like long-term mortality, and the GCS has been Chronic Health Evaluation I-III, the Trauma and studied as trended over time, while the SMS has Injury Severity Score, and the World Federation not. of Neurologic Surgeons Subarachnoid Hemor- rhage Grading Scale) Critical Actions Although it has been adopted widely and in a Points to keep in mind: variety of settings, the GCS score is not intended • Correlation with outcome and severity is most for quantitative use. -

Application of Different Scoring Systems and Their Value in Pediatric
Egyptian Pediatric Association Gazette (2014) 62,59–64 HOSTED BY Contents lists available at ScienceDirect Egyptian Pediatric Association Gazette journal homepage: http://www.elsevier.com/locate/epag Application of different scoring systems and their value in pediatric intensive care unit Hanaa I. Rady *, Shereen A. Mohamed, Nabil A. Mohssen, Mohamed ElBaz Department of Pediatrics, Faculty of Medicine, Cairo University, Cairo, Egypt Received 4 September 2014; accepted 28 October 2014 Available online 17 November 2014 KEYWORDS Abstract Background: Little is known on the impact of risk factors that may complicate the Scoring systems; course of critical illness. Scoring systems in ICUs allow assessment of the severity of diseases and Pediatric intensive care unit; predicting mortality. Mortality rate; Objectives: Apply commonly used scores for assessment of illness severity and identify the combi- Critical care; nation of factors predicting patient’s outcome. Illness severity; Methods: We included 231 patients admitted to PICU of Cairo University, Pediatric Hospital. Multiple organ dysfunction PRISM III, PIM2, PEMOD, PELOD, TISS and SOFA scores were applied on the day of admis- sion. Follow up was done using SOFA score and TISS. Results: There were positive correlations between PRISM III, PIM2, PELOD, PEMOD, SOFA and TISS on the day of admission, and the mortality rate (p < 0.0001). TISS and SOFA score had the highest discrimination ability (AUC: 0.81, 0.765, respectively). Significant positive correla- tions were found between SOFA score and TISS scores on days 1, 3 and 7 and PICU mortality rate (p < 0.0001). TISS had more ability of discrimination than SOFA score on day 1 (AUC: 0.843, 0.787, respectively). -

Sepsis-Related Organ Failure Assessment Score Is a Strong Predictor of Survival in Acute-On-Chronic Liver Failure
DANISH MEDICAL JOURNAL Sepsis-related Organ Failure Assessment Score is a strong predictor of survival in acute-on-chronic liver failure Frederik Cold1, Frank Vinholt Schiødt1, Frank Christian Pott2, Nina Strandkjær2 & Erik Christensen1 ABSTRACT vival of patients with ACLF is more effectively calcu- INTRODUCTION: The mortality of patients with an exacer lated by using ICU-specific scoring systems than scores ORIGINAL ARTICLE bation of decompensated liver cirrhosis is high even if focusing only on liver function [1, 6], great efforts have 1) Centre of Abdominal treated in the intensive care unit (ICU), and the criteria for been made to develop new scoring systems to assist the Disease K, Section of Medical Gastroentero- referral to ICU are not well defined. The objective of this clinicians. The most recent score is the Chronic Liver logy and Hepatology, study was to identify variables associated with mortality. Failure-Sequential Organ Failure Assessment (CLIF- Bispebjerg Hospital METHODS: A singlecentre retrospective cohort analysis SOFA) scoring system [1, 7]. 2) Department of was conducted in a universityaffiliated ICU. A total of 53 Despite progress in the prediction of mortality in Anaesthesia and Intensive Care adult patients with decompensated alcoholic liver cirrhosis the ICU [2, 4, 6, 8], the criteria for transfer to the ICU were admitted from January 2012 to June 2015. Variables Medicine, Bispebjerg may still be improved. Hospital, Denmark associated with survival were identified using Cox The aim of this study was to investigate the survival regression analysis. of patients with ACLF referred to the ICU and to iden- Dan Med J RESULTS: The tenday, 30day, 90day, and oneyear tify those variables that hold the best prognostic infor- 2019;66(8):A5557 mortality were 36%, 57%, 66%, and 80%, respectively. -

Prediction of Median Survival Time in Sepsis Patients by the SOFA Score
Burns & Trauma, 2020, 8, tkz006 doi: 10.1093/burnst/tkz006 Research Article Research Article Prediction of median survival time in sepsis patients by the SOFA score combined with different predictors Wen Li1, Meiping Wang1,2, Bo Zhu1, Yibing Zhu1,3,* and Xiuming Xi1,* 1Department of Critical Care Medicine, Fuxing Hospital, Capital Medical University. 20A Fuxingmenwai Street, Xicheng District, Beijing 100038, China, 2Department of Epidemiology and Health Statistics, School of Public Health, Capital Medical University. 10 Xitoutiao, Youanmenwai, Fengtai District, Beijing 100069, China and 3Department of Statistics, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100037, China *Correspondence. Xiuming Xi, Email: [email protected]; Yibing Zhu, Email: [email protected] Received 30 July 2019; Revised 21 August 2019; Editorial decision 27 November 2019 Abstract Background: Sepsis is the leading cause of intensive care unit (ICU) admission. The purpose of this study was to explore the prognostic value of the Sequential Organ Failure Assessment (SOFA) score, the Acute Physiological and Chronic Health Evaluation II (APACHE II) score, and procalcitonin (PCT), albumin (ALB), and lactate (LAC) levels in patients with sepsis. Methods: Consecutive adult patients with suspected or documented sepsis at ICU admission were recruited. Their basic vital signs and related auxiliary examinations to determine their PCT and ALB levels and APACHE II score were recorded at ICU admission, and their LAC levels and SOFA scores were recorded for one week after admission. The influence of these variables on hospital mortality was evaluated. Logistic regression was used to derive the Sepsis Hospital Mortality Score (SHMS), a prediction equation describing the relationship between predictors and hospital mortality. -

Jama Raschke 2021 Ld 210012
Letters 6. Haute Autorité de Santé (HAS). Stratégie de vaccination contre le SARS-CoV-2: vaccination des personnes ayant un antécédent de Covid-19 Table. Clinical Characteristics of 675 Study Patients [SARS-CoV-2 vaccination strategy: vaccination of people with a history of Characteristics No. (%)a Covid-19]. Published February 11, 2021. Accessed February 13, 2021. https:// Age, median (IQR), y 63 (53-72) www.has-sante.fr/upload/docs/application/pdf/2021-02/strategie_de_ vaccination_contre_le_sars-cov-2___vaccination_des_personnes_ayant_un_ Age group, y antecedent_de_covid-19_-_synthese.pdf 18-44 92 (14) 45-64 267 (40) Discriminant Accuracy of the SOFA Score 65-74 199 (29) for Determining the Probable Mortality 75-84 102 (15) of Patients With COVID-19 Pneumonia Requiring ≥85 15 (2) Mechanical Ventilation Sex The COVID-19 pandemic has raised concern regarding the ca- Female 270 (40) pacity to provide care for a surge of critically ill patients that Male 405 (60) might require excluding patients with a low probability of short- Race/ethnicityb 1 term survival from receiving mechanical ventilation. A sur- Non-Hispanic White 259 (38) vey identified 26 unique COVID-19 triage policies, of which 20 Hispanic 286 (42) used some form of the Sequential Organ Failure Assessment Native American 68 (10) (SOFA) score.2 Black 28 (4) However, studies performed in 2016 and 2017 have shown Body mass index, median (IQR)c 33 (29-39) only moderate discriminant accuracy of the SOFA score for pre- Medications dicting survival in intensive care unit (ICU) patients with sep- Dexamethasone 255 (36) sis and an area under the receiver operating characteristic curve Remdesivir 326 (48) (AUROC) of 0.74 to 0.75.3,4 We hypothesized that the SOFA Anticoagulants 607 (90) score might be less accurate in patients requiring mechanical Norepinephrine 33 (5) ventilation for COVID-19 pneumonia because such patients generally have severe single-organ dysfunction and less varia- Comorbidities tion in SOFA scores. -

Trauma Measure #5 Documentation of Glasgow Coma Score at Time of Initial Evaluation in TBI
Trauma Measure #5 Documentation of Glasgow Coma Score at Time of Initial Evaluation in TBI National Quality Strategy Domain: Communication and Care Coordination Measure Type (Process/Outcome): Process 2016 PQRS OPTIONS FOR INDIVIDUAL MEASURES: REGISTRY DESCRIPTION: Percentage of trauma activations for patients aged 18 years or older evaluated as part of a trauma activation or trauma consultation who have a traumatic intracranial hemorrhage on initial head CT for which a Glasgow Coma Score (GCS) at the time of initial evaluation is documented in the medical record within 1 hour of hospital arrival. INSTRUCTIONS: This measure is to be reported each time a patient is evaluated as part of a trauma activation or trauma consultation and is found to have a traumatic intracranial hemorrhage on initial head CT. It is anticipated that clinicians who are responsible for the initial trauma evaluation of TBI patients as specified in the denominator coding will submit this measure. Measure Reporting via Registry: Abbreviated Injury Scale (AIS) codes, patient demographics, and the medical record are used to identify patients who are included in the measure’s denominator. The listed numerator options are used to report the numerator of the measure. DENOMINATOR: All patients aged 18 years or older evaluated by an eligible professional as part of a trauma activation or trauma consultation who have a traumatic intracranial hemorrhage on initial head CT). Denominator Criteria: Patients aged 18 years or older AND Patients evaluated as part of a trauma activation -
Sepsis-3 Definitions. What Are They, and How Should We Use Them?
Sepsis-3 definitions. What are they, and how should we use them? William T. Browne, MD, FCCM October 28, 2016 ACCP/SCCM Consensus Definitions • SIRS (Systemic Inflammatory Response Syndrome) – Temperature > 38° C or < 36° C – Heart rate > 90 – Respiratory rate > 20 or pCO2 < 32 mm Hg – WBC > 12,000 or < 4,000 or > 10% bands • Any two of the criteria needed for SIRS diagnosis ACCP/SCCM Consensus Definitions • Sepsis – Must have diagnosis of SIRS – Clinical evidence of infection • bacteremia • infiltrate on CXR • abscess on imaging study ACCP/SCCM Consensus Definitions • Severe sepsis – must have diagnosis of sepsis – evidence of organ dysfunction • Organ dysfunction – increase in BUN/creatinine – elevated LFTs – hypoxia – elevated serum lactate ACCP/SCCM Consensus Definitions • Septic shock – must have findings of severe sepsis – hypotension after adequate fluid resuscitation – systolic BP 40 mm Hg below baseline – may not have hypotension if receiving pressor agents Was this a useful bedside tool? Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection Under these new definitions Sepsis(new) = Severe Sepsis(old) Key concepts of sepsis (1) • Sepsis is the primary cause of death from infection, especially if not recognized and treated promptly. Its recognition mandates urgent attention • Sepsis is a syndrome shaped by pathogen factors and host factors (eg, sex, race and other genetic determinants, age, comorbidities, environment) with characteristics that evolve over time. What differentiates sepsis from infection is an aberrant or dysregulated host response and the presence of organ dysfunction. Key concepts of sepsis (2) • Sepsis-induced organ dysfunction may be occult; therefore, its presence should be considered in any patient presenting with infection. -

On-Line Table 1: Clinical, EEG, and Perfusion Data of Patients with NCSE Age Pre- Lat Signs/ Perfusion (Visual Seizure No
On-line Table 1: Clinical, EEG, and perfusion data of patients with NCSE Age Pre- Lat Signs/ Perfusion (visual Seizure No. (yr) Sex seizure Jerks GCS Ventilation EEG analysis) Classification Epilepsy Comorbidity Survival 1.1 59 M Coma R/Ϫ 6 ϩ SW Hyperperfusion Ins L Coma with NCSE – Cardiac arrest – FT L 1.2 72 F GTCS L/Ϫ 3 ϩ SW Hyperperfusion SSE ϩ Chronic infarction L ϩ PR PR 1.3 60 F GTCS No/Ϫ 3 ϩ SW Hyperperfusion SSE ϩ Traumatic brain injury ϩ FR FR 1.4 72 F GTCS R/ϩ 7 – SW Hyperperfusion SSE ϩ Chronic infarction L – TL TL 1.5 89 F GTCS L/Ϫ 8 – SW Hyperperfusion SSE ϩ Chronic infarction R – FR FR 1.6 67 F CP No/ϩ 11 – SW No Hyperperfusion CPSE ϩ Chronic infarction L ϩ FL 1.7 62 F GTCS R/Ϫ 5 ϩ SW Hyperperfusion SSE – Meningo-encephalitis – FR Ins,TL 1.8 67 M GTCS R/ϩ 5 ϩ SL Hyperperfusion SSE – Subacute SDH L ϩ FP L Ins L 1.9 63 F CP L/Ϫ 11 – SW No hyperperfusion CPSE ϩ Chronic infarction L ϩ TP L Note:—Lat indicates lateralizing; Pre, preceding: R, right; L, left; SW, spike-wave activity; F, frontal; T, temporal; P, parietal; Ins, insular; SDH, subdural hemorrhage; SL, slowing; EEG, electroencephalography; NCSE, nonconvulsive status epilepticus; GCS, Glasgow Coma Scale; GTCS, generalized tonic-clonic seizure; CP, complex-partial; CPSE, complex-partial status epilepticus; SSE, subtle status epilepticus. AJNR Am J Neuroradiol ͉͉www.ajnr.org E1 On-line Table 2: Clinical, EEG, and perfusion data of patients with a postictal state Age Pre- Lat Perfusion (visual No. -

Correlation of Quick SOFA Score and Procalcitonin with Mortality in the Emergency Department
Journal of Advances in Medicine and Medical Research 32(6): 64-69, 2020; Article no.JAMMR.56300 ISSN: 2456-8899 (Past name: British Journal of Medicine and Medical Research, Past ISSN: 2231-0614, NLM ID: 101570965) Correlation of Quick SOFA Score and Procalcitonin with Mortality in the Emergency Department Mandip Singh Bhatia1*, Ritu Attri2, Kumar Rajni Kant3 and Saurabh C. Sharda1 1Department of Internal Medicine, PGIMER, Chandigarh, India. 2Department of Internal Medicine, Government Medical College, Patiala, India. 3Anaesthesia and Critical Care, SGHS Hospital, Mohali, India. Authors’ contributions This work was carried out in collaboration among all authors. Authors MSB and RA designed the study, performed the statistical analysis, wrote the protocol and wrote the first draft of the manuscript. Authors KRK and SCS managed the analyses of the study. Author SCS managed the literature searches. All authors read and approved the final manuscript. Article Information DOI: 10.9734/JAMMR/2020/v32i630434 Editor(s): (1) Dr. Rameshwari Thakur, Muzaffarnagar Medical College, India. Reviewers: (1) Dinesh Yadav, Madhav Hospital, India. (2) Apeksha Niraula, Nepal. (3) Marcel Cerqueira Cesar Machado, University of São Paulo, Brazil. Complete Peer review History: http://www.sdiarticle4.com/review-history/56300 Received 25 February 2020 Accepted 01 May 2020 Original Research Article Published 08 May 2020 ABSTRACT Introduction: Sepsis is defined as life-threatening organ dysfunction caused by the dysregulated host response to infection with high mortality. Early diagnosis and treatment can decrease mortality. Methods: We studied 2031 patients presenting to an emergency department with fever or suspected infection to find the correlation between q SOFA SCORE and procalcitonin levels with mortality. -
Pediatric Index of Mortality 2 Score As an Outcome Predictor in Pediatric Intensive Care Unit in India
Research Article Pediatric index of mortality 2 score as an outcome predictor in pediatric Intensive Care Unit in India Jeyanthi Gandhi, Shanthi Sangareddi, Poovazhagi Varadarajan, Saradha Suresh Background and Aims: Pediatric index of mortality (PIM) 2 score is one of the severity Access this article online scoring systems being used for predicting outcome of patients admitted to intensive Website: www.ijccm.org care units (ICUs). The aim of the present study was to evaluate the usefulness of PIM2 DOI: 10.4103/0972-5229.120320 score in predicting mortality in a tertiary care pediatric ICU (PICU) and to assess the Quick Response Code: Abstract associated factors in predicting mortality such as presence of shock, need for assisted ventilation and Glasgow coma scale <8. Materials and Methods: This was a prospective observation study done at tertiary care PICU from May 2011 to July 2011. Consecutive 119 patients admitted to PICU (aged 1 month to 12 years) were enrolled in the study. PIM2 scoring was done for all patients. The outcome was recorded as death or discharge. The associated factors for mortality were analyzed with SPSS 17. Results: PIM2 score discriminated between death and survival at a 99.8 cut-off, with area under receiver operating characteristic curve 0.843 with 95% confi dence interval (CI) (0.765, 0.903). Most patients were referred late to this hospital, which explains higher death rate (46.2%), lesser length of hospital stay (mean 2.98 days) in the mortality group, and increased rate of mechanical ventilation (68.1%). Presence of shock was independently associated with mortality, as evidenced by binary logistic regression. -

Predictive Value of Scoring System in Severe Pediatric Head Injury
Medicina (Kaunas) 2007; 43(11) 861 Predictive value of scoring system in severe pediatric head injury Dovilė Evalda Grinkevičiūtė, Rimantas Kėvalas, Viktoras Šaferis1, Algimantas Matukevičius1, Vytautas Ragaišis2, Arimantas Tamašauskas1 Department of Children’s Diseases, 1Institute for Biomedical Research, 2Department of Neurosurgery, Kaunas University of Medicine, Lithuania Key words: pediatric head trauma; Glasgow Coma Scale, Pediatric Trauma Score; Glasgow Outcome Scale, Pediatric Index of Mortality 2. Summary. Objectives. To determine the threshold values of Pediatric Index of Mortality 2 (PIM 2) score, Pediatric Trauma Score (PTS), and Glasgow Coma Scale (GCS) score for mortality in children after severe head injury and to evaluate changes in outcomes of children after severe head injury on discharge and after 6 months. Material and methods. All children with severe head injury admitted to the Pediatric Intensive Care Unit of Kaunas University of Medicine Hospital, Lithuania, from January 2004 to June 2006 were prospectively included in the study. The severity of head injury was categorized according to the GCS score ≤8. As initial assessment tools, the PTS, postresuscitation GCS, and PIM 2 scores were calculated for each patient. Outcome was assessed according to Glasgow Outcome Scale on discharge and after 6 months. Results. The study population consisted of 59 children with severe head injury. The group consisted of 37 (62.7%) boys and 22(37.3%) girls; the mean age was 10.6±6.02. The mean GCS, PTS, and PIM 2 scores were 5.9±1.8, 4.8±2.7, and 14.0±19.5, respectively. In terms of overall outcome, 46 (78.0%) patients survived and 13 (22.0%) died. -
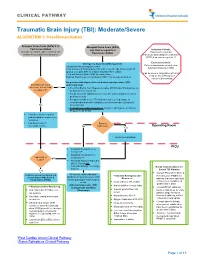
Traumatic Brain Injury (TBI): Moderate/Severe ALGORITHM 1: Post-Resuscitation
CLINICAL PATHWAY Traumatic Brain Injury (TBI): Moderate/Severe ALGORITHM 1: Post-Resuscitation Glasgow Coma Scale (GCS) 9-12 Glasgow Coma Scale (GCS) Post resuscitation less than or equal to 8 Inclusion Criteria: (Consider for children under 2 years old with Post-resuscitation Patient with traumatic concern for acute abusive head trauma) brain injury and Glasgow Coma Scale (GCS) less than or equal to 12 Exclusion Criteria: Emergency Department Management Patients found down without clear Trauma and Neurosurgery Consult traumatic brain injury (TBI) Head Computed Tomography (CT) scan- if not already obtained (STAT upload) or a quick MRI as a viable (radiation-free) option (Can be used in conjunction with Post 2 IVs with Normal Saline (NS) as maintenance Cardiac Arrest Pathway if Modified Rapid sequence intubation (RSI) if not already performed considered beneficial) For patients with signs of elevated intracranial pressure (ICP) Monitor GCS. GCS empirically treat decrease to less than Yes • 3% (0.5 mEq/mL Na+) Hypertonic saline (HTS) bolus 5mL/kg/dose via or equal to 8? peripheral IV or central line • For patients with ongoing seizures use the status epilepticus clinical pathway (below). • For patients with severe TBI who have not received a dose of levetiracetam at another institution, give levetiracetam 20mg/kg IV No (max 2 grams) • If transporting to Operating Room: Consider mild hyperventilation to PCO2 of 32-35 mmHg • Consider comfort sedation and standard neuroprotective measures. • Complete frequent Surgery neurologic exams. No Indicated?