The Selective Cyclooxygenase-2 Inhibitor Nimesulide Prevents Helicobacter Pylori-Associated Gastric Cancer Development in a Mouse Model
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nimesulide: Patients Still Exposed to a Risk of Severe Hepatitis
Translated from Rev Prescrire January 2011; 31 (327): 22-23 Nimesulide: patients still exposed to a risk of severe hepatitis Abstract imesulide, a nonsteroidal anti- Severe liver damage at standard N inflammatory drug (NSAID), has doses, especially in young women. In Nimesulide, a nonsteroidal anti- been on the French market since 2007, the Italian Medicines Agency inflammatory drug (NSAID) that has 1998 (1). It is neither more effective nor released Italian pharmacovigilance data been marketed in France since 1998, is better tolerated than many other showing that hepatic adverse effects rep- neither more effective nor better tol- NSAIDs, and has been shown to cause resented 13.8% of reports implicating erated than other NSAIDs. potentially life-threatening liver da- nimesulide, compared to only 1.4% for mage (1-5). ibuprofen and 2.8% for diclofenac (3). Many reports and reviews published What is known concerning the hepatic The CHMP report published in 2008 by drug regulatory agencies in Spain, adverse effects of nimesulide in early included similar findings. Among the Ireland and Italy have warned of the 2011? 574 reports implicating nimesulide record- hepatic adverse effects of nimesulide. ed in the European EudraVigilance phar- In early 2008, 17 cases of nimesulide- An increasing number of reports of macovigilance database, the proportion of induced liver damage requiring trans- liver damage. Soon after it was first mar- hepatic disorders (cholestasis, jaundice, plantation had been reported in Ire- keted, cases of hepatitis were attributed liver failure, and hepatitis) was higher land, Italy, Spain, Finland and France. to nimesulide, including a case of fulmi- than with cox-2 inhibitors. -

White Paper on Nimesulide Pharmacologic Category
White paper on Nimesulide Pharmacologic Category : Analgesic, Nonsteroidal Anti-inflammatory Drug; Nonsteroidal Anti-inflammatory Drug (NSAID) Indications: Fever, Pain & Inflammation Duration: Can be safely prescribed upto 15 days. Adults: Oral: 100 mg twice daily. Children below 12 years: Not to be used. Product Availability: Product available in various countries; not currently available in the U.S. Dosage Forms: Tablet: 100 mg 1. Nimesulide has preferential selectivity for COX-2 over COX-1 in vivo at full therapeutic doses and induces less gastrointestinal damage than that seen with naproxen in the short term. [ Uptodate: Gut. 2001;48(3):339.] 2. Atopy is a risk factor for non-steroidal anti-inflammatory drug sensitivity. The prevalence of atopy is increased in challenge-proven NSAID-intolerant patients. The atopic condition may represent an important risk factor for developing reactions to these drugs. Paracetamol and nimesulide are relatively safe alternative choices in those patients. [ Uptodate: Ann Allergy Asthma Immunol. 2000;84(1):101.] 3. Topical NSAIDs that are effective for chronic musculoskeletal pain in adults include diclofenac, ketoprofen (level 1 [likely reliable] evidence), ibuprofen, felbinac, and nimesulide (level 2 [mid-level] evidence) [DynaMed] 4. nimesulide may be associated with better efficacy than diclofenac for acute gout (level 2 [mid-level] evidence) [Ter Arkh 2007;79(5):35 ] 5. Nimesulide is safe in Crohn's disease [DynaMed: Clin Gastroenterol Hepatol 2006 Feb;4(2):196] 6. It is safe in ulcerative colitis { DynaMed Clin Gastroenterol Hepatol 2006 Feb;4(2):196, commentary can be found in Clin Gastroenterol Hepatol 2006 Feb;4(2):157] 7. Many PUBMED studies are available about its efficacy in primary dysmennhorea, acute dental pain, respiratory inflammatory conditions etc. -

Effects of the European Restrictive Actions Concerning Nimesulide Prescription
ANN IST SUPER SANITÀ 2010 | VOL. 46, NO. 2: 153-157 153 DOI: 10.4415/ANN_10_02_08 ES Effects of the European restrictive actions I concerning nimesulide prescription: a simulation study on hepatopathies ETHODOLOG M and gastrointestinal bleedings in Italy ND A Mauro Venegoni(a), Roberto Da Cas(b), Francesca Menniti-Ippolito(b) and Giuseppe Traversa(b) RCH A (a)Centro Regionale di Farmacovigilanza, Regione Lombardia, Milan, Italy (b) ESE Centro Nazionale di Epidemiologia, Sorveglianza e Promozione della Salute, R Istituto Superiore di Sanità, Rome, Italy Summary. In 2002 and 2007 the European Medicines Agency (EMA) examined the signals of a greater risk of hepatopathies related to nimesulide use. In 2007 restrictive actions were adopted in Europe. Moreover, EMA initiated a new referral in February 2010. The objective of this paper is to evaluate the effects of the 2007 regulatory measures concerning nimesulide and to estimate the potential effect of further actions. Specifically, we carried out a simulation on the expected number of hospitalisations for hepatopathies and upper gastrointestinal bleedings (UGIBs) in Italy before and after the regulatory measures (2006 vs. 2009), taking into account the shifting of nimesulide prescriptions on other non steroidal anti-inflammatory drugs (NSAIDs). The expected figures of hospitalisation for hepatopathies and UGIBs for all NSAIDs were calculated on the basis of risk estimates reported in two epidemiological studies. The result of the simulation suggests that the im- plementation of the restrictive actions might prevent 79 events of liver injuries, but might increase UGIBs by 859 events. The simulation helped to clarify the effects on hepatopathies and UGIBs as a consequence of nimesulide restriction of use. -

Anti-Proliferative Effects of Piroxicam and Nimesulide on A431 Human
Int J Cancer Manag. 2017 April; 10(4):e7565. doi: 10.5812/ijcm.7565. Published online 2017 April 22. Research Article Anti-Proliferative Effects of Piroxicam and Nimesulide on A431 Human Squamous Carcinoma Cell Line Faezeh Khodaie,1 Yalda Khazaei-Poul,1 and Taraneh Moini-Zanjani1,* 1Department of Pharmacology, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, IR Iran *Corresponding author: Taraneh Moini-Zanjani, Department of Pharmacology, School of Medicine, Shahid Beheshti University of Medical Sciences, Koodakyar Street, Daneshjoo boulevard, Velenjak, Tehran, IR Iran. Tel/Fax: +98-21-22439969, Tel: +98-9123497094, E-mail: [email protected] Received 2016 June 15; Accepted 2017 March 08. Abstract Background: Skin cancer is one of the most common types of cancer worldwide and non-steroidal anti-inflammatory drugs (NSAIDs) have been proposed for prevention and treatment of a variety of cancers. Objectives: In this study we aimed to evaluate the cytotoxic effects of piroxicam (a non-selective cyclooxygenase (COX) inhibitor) and nimesulide (a highly selective COX-2 inhibitor) on A431 human squamous carcinoma cell line. Methods: Squamous carcinoma cell line (A431) was cultured in RPMI medium containing 10% FBS and penicillin-streptomycin at 37°C and 5% CO2. Cells were treated with different concentrations of piroxicam and nimesulide (100 - 1000 µmol/L) for 24, 48 and 72 hours (h). Anti-proliferative effects were determined using MTT colorimetric assay. Results: Piroxicam and nimesulide reduced cell viability in a time and concentration dependent manner. The most cytotoxic effect was produced in 72 hours incubation time. The IC50 value of nimesulide was significantly lower than piroxicam in 24 and 72 hours, but not in 48 hours treatment duration. -

Indomethacin in Pregnancy: Applications and Safety
Original Article 175 Indomethacin in Pregnancy: Applications and Safety Gael Abou-Ghannam, M.D. 1 Ihab M. Usta, M.D. 1 Anwar H. Nassar, M.D. 1 1 Department of Obstetrics and Gynecology, American University of Address for correspondence and reprint requests Anwar H. Nassar, Beirut Medical Center, Hamra, Beirut, Lebanon M.D., American University of Beirut Medical Center, P.O. Box 113-6044/B36, Hamra 110 32090, Beirut, Lebanon (e-mail: [email protected]). Am J Perinatol 2012;29:175–186. Abstract Preterm labor (PTL) is a major cause of neonatal morbidity and mortality worldwide. Among the available tocolytics, indomethacin, a prostaglandin synthetase inhibitor, has been in use since the 1970s. Recent studies have suggested that prostaglandin synthetase inhibitors are superior to other tocolytics in delaying delivery for 48 hours and 7 days. However, increased neonatal complications including oligohydramnios, Keywords renal failure, necrotizing enterocolitis, intraventricular hemorrhage, and closure of the ► indomethacin patent ductus arteriosus have been reported with the use of indomethacin. Indometh- ► tocolysis acin has been also used in women with short cervices as well as in those with idiopathic ► preterm labor polyhydramnios. This article describes the mechanism of action of indomethacin and its ► short cervix clinical applications as a tocolytic agent in women with PTL and cerclage and its use in ► polyhydramnios the context of polyhydramnios. The fetal and neonatal side effects of this drug are also ► fetal side effects summarized and guidelines for its use are proposed. Preterm labor (PTL) is a major cause of neonatal morbidity in women with PTL and cerclage and its use in the context of and mortality worldwide.1 Care of premature infants has polyhydramnios. -

The Importance of COX-2 Inhibition for Aspirin Induced Asthma
S54 Thorax 2000;55 (Suppl 2):S54–S56 Thorax: first published as 10.1136/thorax.55.suppl_2.S54 on 1 October 2000. Downloaded from The importance of COX-2 inhibition for aspirin induced asthma Alan Bennett There have been recent reviews of aspirin “specific” is used here to denote that the activ- induced asthma (AIA),12 the use of the ity is (usually) much greater against COX-2 COX-2 preferential inhibitor nimesulide in than against COX-1. Two drugs with a asthmatic patients intolerant to non-steroidal “preferential” status are nimesulide and mel- anti-inflammatory drugs (NSAIDs),3 and of oxicam, whereas two drugs that probably nimesulide in general.45 This paper discusses deserve the title “specific” are rofecoxib and the importance of inhibiting prostaglandin E2 celecoxib. (PGE2) synthesis in AIA, and the relative Nimesulide (4-nitro-2-phenoxymethane- safety of NSAIDs that preferentially inhibit sulphonanilide) is particularly important in COX-2. AIA because several studies have shown that it Aspirin and other NSAIDs cause broncho- is tolerated by most patients with the disorder constriction in about 10% of asthmatic to about the same extent as paracetamol. This subjects but NSAIDs relieve asthma in about sulphonanilide NSAID, which is eVective in 0.3%.2 This variability helps to show the com- treating a wide spectrum of inflammatory and plexity of the problem. Prostaglandins in painful conditions,7 was first marketed in 1985 human lung are formed by various tissues and and 10 years later it was found to be a cells, including bronchial muscle, epithelium, preferential inhibitor of COX-2.89Because it is and inflammatory cells,12 so the inhibition of not marketed in the USA, Japan, or the UK, prostaglandin formation can have numerous nimesulide is not well known in some parts of eVects. -

Nimesulide for Painful Osteoarthritis
For reprint orders, please contact: DRUG EVALUATION [email protected] Nimesulide for painful osteoarthritis Mauro Bianchi Osteoarthritis is one of the most common joint disorders in the world. It is costly and a major University of Milan, School of cause of pain and disability, especially in the elderly. The severity of pain often calls for Medicine, Department of Pharmacology, Via Vanvitelli, treatment with nonsteroidal anti-inflammatory drugs. Worldwide experience with nimesulide 32, 20129 Milano, Italy shows that this nonsteroidal anti-inflammatory drug has a number of pharmacological Tel.: +39 025 031 6930; properties that may make it favorable in the treatment of joint diseases. In recent years, Fax: +39 025 031 6949; several controlled studies have been carried out in order to investigate its analgesic effects in [email protected] patients with OA. The objective of this article is to review some of the features of osteoarthritis and to identify the role of nimesulide as a drug particularly tailored for the treatment of painful osteoarthritis. Osteoarthritis (OA) is one of the most common Rheumatism (EULAR) [4] and the American Col- forms of musculoskeletal disorder encountered lege of Rheumatology (ACR) Recommendations worldwide, particularly in Western populations. [11]. However, the severity of pain often requires A recent WHO report on the global burden of treatment with nonsteroidal antiinflammatory disease indicates that OA is likely to become one drugs (NSAIDs), which are the drugs preferred by of the most important causes of disability in many patients with OA [12]. Indeed, NSAIDs are both women and men [1]. The prevalence of OA the drug most commonly used by many doctors increases with age, affecting a large proportion of for the management of pain in OA patients, in elderly people [2]. -

Selectivity of Cyclo-Oxygenase Inhibitors in Human Pulmonary Epithelial and Smooth Muscle Cells
Copyright #ERS Journals Ltd 2000 Eur Respir J 2000; 15: 751±756 European Respiratory Journal Printed in UK ± all rights reserved ISSN 0903-1936 Selectivity of cyclo-oxygenase inhibitors in human pulmonary epithelial and smooth muscle cells S.P. Range, L. Pang, E. Holland, A.J. Knox Selectivity of cyclo-oxygenase inhibitors in human pulmonary epithelial and smooth muscle Respiratory Medicine Unit, City Hospital, cells. S.P. Range, L. Pang, E. Holland, A.J. Knox. #ERS Journals Ltd 2000. Hucknall Road, Nottingham, NG5 1PB, ABSTRACT: Cyclo-oxygenase (COX) inhibitors may have a role in reducing in- UK flammation in asthma and other pulmonary diseases. COX inhibitors have different Correspondence: S.P. Range selectivities for the two COX isoenzymes (COX 1 and COX 2) which vary between Dept of Respiratory Medicine purified enzyme and intact cell preparations. The relative selectivity of COX inhi- University Hospital bitors has not been studied in human airway cells. Queen's Medical Centre A number of COX inhibitors in cultured human airway cells were compared which Nottingham NG7 2UH exclusively express either COX 1 (primary degree cultured human airway smooth UK muscle (HASM) cells) or COX 2 (A549 pulmonary epithelial cell-line) as measured by Fax: 44 1159424554 Western blotting. COX activity was assayed by prostaglandin (PG)E2 production following 30 min incubation with 5 mM arachidonic acid. Keywords: A549 cells . -1 airway smooth muscle COX activity in both cell types was similar; HASM cells 92.212.1 ng PGE2 mg . -1 asthma protein, A549 cells 87.724.4 ng PGE2 mg protein. In HASM cells the median -5 -6 cyclo-oxygenase inhibitory concentration (IC50) was >10 M for nimesulide, 3.2610 M for N-(2- cyclo- cyclo-oxygenase inhibitor -8 hexyloxy-4-nitrophenyl)-methanesulphonamide (NS398), 1.8610 M for flurbiprofen, prostaglandin E2 6.7610-9 M for indomethacin and >10-5 M for aspirin. -

ANNEX III SUMMARY of PRODUCT CHARACTERISTICS Note
ANNEX III SUMMARY OF PRODUCT CHARACTERISTICS Note: This SPC is the one that was annexed to the Commission Decision on this Article 31 referral for nimesulide containing medicinal products. The text was valid at that time. After the Commission Decision, the Member State competent authorities will update the product information as required. Therefore, this SPC may not necessarily represent the current text. CPMP/3086/03-REV.1 1 EMEA 2004 SUMMARY OF PRODUCT CHARACTERISTICS NIMESULIDE 100 MG TABLETS, SOLUBLE TABLETS, EFFERVESCENT TABLETS, COATED TABLETS, CAPSULES, HARD CAPSULES, NIMESULIDE 50/100 MG GRANULES OR POWDER FOR ORAL SUSPENSION NIMESULIDE 1%, 2% OR 5% ORAL SUSPENSION CPMP/3086/03-REV.1 2 EMEA 2004 1. NAME OF THE MEDICINAL PRODUCT <TRADENAME> 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet, soluble tablet, effervescent tablet, coated tablet, capsule, hard capsule contains 100mg nimesulide. Each sachet contains 50 or 100mg nimesulide. Oral suspension containing 10mg, 20mg or 50mg per ml. For excipients, see section 6.1 3. PHARMACEUTICAL FORM Tablet, soluble tablet, effervescent tablet or coated tablet: <Company-specific> Granules or powder for oral suspension: <Company-specific> Capsule, hard capsule: <Company-specific> Oral suspension: <Company-specific> 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of acute pain. Symptomatic treatment of painful osteoarthritis. Primary dysmenorrhoea. 4.2 Posology and method of administration <Nimesulide-containing medicinal products> should be used for the shortest possible duration, as required by the clinical situation. Adults: 100mg nimesulide tablets, soluble tablets, effervescent tablets, coated tablets, capsules, hard capsules, 50mg and 100mg granules or powder, 1%, 2% and 5% oral suspension: 100mg bid after meal Elderly: in elderly patients there is no need to reduce the daily dosage (see section 5.2). -

The Effects of Etodolac, Nimesulid and Naproxen Sodium on the Frequency of Sister Chromatid Exchange After Enclused Third Molars Surgery
Yonsei Med J 49(5):742 - 747, 2008 DOI 10.3349/ymj.2008.49.5.742 The Effects of Etodolac, Nimesulid and Naproxen Sodium on the Frequency of Sister Chromatid Exchange after Enclused Third Molars Surgery Banu Gürkan Köseoğlu,1 Şükrü Öztürk,2 Hülya Koçak,1 Şükrü Palanduz,2 and Kıvanç Çefle2 1Department of Oral Surgery, Istanbul University, Faculty of Dentistry, Istanbul; 2Department of Internal Medicine, Istanbul University, Istanbul Medical Faculty, Division of Medical Genetics, Istanbul, Turkey. Purpose: Non-steroidal anti-inflammatory drugs (NSAID) diseases, orthopedic and gynecologic surgery and are frequently used in oral surgical procedures in dentistry. in soft tissue traumas. This group of medications The evaluation of the frequency of sister chromatid exchange is also commonly used in the clinical practice of (SCE) is accepted as a reliable cytogenetic method to assess dentistry, such as in the treatment of oro-facial the genotoxic effects of environmental factors. Materials and 3,4 Methods: In this study, the genotoxic effects of various pain or after oral surgical procedures. NSAIDs were assessed in 30 patients to who they were Some NSAIDs are widely used in Turkey, administered following encluosed third molar surgery using without prescription, for their analgesic and SCE analysis before and after the operation. The frequency of anti-inflammatory properties. SCE was evaluated before the operation and after 3 days of Naproxen, a propionic acid derivative, is a etodolac, nimesulid and naproxen use. Results: There was no prototypical anti-inflammatory agent which is statistically significant difference in the frequency of SCE between the preoperative and postoperative states in patients generally used for the treatment of rheumatoid given etodolac, nimesulid or naproxen sodium. -
Nimesulide.Pdf
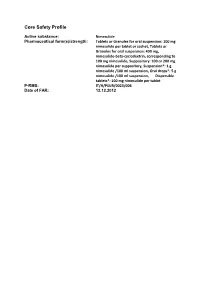
Core0B Safety Profile Active substance: Nimesulide Pharmaceutical form(s)/strength: Tablets or Granules for oral suspension: 100 mg nimesulide per tablet or sachet, Tablets or Granules for oral suspension: 400 mg, nimesulide-beta-cyclodextrin, corresponding to 100 mg nimesulide, Suppository: 100 or 200 mg nimesulide per suppository, Suspension*: 1 g nimesulide /100 ml suspension, Oral drops*: 5 g nimesulide /100 ml suspension, Dispersible tablets*: 100 mg nimesulide per tablet P-RMS: IT/H/PSUR/0023/006 Date of FAR: 12.12.2012 2. Posology and Method of Administration <Nimesulide-containing medicinal products> should be used for the shortest possible duration, as required by the clinical situation. Moreover, undesirable effects may be minimized by using the minimum effective dose for the shortest duration necessary to control symptoms (see Section 4). The maximum duration of a treatment course with nimesulide is 15 days. Adults: Tablets or Granules: 100 mg twice a day after meals 400 mg nimesulide-beta-cyclodextrin Tablets or Granules: 400 mg (= 100 mg nimesulide) twice a day after meals Suppositories: 200 mg twice a day Elderly: in elderly patients there is no need to reduce the daily dosage. Children (< 12 years): <Nimesulide-containing medicinal products> are contraindicated in these patients (see also Section 3). Adolescents (from 12 to 18 years): on the basis of the kinetic profile in adults and on the pharmacodynamic characteristics of nimesulide, no dosage adjustment in these patients is necessary. Impaired renal function: on the basis of pharmacokinetics, no dosage adjustment is necessary in patients with mild to moderate renal impairment (creatinine clearance of 30-80 ml/min), while <Nimesulide-containing medicinal products> are contraindicated in case of severe renal impairment (creatinine clearance < 30 ml/min) (see Section 3). -

(12) Patent Application Publication (10) Pub
US 2004O156872A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0156872 A1 Bosch et al. (43) Pub. Date: Aug. 12, 2004 (54) NOVEL NMESULIDE COMPOSITIONS application No. 09/572,961, filed on May 18, 2000, now Pat. No. 6,316,029. (75) Inventors: H. William Bosch, Bryn Mawr, PA (US); Christian F. Wertz, Brookhaven, Publication Classification PA (US) (51) Int. Cl. ............................ A61K 9/14; A61K 9/00 Correspondence Address: FOLEY AND LARDNER (52) U.S. Cl. ............................................ 424/400; 424/489 SUTE 500 3000 KSTREET NW WASHINGTON, DC 20007 (US) (57) ABSTRACT (73) Assignee: Elan Pharma International Ltd. The present invention provides nanoparticulate nimeSulide (21) Appl. No.: 10/697,703 compositions. The compositions preferably comprise nime (22) Filed: Oct. 31, 2003 Sulide and at least one Surface Stabilizer adsorbed on or asSociated with the Surface of the nimeSulide particles. The Related U.S. Application Data nanoparticulate nimeSulide particles preferably have an effective average particle size of less than about 2000 nm. (63) Continuation-in-part of application No. 10/276,400, The invention also provides methods of making and using filed on Jan. 15, 2003, which is a continuation of nanoparticulate nimeSulide compositions. US 2004/O156872 A1 Aug. 12, 2004 NOVEL NMESULIDE COMPOSITIONS tion;' U.S. Pat. Nos. 5,399,363 and 5,494,683, both for “Surface Modified Anticancer Nanoparticles; U.S. Pat. No. RELATED APPLICATIONS 5,401,492 for “Water Insoluble Non-Magnetic Manganese Particles as Magnetic Resonance Enhancement Agents,” 0001. This application is a continuation-in-part of U.S. U.S. Pat. No.