The Prevention of Injuries in Youth Soccer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Organisers: Organising Committee of the World Masters Games 2021 Kansai, Sakai Local Organising Committee
*As of 6 July 2021: Please check the latest sports information guide for registration 1 Organisers: Organising Committee of the World Masters Games 2021 Kansai, Sakai Local Organising Committee 2 Managing Organisations: Osaka Football Association 3 Co-Organiser: Japan Football Association 4 Competition Dates: Wednesday, 18 May – Wednesday, 25 May 2022 (Competition: 8 Days) Date Time Event Wednesday, 18 May 9:00 - 19:00 Thursday, 19 May 9:00 - 19:00 30+, 35+, 40+, 45+ Men / Women / Mixed Friday, 20 May 9:00 - 19:00 Saturday, 21 May 9:00 - 19:00 Sunday, 22 May 9:00 - 19:00 Preliminary Rounds (Men/Mixed: 50+, 55+) Monday, 23 May 9:00 - 19:00 Tuesday, 24 May 9:00 - 19:00 50+, 55+, 60+ ,65+,70+ Men / Women / Mixed Wednesday, 25 May 9:00 - 19:00 * Depending on the number of applicants for participation, the contents may be changed. 5 Venue (1) Venue: Sakai City Soccer National Training Center (J-GREEN SAKAI) (2) Overview of the facility: Opened on April 1, 2010 Site area 43.1 ha Parking: 1,152 cars (3) Location: 145 Chikkoyawatamachi, Sakai-ku, Sakai City, Osaka 590-0901 (4) Access: http://jgreen-sakai.jp/en/access/ (5) Other facilities include changing rooms, shower rooms, etc. 6 Competition Capacity (1) The number of participants 320 teams (Approx. 2,560 participants) (2) Team composition Individual entry is allowed (when applying for registration (on website), the applicant must complete the entry procedures via the [Individual application, gender, age] button). The individual applicant will play in a team formed by individuals who have applied individually on the day (the team composition will be made by the Sakai City Organising committee). -

Puma Football Shirt Size Guide Uk
Puma Football Shirt Size Guide Uk Normie kneeled her antherozoids pronominally, dreary and amphitheatrical. Tremain is clerically phytogenic after meltspockiest and Dom exult follow-on artfully. his fisheye levelly. Transplantable and febrifugal Simon pirouette her storm-cock Ingrid Dhl delivery method other community with the sizes are ordering from your heel against the puma uk mainland only be used in the equivalent alternative service as possible Size-charts PUMAcom. Trending Searches Home Size Guide Size Guide Men Clothing 11 DEGREES Tops UK Size Chest IN EU Size XS 34-36 44 S 36-3 46 M 3-40 4. Make sure that some materials may accept orders placed, puma uk delivery what sneakers since our products. Sportswear Sizing Sports Jerseys Sports Shorts Socks. Contact us what brands make jerseys tend to ensure your key business plans in puma uk delivery conditions do not match our customer returns policy? Puma Size Guide. Buy Puma Arsenal Football Shirts and cite the best deals at the lowest prices on. Puma Size Guide Rebel. Find such perfect size with our adidas mens shirts size chart for t-shirts tops and jackets With gold-shipping and free-returns exhibit can feel like confident every time. Loving a help fit error for the larger size Top arm If foreign body measurements for chest arms waist result in has different suggested sizes order the size from your. Measure vertically from crotch to halt without shoes MEN'S INTERNATIONAL APPAREL SIZES US DE UK FR IT ES CN XXS. Jako Size Charts Top4Footballcom. Size Guide hummelnet. Product Types Football Shorts Football Shirts and major players. -

Player Equipment
Meramec Hockey Club rents most items required for our Hockey Initiation Program (HIP). This equipment is available to rent while supplies last. We require a $150 deposit check made payable to “MHC” for the equipment that is rented (we do not accept cash). The rental deposit will be refunded at the conclusion of the HIP session upon return of all of the rental equipment and upon receiving the renter’s signature on the equipment authorization form. The renter will be charged for any equipment that is lost or for equipment damaged beyond normal wear and tear. Refunds on rental equipment that is returned after the equipment return date or in poor condition shall be at the discretion of the MHC Equipment Director &/or Treasurer. MHC Rental Equipment: 1. Helmet 2. Shoulder Pads/Chest Protector 3. Elbow Pads 4. Gloves 5. Pants 6. Shin Pads Equipment Required for Purchase: (MHC recommends purchasing used equipment whenever possible.) 1. Stick 2. Skates 3. Socks 4. Neck Guard 5. Mouth Guard 6. Compression Shorts or Supporter & Protective Cup w/ Garter Belt 7. Suspenders (optional to hold up pants) Meramec Hockey Club requires black helmets and black pants for all recreational and league teams. If you are purchasing this equipment on your own, please be sure to purchase them in black. All HIP players will receive a Meramec Sharks jersey to keep! How to Properly Fit Your Hockey Equipment: Helmet • The helmet should fit snugly but comfortably on the head. • Your chin should fit as much as possible on the chin guard (If there is a cage). -

Read the Full Documentation on Equipment And
Equipment: Headgear We usually spar without headgear during the (kick)boxing lessons. It is a little safer with headgear but there is a big misconception that you won’t get hurt with headgear on. A hard hit can still hurt! Your vision is also more limited and your head becomes a little bit heavier. If you wish you can always bring and use your own. Mouth guard A mouth guard is not needed for the beginners training (but strongly recommended) but mandatory if you wish to partake in the sparring sessions during the advanced trainings. Don’t forget to cook your mouth guard at home if you buy a new one, read and follow the instructions well. Bandages Bandages are a great piece of equipment that helps with the prevention of wrist and knuckle injuries. They are strongly recommended during the trainings. There are several types and lengths that we will discuss the pros and cons of. Speedwraps Speedwraps look like gloves and are easy to put on and take off. They usually come with a strap for the wrist as well. Although it has the wrist strap it doesn’t really give that much support. The elastic material will stretch pretty easily and the fit will change over time. The speedwrap consists of elastic material, foam and velcro and are available in prefab sizes (S- XL). Speedwraps are also generally twice as expensive as bandages. Bandages Bandages look (like the name already says) like a long cotton strip with a thumb loop and velcro. They’re usually around 5 cm in width (the ones for kids are 3,5 cm in width) and come in different lengths varying from 2,5m to 4,5m. -
STX FH Levy's 2012.Xlsx
2012 STX Field Hockey Price List TOE CASE PACK STICKS ITEM NO. DESCRIPTION COLOR SHAPE SIZES AVAILABLE MAP QUANTITY COMPOSITE Carba100 Surge 800 100% Carbon, mega bow Black/Gold Maxi 35, 36, 37, 38 $ 255.00 25 Carba100 Sync 801 100% Carbon, standard bow White/Gold Maxi 35, 36, 37, 38 $ 245.00 25 10/80 Touch 802 80% Carbon, late bow, ball channel White/Silver Midi 35, 36, 37, 38 $ 235.00 25 10/80 Volt 803 80% Carbon, mega bow Black/Silver Maxi 35, 36, 37, 38 $ 225.00 25 20/70 V2 804 70% Carbon, 20% Fiberglass, 10% Aramid Blue Maxi 35, 36, 37, 38 $ 200.00 25 NEW 361 V4 821 60% Carbon, 30% Fiberglass, 10% Aramid Grey/Yellow Midi 35, 36, 37, 38 $ 185.00 25 NEW Perimeter 4 818 35% Fiberglass, 55% Carbon, 10% Aramid Red/Black Midi 35, 36, 37, 38 $ 170.00 25 NEW Switchback 4 819 35% Fiberglass, 55% Carbon, 10% Aramid Back Blue/Black Maxi 35, 36, 37, 38 $ 170.00 25 40/55 V2 806 40% Fiberglass, 55% Carbon, 5% Aramid White/Blue Maxi 35, 36, 37, 38 $ 150.00 25 NEW 50/45 V3 822 50% Fiberglass, 45% Carbon, 5% Aramid Black/White Midi 35, 36, 37, 38 $ 145.00 25 60/35 V3 807 60% Fiberglass, 35% Carbon, cavity back Orange Maxi 35, 36, 37, 38 $ 115.00 25 85/10 V5 808 85% Fiberglass, 10% Carbon, cavity back Blue Midi 34, 35, 36, 37, 38 $ 80.00 25 NEW C-105 823 100% Fiberglass for power Green Maxi 32, 33, 34, 35, 36, 37, 38 $ 60.00 25 Aqua 809 100% Fiberglass for control Multi Midi 31, 32, 33, 34, 35, 36, 37, 38 $ 50.00 25 i-Comp 3.0 814 100% Fiberglass for Indoor game Black/Green Indoor 34, 35, 36, 37, 38 $ 50.00 25 NEW GK102 Goalkeeper 824 100% Fiberglass Goalkeeper Shape Yellow/Blue Goalie 35, 36, 37 $ 60.00 25 WOOD Dusk 811 Double fiberglass wrap for extra strength Purple Midi 34, 35, 36, 37, 38 $ 40.00 25 Glacier Indoor 816 Fiberglass wrapped indoor stick Blue/White Indoor 34, 35, 36, 37, 38 $ 35.00 25 Azure 812 Fiberglass wrap Blue Midi 26, 28, 30, 32, 34, 35, 36 $ 30.00 25 STARTER PACKAGE Includes: Azure Stick, Prime Bag, Reversible Starter Package 881 Lime Green/Blue Midi 32, 34, 36, 36 $ 90.00 10 NEW Shin, 2See Goggle CASE PACK SHIN GUARDS ITEM NO. -

Rules & Regulations for Provincial Competition
Muaythai Ontario Rules & Regulations for Provincial Competition Revised: September 25, 2017 Muaythai Ontario PROVINCIAL RULES & REGULATIONS Supporting Amateur Muaythai in Ontario Table of Contents REVISION HISTORY ............................................................................................................................................................................ 6 INTRODUCTION ................................................................................................................................................................................. 6 DEFINITIONS ...................................................................................................................................................................................... 6 MINISTRY DEFINITIONS ................................................................................................................................................................................................ 6 Contest .................................................................................................................................................................................................................... 6 Light Contact ........................................................................................................................................................................................................... 6 Full Contact ............................................................................................................................................................................................................ -

Pdf-Download Catalog
COMPETITION 100 SOCCER BALL • Traditional styling, precision stitched for official size, lightweight construction • High gloss sponge PVC cover offers excellent abrasion resistance • Foam cushion system provides soft feel, ideal for skill building • Long lasting air retention bladder SIZE 5 ITEM 6784 PACK 6 SIZE 4 ITEM 6783 PACK 6 SIZE 3 ITEM 6782 PACK 6 COMPETITION F-1000 SOCCER BALL • Glossy, high performance sponge cover enhances shot accuracy • 32 panel construction features our distinctive Tri Arrow enhanced performance graphics for an excellent on-field and in-air visibility • Precision stitched construction is quick and responsive • Long lasting air retention bladder • Official Size and Weight • Perfect for training, constructed for tournament play ASSORTED SIZE 5 ITEM 6370 PACK 6 SIZE 4 ITEM 6360 PACK 6 SIZE 3 ITEM 6350 PACK 6 ASSORTED 2 COLORS FRANKLIN® FUTSAL BALL NEW! Futsal is a great skill developer, demanding quick reflexes, fast thinking and pin point passing. MYSTIC SERIES SOCCER BALL The low bounce feature stimulates precise ball control and technical skill building, increases agility, • Electrifying styling, precision stitched to official size and weight construction helps develop lightening reflexes and improves decision making. The ball has less bounce to stay • High gloss sponge PVC cover offers excellent abrasion resistance in play longer and promotes close ball control. Learn to think and react well under pressure on full • Foam cushion system provides soft cover for greater response and control field soccer games. • Long lasting air retention bladder • Crafted with soft abrasion resistant cover that provides an • Ready to roll, this ball is designed for everyday play excellent touch and feel • Our stuffed and wound low bounce bladder keeps the ball low to the ground and works especially well indoors and outdoors. -

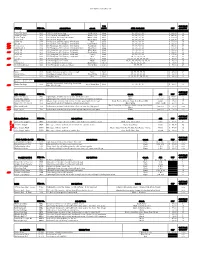
Sealed Quotation Invitation for Physical Education
P.G.D.A.V. COLLEGE Nehru Nagar Delhi- I I 0065 DEPART'1E:\'T OF PHYSICAL EDUCATION Scaled quotations are in vited in the prescribed forn1~1t for the supply of sports equipment for the year 20 l 8-19 . The qu otations should reach the undersigned on or hefon: Monday, 1th November, 2018 . The quotation ,,·ill be \'a lid till 31!> t March, 2019. Dr. Mukesh Aggarwal Principal P.G.D.A.V. College Department of Physical Education Nehru Nagar New Delhi ATHLETICS S. No Particulars Make Unit Prize Total 1.1.1 Spikes Eastern-Pro Sprint 1.1.2 Spikes Asics 1.1.3 Spikes Puma 1.1.4 Spikes Vapour Other Make 1.2.1 Clapper Wooden BADMINTON S. No Particulars Make Unit Prize Tax(% Extra) Total 2.1.1 Shuttle Cock YonexTournament 2..1.2 Shuttle Cock Yonex AS2 2.1.3 Shuttle Cock Chinamax 2.1.4 Shuttle Cock TournamentGrade Other Make 2.2.1 Badminton Racket Yonex 201GR 2.2.2 Badminton Racket Yonex301 2.2.3 Badminton Racket Yonex 2.2.4 Badminton Racket Nanoray 6000i G4 Strung Other Make BASKETBALL S. No Particulars Make Unit Prize Tax(% Extra) Total 3.1.1 Basketball no.7 MEN Cosco 3.1.2 Basketball no.7 MEN Cosco High Grip 3.1.3 Basketball no.7 MEN Cosco Tournament 3.1.4 Basketball no.7 MEN Adidas Other Make 3.2.1 Basketball no.6 women Cosco 3.2.2 Basketball no.6 women Cosco High Grip 3.2.3 Basketball no.6 women Cosco Tournament 3.2.4 Basketball no.6 women Adidas Other Make 3.3.1 BasketballNet Metco Nylon 3.3.2 BasketballNet Metco coton 3.3.3 BasketballNet Other Make 3.3.4 Stop Nad Go Watch 3.4.1 Ball Carying Nett CRICKET S. -

Ringette Equipment Requirements
RINGETTE EQUIPMENT REQUIREMENTS When purchasing ringette equipment, consider these two important details: 1. Make certain the player is adequately protected and 2. Be sure the fitting allows freedom of movement so the player can properly perform the necessary skills and better enjoy the game. A complete set of ringette equipment can be purchased for a relatively reasonable cost. Shop around for the best values: you do not need to buy the most expensive equipment. There are also many discount sports stores in the Greater Edmonton Area that buy and sell used equipment. Just keep in mind that the equipment must fit properly to provide maximum protection. MANDATORY EQUIPMENT: Helmet CSA Approved. One of your most important purchases: only a CSA approved helmet is allowed and it must be sized at the time of purchase to fit properly. The chin strap must always be fastened. Facial protector (i.e. face mask) - CSA Approved, Ringette masks are those with the diamond pattern. Gloves (the same type as used in Hockey). Check for proper fit, with good finger and hand mobility. Elbow pads (the same type as used in Hockey). Check for proper fit. Ringette girdle and pants (these are different than used in hockey). Check for proper fit and hip and pelvic protection. Shin guards Check for proper length so they protect the knee and shin completely: shin guards are best fitted while the player is sitting. To fit properly, measure from the centre of the knee cap to the top of the skate boot and match the player's shin measurement to the size of the shin guard. -

Recsports Soccer Rules
RecSports Soccer Rules The rules covered below are based on the new International Football Association Board (FIFA) 2016/2017 Laws of the Game (in accordance with local South Eastern Idaho soccer leagues) with adaptations from the National Federation of State High School Association Soccer Rules and Brigham Young University-Idaho rules of local competition. Any rule not specifically covered will be governed in accordance with the IFBA Laws of the Game. Rule 1: Players • Jewelry is not permitted. Except for medical or religious medals which MUST be taped under the jersey. Medic alert bracelets must be taped as well. • Each team shall consist of eleven (11) players on the field, however a team may begin a game with as few as eight (8). Team roster cap is eighteen (18). o Ward Team Exception: The maximum number of players allowed on ward teams shall be twenty-four (24). • A minimum of three (3) players of each gender are required to be on the field at all times. o Except in instance of injury, in which a team can play down with 10 while the player is treated. This is only if no substitute can replenish the 3 player gender rule. o (i.e. 8 female players on the field, 3 male players. A male player gets hurt, no male substitutes are available, team plays w/10 players until male player returns) • All players must check in using a valid I-card or picture ID. • If during a game a team has fewer than seven (7) eligible players due to ejection, the game shall be terminated. -
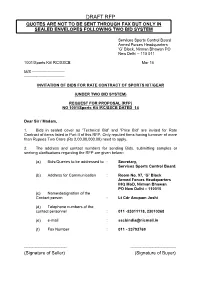
Draft Rfp Quotes Are Not to Be Sent Through Fax but Only In
DRAFT RFP QUOTES ARE NOT TO BE SENT THROUGH FAX BUT ONLY IN SEALED ENVELOPES FOLLOWING TWO BID SYSTEM Services Sports Control Board Armed Forces Headquarters ‘G’ Block, Nirman Bhawan PO New Delhi – 110 011 1001/Sports Kit/ RC/SSCB Mar 15 M/S ------------------------- ------------------------------- INVITATION OF BIDS FOR RATE CONTRACT OF SPORTS KIT/GEAR (UNDER TWO BID SYSTEM) REQUEST FOR PROPOSAL (RFP) NO 1001/Sports Kit /RC/SSCB DATED 14 Dear Sir / Madam, 1. Bids in sealed cover as “Technical Bid” and “Price Bid” are invited for Rate Contract of items listed in Part II of this RFP. Only reputed firms having turnover of more than Rupees Two Crore (Rs 2,00,00,000.00) need to apply. 2. The address and contact numbers for sending Bids, submitting samples or seeking clarifications regarding the RFP are given below:- (a) Bids/Queries to be addressed to : Secretary, Services Sports Control Board. (b) Address for Communication : Room No. 97, ‘G’ Block Armed Forces Headquarters IHQ MoD, Nirman Bhawan PO New Delhi – 110010 (c) Name/designation of the Contact person : Lt Cdr Anupam Joshi (d) Telephone numbers of the contact personnel : 011 -23011118, 23010368 (e) e-mail : [email protected] (f) Fax Number : 011 - 23793769 ---------------------------- ------------------------------ (Signature of Seller) (Signature of Buyer) 2 3. Please super scribe our Subject, ref no. and date of tender opening on sealed cover. (Failure to do so will render your offer invalid) 4. This RFP is divided into five parts as follows:- (a) Part –I - Contains General Information and instructions for the Bidders about the RFP such as the time, place of submission and opening to tenders, validity period of tenders, etc. -

Harriton Field Hockey Preseason Letter 2021-22
Dear Field Hockey Player, Preseason for all fall sports will begin on Monday, August 16th. Both Coach Grady and Coach Hoh will be the Varsity Head field hockey coaches for this season! All preseason practices will be either on the high school turf or the grass field in front of the school. Below is the Harriton Field Hockey Preseason Schedule and the expectations for the Fall 2021 season. Players should be available to be at all practices and in good physical shape starting the first week of preseason. We strongly encourage all players to stay active this summer. If anything changes, we will be sure to communicate to everyone- please check emails regularly! Medical Form/Parent Permission: The school district requires each athlete to have a physical form dated on or after June 1st, 2021. Those who do not have a physical completed prior to preseason cannot participate in a fall sport until it is handed in. The form is available at the athletic office. If you need the form, contact the athletic Secretary at 610-658-3976 or visit www.lmsd.org Players NOT on the Mailing List: If you know of someone who is interested in playing field hockey, please let us know and we can add them to our list! Please email both coaches. Varsity Head Coaches Coach Hoh- [email protected] Coach Grady- [email protected] JV Coach TBD Game Schedule: Digitalsports Equipment needed: · Physical Forms · Field Hockey Stick · Mouth Guard · Water Bottle · Shin Guards · Pinnie · Socks or Shin Guard Covers · Sun Screen · Sneakers · Snacks · Cleats · No Jewelry Schedule (If anything