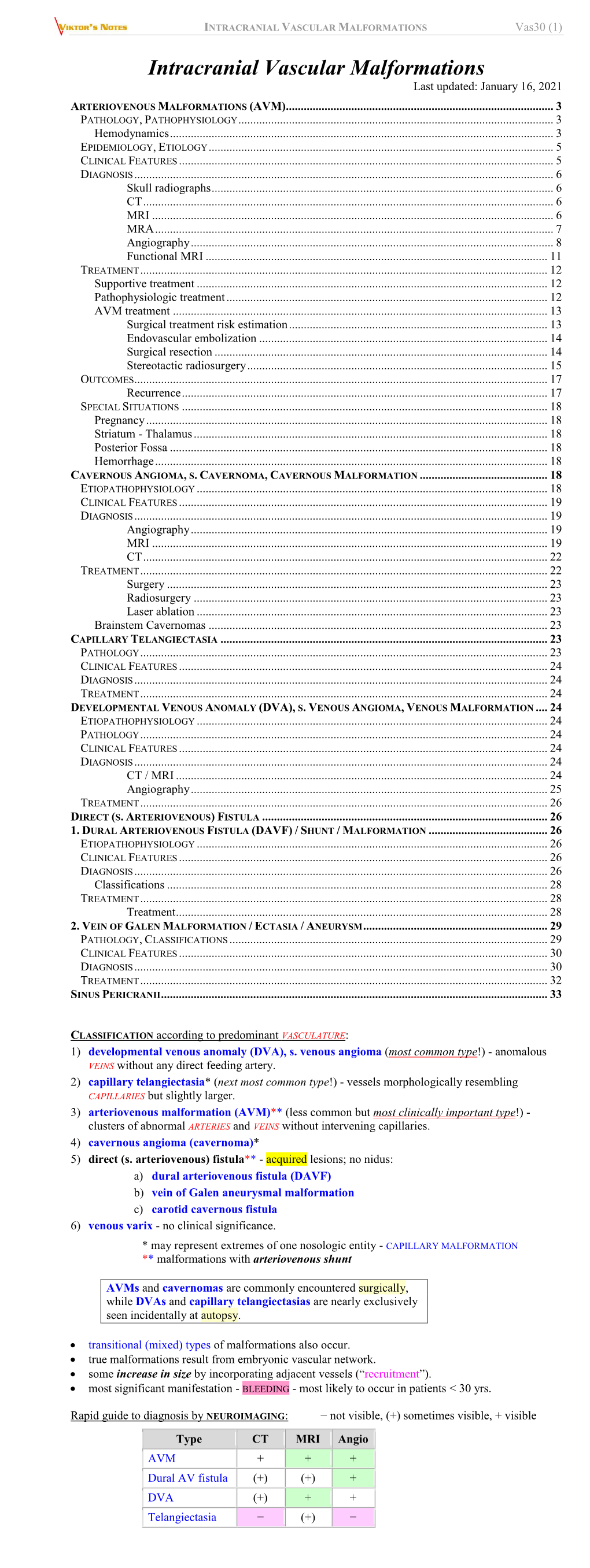
INTRACRANIAL VASCULAR MALFORMATIONS Vas30 (1)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Developmental Venous Anomaly: MR and Angiographic Features
JBR–BTR, 2014, 97: 17-20. DEVELOPMENTAL VENOUS ANOMALY: MR AND ANGIOGRAPHIC FEATURES M. Faure1, M. Voormolen1, T. Van der Zijden1, P.M. Parizel1 Developmental venous anomaly (DVA) is probably the most common anomaly of the intracranial vasculature. DVAs consist of multiple, radially oriented dilated medullary veins that converge into a transcerebral vein. We describe the imaging findings of this vascular anomaly in different patients and the role of different imaging modalities. Key-words: Cerebral blood vessels, abnormalities – Cerebral blood vessels, MR – Cerebral angiography. Developmental venous anomaly (DVA) was first considered a rare vascular malformation (1, 2). Nowa- days, with the advent of Computed Tomography (CT) and especially Magnetic Resonance Imaging (MRI), DVAs are seen every week to month by radiologists (3, 4). Most DVAs are solitary, asymptomatic lesions and are discovered incidentally. They have a relatively benign nature with a low incidence of hemorrhage. When they do bleed, this is thought to be due to associated vascular mal- formations, like cavernous angiomas. The typical angiographic appearance of a DVA is a caput medusae appear- ance in the venous phase. MRI com- bined with MR angiography (MRA) replaces angiography in most un- A B complicated cases as a non-invasive alternative (3, 5). Case reports Case 1 A 32-year-old woman presented with headache, with no particular location and no neurological deficit. MRI of the brain was made in another hospital that showed a flow void running transcerebral, suggestive for a vascular malformation (Fig. 1A,B). Initially, there was no gadolinium contrast given and an arterial feeder could thus not be excluded with MRI. -

Venous Angiomas of the Brain A
- REVIEW ARTICLE systems," Venous angiomas may be Venous angiomas of quite small, draining a limited region of the brain, or may be very large, the brain a sometimes draining an entire hemi- • sphere. They can be single or multi- ple, and even bilateral.P" The com- review monest sites of occurrence are in the frontal and parietal lobes of the cere- venous anomaly' or DVA, pointing bral hemispheres and in the cerebel- Ian C Duncan out that these abnormalities actual- Ium.':" They can also be found in the ly represented an extreme anatomi- FFRad(D)SA occipital and temporal lobes, basal cal variant of the normal venous ganglia and pons." Unitas Interventional Unit POBox 14031 drainage of the brain. Lytlelton Imaging 0140 Pathology The classical radiographic appear- The theory of the development of ance of these abnormalities accurately venous angiomas is that there is fail- reflects the anatomical picture with Introduction ure of regression of normal embryon- multiple enlarged transmedullary Venous angiomas of the brain, also ic transmedullary venous channels. veins radiating in a wedge or radial termed venous malformations or These persistent transmedullary veins pattern toward the larger collecting developmental venous anomalies run axially through the white matter vein producing the pathognomic (DVA) are commonest of the to drain into a single larger calibre col- 'caput medusae' or 'spoke wheel' intracranial vascular malformations lecting venous trunk. The dilated ter- appearance during the venous phase comprising between 50% and 63% of minal collecting vein then penetrates of a cerebral angiogram (Figs 1,2).14,15 all intracranial vascular malforma- the cortex to drain either superficially A similar appearance is often seen on tions. -

Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation
Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation. ФЕДЕРАЛЬНОЕ ГОСУДАРСТВЕННОЕ БЮДЖЕТНОЕ ОБРАЗОВАТЕЛЬНОЕ УЧРЕЖДЕНИЕ ВЫСШЕГО ОБРАЗОВАНИЯ «КУБАНСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» МИНИСТЕРСТВА ЗДРАВООХРАНЕНИЯ РОССИЙСКОЙ ФЕДЕРАЦИИ (ФГБОУ ВО КубГМУ Минздрава России) Кафедра пропедевтики внутренних болезней Department of Propaedeutics of Internal Diseases BASIC CLINICAL SYNDROMES Guidelines for students of foreign (English) students of the 3rd year of medical university Krasnodar 2020 2 УДК 616-07:616-072 ББК 53.4 Compiled by the staff of the department of propaedeutics of internal diseases Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation: assistant, candidate of medical sciences M.I. Bocharnikova; docent, c.m.s. I.V. Kryuchkova; assistent E.A. Kuznetsova; assistent, c.m.s. A.T. Nepso; assistent YU.A. Solodova; assistent D.I. Panchenko; docent, c.m.s. O.A. Shevchenko. Edited by the head of the department of propaedeutics of internal diseases FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation docent A.Yu. Ionov. Guidelines "The main clinical syndromes." - Krasnodar, FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation, 2019. – 120 p. Reviewers: Head of the Department of Faculty Therapy, FSBEI HE KubSMU of the Ministry of Health of Russia Professor L.N. Eliseeva Head of the Department -

Recurrent Bleeding from Cutaneous Venous Collaterals in Portal Hypertension
Gut: first published as 10.1136/gut.29.9.1279 on 1 September 1988. Downloaded from Gut, 1988, 29, 1279-1281 Recurrent bleeding from cutaneous venous collaterals in portal hypertension H R VAN BUUREN, T E FICK, AND S W SCHALM From the Departments ofInternal Medicine and Surgery, University Hospital Dijkzigt, Rotterdam, The Netherlands SUMMARY In portal hypertension, three types of cutaneous portosystemic collaterals may develop: the 'classical' caput Medusae, enterostomal varices and scar or adhesion-related abdominal collaterals. Two patients were treated with severe and recurrent bleeding from adhesion-related collaterals, a complication not reported previously. In the first patient bleeding was only controlled by mesocaval shunt operation; the second patient suffered no further recurrence after local sclerotherapy. Portal hypertension is characterised by the develop- colon with abscess formation. The continuity of the ment of splanchnic systemic venous connections that colon was restored six months later. decompress the portal venous system. Although this On physical examination a caput Medusae like is a protective adaptation, several pathological cutaneous venous pattern with a tiny bleeding spot conditions, such as hepatic encephalopathy and was seen originating from a midline abdominal http://gut.bmj.com/ pulmonary hypertension,' can be associated with surgical scar. Local ligation was done but within two the collateral blood flow. The most important is weeks three recurrent haemorrhages necessitated a gastrointestinal haemorrhage, usually from oeso- local pressure bandage, transfusion of 5 units of phagogastric varices but occasionally from varices blood and repeated local ligations. Again, bleeding elsewhere in the intestinal or biliary tract.2 More- recurred two weeks later. -

Caput Medusae in Alcoholic Liver Disease
case report © Borgis CAPUT MEDUSAE IN ALCOHOLIC LIVER DISEASE – CASE REPORT *Konrad Wroński1, 2 1Faculty of Medicine, Department of Oncology, University of Warmia and Mazury, Olsztyn, Poland Head of Department: prof. Sergiusz Nawrocki, MD, PhD 2Department of Surgical Oncology, Hospital Ministry of Internal Affairs with Warmia and Mazury Oncology Centre, Olsztyn, Poland Head of Department: Andrzej Lachowski, MD Summary Caput medusae is the symptom of portal hypertension due to cirrhosis of liver. This symptom is encountered in medical practice less and less due to earlier diagnostic and effective treatment of portal hypertension. In this article the author present a case of a man who reported to the hospital because of huge ascites due to cirrhosis of liver. After draining ascitic fluid the symptom of caput medusae was observed. Key words: caput medusae, chronic liver disease, alcohol INTRODUCTION Caput medusae is the symptom of portal hyper- tension due to cirrhosis of liver (1-3). This symptom is encountered in medical practice less and less due to earlier diagnostic and effective treatment of portal hy- pertension (1, 4, 5). CASE REPORT A 53-year-old man, Caucasian race, was admitted to the hospital because of the huge ascites and gen- eral destruction. He had history of alcohol consumption about 80-120 gram/day for 20 years and he was heavy smoker – 20 cigarette/day for 20 years. The patient had suffered from cirrhosis of the liver for 5 years. Serology for viral hepatitis B and C were negative. During pal- Fig. 1. Dilated superficial epigastric veins radiating from pable examination, drew attention to the huge ascites a umbilical large venous varix. -

Caput Medusae
BMJ Case Reports: first published as 10.1136/bcr.03.2010.2795 on 6 December 2010. Downloaded from Images in... Caput medusae Nishith K Singh, Usman Cheema, Ali Khalil Department of Internal Medicine, Southern Illinois University School of Medicine, Springfield, Illinois, USA Correspondence to Nishith K Singh, [email protected] A 57-year-old female with significant alcohol exposure, originating from the left side of the portal vein. It coursed hepatitis C and liver cirrhosis was admitted for manage- through the falciform ligament towards the epigastric ment of dehydration and anaemia. On examination she had abdominal wall to empty into a large varix (figure 2). Supe- spider angiomas, a palpable firm left lobe of the liver and rior and inferior epigastric veins from the varix then drained clubbing. Dilated tortuous superficial epigastric veins (caput into the axillary and femoral veins, respectively, forming medusae, figure 1) were noted above the umbilicus radiat- porto-systemic circulation. ing from a central large venous varix like snakes emerging from Medusa's head. So far, none of the onlookers have turned into stone! Competing interests None. A review of the patient's recent CT of the abdomen Patient consent Obtained. revealed a large recanalised paraumbilical vein (figure 2) http://casereports.bmj.com/ on 23 September 2021 by guest. Protected copyright. Figure 1 Dilated superficial (superior and inferior) epigastric veins radiating from a central large venous varix. BMJ Case Reports 2010; doi:10.1136/bcr.03.2010.2795 1of2 BMJ Case Reports: first published as 10.1136/bcr.03.2010.2795 on 6 December 2010. -

Complications of Liver Cirrhosis
GNT block Dec 2019 Complications of liver cirrhosis Complications of liver cirrhosis Objectives Recognize the major complications of cirrhosis Understand the pathogenetic mechanisms underlying the occurrence of the complications Recognize the clinical features inherent to the above mentioned complications Describe the pathological findings of the different complications . Complications of liver cirrhosis 1. Portal hypertension: a. Splenomegaly b. Variceal bleeding c. Hemorrhoids d. Periumbilical venous collaterals (caput medusa) 2. Hepatic failure a. Coagulopathy b. Hypoalbuminemia c. Hepatic encephalopathy 3. Ascites 4. Spontaneous bacterial peritonitis 5. Jaundice and cholestasis 6. Hepatorenal syndrome 7. Hyperestrinism in males 8. Hepatocellular carcinoma Complications of liver cirrhosis 1. PORTAL HYPERTENSION: 1. Splenomegaly 2. Portosystemic shunt: A. Variceal bleeding B. Hemorrhoids C. Periumbilical venous collaterals (caput medusa) Complications of liver cirrhosis PORTAL HYPERTENSION: Resistance to blood flow prehepatic, intrahepatic, and posthepatic The dominant intrahepatic cause is cirrhosis (This is accounting for most cases of portal hypertension) Portosystemic shunts develop when blood flow is reversed from the portal to systemic circulation. due to intrasinusoidal hypertension from regenerative nodule compression Complications of liver cirrhosis Splenomegaly: Long-standing congestion may cause congestive splenomegaly (spleen weight may reach up to 1000 gm) The massive splenomegaly may induce hematologic abnormalities -

Collaterals in Portal Hypertension: Anatomy and Clinical Relevance
3881 Review Article Collaterals in portal hypertension: anatomy and clinical relevance Hitoshi Maruyama, Shuichiro Shiina Department of Gastroenterology, Juntendo University, Tokyo, Japan Correspondence to: Hitoshi Maruyama. Department of Gastroenterology, Juntendo University, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan. Email: [email protected]. Abstract: Portal hypertension is a key pathophysiology of chronic liver diseases typified with cirrhosis or noncirrhotic portal hypertension. The development of collateral vessels is a characteristic feature of impaired portal hemodynamics. The paraumbilical vein (PUV), left gastric vein (LGV), posterior gastric vein (PGV), short gastric vein (SGV), splenorenal shunt (SRS), and inferior mesenteric vein (IMV) are major collaterals, and there are some rare collaterals. The degree and hemodynamics of collateral may affect the portal venous circulation and may compensate for the balance between inflow and outflow volume of the liver. Additionally, the development of collateral shows a relation with the liver function reserve and clinical manifestations such as esophageal varices (EV), gastric varices, rectal varices and the other ectopic varices, hepatic encephalopathy, and prognosis. Furthermore, there may be an interrelationship in the development between different collaterals, showing additional influences on the clinical presentations. Thus, the assessment of collaterals may enhance the understanding of the underlying pathophysiology of the condition of patients with portal hypertension. This review article concluded that each collateral has a specific function depending on the anatomy and hemodynamics and is linked with the relative clinical presentation in patients with portal hypertension. Imaging modalities may be essential for the detection, grading and evaluation of the role of collaterals and may help to understand the pathophysiology of the patient condition. -

IROS 2019 Poster Abstracts and Author Index
Interventionell Radiologisches Olbert Symposium POSTER ABSTRACTS AND AUTHOR INDEX Berlin, 10.–12.1.2019 Transnatonal Congress of the German, Austrian and Swss Societes of Interventonal Radiology (DeGIR, ÖGIR & SSVIR) Online Publicaton Number: 10.1007/s00270-018-2121-y S2 Poster Abstracts P-1 (301.1) be “off-label”. Goal of this retrospective analysis is to assess safety and efficacy of the “off-label” use of the Outcome of DEB and PTA post stenting in occluded Angio-Seal closure device. versus stenotic lesions including evaluation of the implanted stent – subgroup analysis of the randomized Material and methods: The use of 6F and 8F Angio-Seal Freeway Stent Study devices in 471 consecutive patients was evaluated. Indi- cations, puncture technique and patient characteristics J. Tacke1, K. Hausegger2, S. Müller-Hülsbeck3, including coagulation state were recorded. Outcome H. Schroeder4, S. Stahnke5, J. Dambach5; 1Passau/DE, was monitored using data from the institutional compli- 2Klagenfurt/AT, 3Flensburg/DE, 4Berlin/DE, 5Bonn/DE cation management system and patient records. Results Purpose: Stents are needed in up to 50 % of all periphe- were statistically analyzed. ral interventions where PTA with plain or drug-eluting Results: In 94 patients devices were used in one or more balloons alone will not reopen the vessel sufficiently. off-label indications, including oversize puncture (n=31), Nevertheless, the restenosis rate of stents is still a major thrombolysis for more than 24h (n=44), recurrent arterial limitation of peripheral arterial interventions. Drug-elu- punctures within 90 days (n=7), superficial femoral ar- ting balloons (DEB) potentially overcome the problem of tery puncture (n=7) and coagulation disorders (n=13). -

Blood Vessels Chapter 9 Basic Robbins Chapter 11 Big Robbins M
Blood Vessels Chapter 9 Basic Robbins Chapter 11 Big Robbins M. E. Bauman, MD Structure and Function of Blood Vessels Intima (figure 9-1) Internal elastic lamina Media External elastic media Adventitia Vasa vasorum: Vascular Organization Large elastic arteries→small arteries→arterioles→capillaries→postcapillary venules→veins Pericytes Lymphatics Endothelial Cells Continuous lining of entire vascular tree Interendothelial junctions Fenestrations Blood vessels page 2 Blood-brain barrier Endothelial activation (figure 9-2) Endothelial dysfunction Vascular Smooth Muscle Cells Congenital Anomalies Saccular (berry) aneurysms : see aneurysm section below Arteriovenous fistulae (fistulas) (figure 22-11) Jill Bolte Taylor: My Stroke of Insight Fibromuscular dysplasia (Figures not in book) Blood vessels page 3 Blood Pressure Regulation BP = Cardiac Output X Peripheral Resistance (figure 9-3) Renin ACE Angiotensinogen → Angiotensin I → Angiotensin II Vasodilators Adrenal aldosterone Atrial natriuretic peptides (figure 9-4) Hypertensive Vascular Disease Epidemiology of Hypertension “140/90 mm Hg” Morbidity increases with other cardiovascular risk factors “Malignant hypertension” “Essential hypertension” Mechanisms Blood vessels page 4 Morphology (figure 9-5) Hyaline arteriolosclerosis Nephrosclerosis Hyperplastic arteriolosclerosis Vascular Wall Response to Injury Etiologies of vascular injury Responses to vascular injury (figure 9-6) Stenosis = Arteriosclerosis Arteriolosclerosis (see above) Mönckeberg medial sclerosis (figure not in book) Blood -
Mesenteric Angiography with Intervention for Chronic Portal Vein Occlusion
Mesenteric Angiography with Intervention for Chronic Portal Vein Occlusion Janelle Korf 1/17/2020 RAD 3030 Diagnostic Radiology Elective Dr. Zagum Bhatti Clinical History CC: Abdominal Pain 45 yo F PMHx: HTN, Obesity, Gastric Sleeve 2016, PCOS, Endometriosis on OCPs/Spironolactone for >20years, and chronic anemia ROS: • RUQ pain 1 year, worse when bending down • Fatigue x3 months • Denies jaundice, confusion, hematemesis, melena, or hematochezia McGovern Medical School Clinical History Sx: Denies history of tobacco or alcohol abuse FHx: Factor V Leiden Physical Exam: Vitals all in normal limits BMI 28.1 General: AOx3, NAD Abdomen: +BS, depressible, TTP in RUQ, no caput medusae Skin: No petechiae or large ecchymosis, no jaundice McGovern Medical School HPI • PCP diagnosed pt with anemia • Referred to hematology • Started on B12 IM, Folate, and Fe-infusions, with no symptom improvement • Imaging conducted at outside hospital McGovern Medical School CT w/ Contrast Coronal View Spleen Liver Ascending Colon McGovern Medical School Liver Splenic Flexure Mesentery Cavernous Transformation McGovern Medical School CT w/ Con Axial Cavernous Transformation Portal Vein A IVC Liver Spleen McGovern Medical School https://www.intechopen.com/books/what- should-we-know-about-prevented-diagnostic- and-interventional-therapy-in-coronary-artery- disease/percutaneous-recanalization-of- chronic-total-occlusion-cto-coronary-arteries- looking-back-and-moving McGovern Medical School https://www.scienced irect.com/topics/neur oscience/portal- venous-pressure McGovern -

View the 2019 Index
Index A Abnormal uterine bleeding (AUB), heart failure, 311 Achondroplasia, 454 A-a gradient 618, 619 hypertension, 319 chromosome disorder, 64 in elderly, 654 adenomyosis, 634 naming convention for, 253 endochondral ossification in, 450 with hypoxemia, 654, 655 anemia with, 410 preload/afterload effects, 282 inheritance, 60 restrictive lung disease, 661 Asherman syndrome, 634 teratogenicity, 600 AChR (acetylcholine receptor), 229 Abacavir, 201, 203 leiomyoma (fibroid), 634 Acetaldehyde, 72 Acid-base physiology, 580 Abciximab, 122 polyps (endometrial), 634 Acetaldehyde dehydrogenase, 70, 72 Acidemia, 580 Glycoprotein IIb/IIIa inhibitors, thecoma, 632 Acetaminophen, 474 diuretic effect on, 595 429 ABO blood classification, 397 vs. aspirin for pediatric patients, 474 Acid-fast oocysts, 177 thrombogenesis and, 403 newborn hemolysis, 397 free radical injury and, 210 Acid-fast organisms, 125, 140, 155 Abdominal aorta, 357 Abruptio placentae, 626 hepatic necrosis from, 249 Acidic amino acids, 81 atherosclerosis in, 305, 687 cocaine use, 600 N-acetylcysteine for overdose, 671 Acid maltase, 86 bifurcation of, 649 preeclampsia, 629 for osteoarthritis, 458 Acidosis, 578, 580 Abdominal aortic aneurysm, 306 Abscess, 470 toxicity effects, 474 contractility in, 282 Abdominal colic acute inflammation and, 215 toxicity treatment for, 247 hyperkalemia with, 578 lead poisoning, 411 lung, 670 Acetazolamide, 252, 539, 594 Acid phosphatase in neutrophils, 398 Abdominal pain Absence seizures idiopathic intracranial Acid reflux bacterial peritonitis, 384 characteristics