Dominant LMNA Mutations Can Cause Combined Muscular Dystrophy and Peripheral Neuropathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differential Expression of Two Neuronal Intermediate-Filament Proteins, Peripherin and the Low-Molecular-Mass Neurofilament Prot
The Journal of Neuroscience, March 1990, fO(3): 764-764 Differential Expression of Two Neuronal Intermediate-Filament Proteins, Peripherin and the Low-Molecular-Mass Neurofilament Protein (NF-L), During the Development of the Rat Michel Escurat,’ Karima Djabali,’ Madeleine Gumpel,2 Franqois Gras,’ and Marie-Madeleine Portier’ lCollBne de France, Biochimie Cellulaire, 75231 Paris Cedex 05, France, *HBpital de la Salpktricke, Unite INSERM 134, 75651Paris Cedex 13, France The expression of peripherin, an intermediate filament pro- and Freeman, 1978), now more generally referred to respectively tein, had been shown by biochemical methods to be local- as high-, middle-, and low-molecular-mass NFP (NF-H, NF-M, ized in the neurons of the PNS. Using immunohistochemical and NF-L). These proteins are expressed in most mature neu- methods, we analyzed this expression more extensively dur- ronal populations belonging either to the CNS or to the PNS; ing the development of the rat and compared it with that of developing neurons generally do not express any of them until the low-molecular-mass neurofilament protein (NF-L), which they become postmitotic (Tapscott et al., 198 la). is expressed in every neuron of the CNS and PNS. We, however, described another IFP with a molecular weight The immunoreactivity of NF-L is first apparent at the 25 of about 57 kDa, which we had first observed in mouse neu- somite stage (about 11 d) in the ventral horn of the spinal roblastoma cell lines and which was also expressed in rat pheo- medulla and in the posterior part of the rhombencephalon. chromocytoma PC1 2 cell line. -

Lamin-Related Congenital Muscular Dystrophy Alters Mechanical Signaling and Skeletal Muscle Growth
International Journal of Molecular Sciences Article Lamin-Related Congenital Muscular Dystrophy Alters Mechanical Signaling and Skeletal Muscle Growth Daniel J. Owens 1,2 , Julien Messéant 1, Sophie Moog 3, Mark Viggars 2, Arnaud Ferry 1,4, Kamel Mamchaoui 1,5, Emmanuelle Lacène 5 , Norma Roméro 5,6, Astrid Brull 1 , Gisèle Bonne 1 , Gillian Butler-Browne 1 and Catherine Coirault 1,* 1 Center for Research in Myology, Sorbonne Université, INSERM UMRS_974, 75013 Paris, France; [email protected] (D.J.O.); [email protected] (J.M.); [email protected] (A.F.); [email protected] (K.M.); [email protected] (A.B.); [email protected] (G.B.); [email protected] (G.B.-B.) 2 Research Institute for Sport and Exercise Science, Liverpool John Moores University, Liverpool L3 3AF, UK; [email protected] 3 Inovarion, 75005 Paris, France; [email protected] 4 Université de Paris, 75006 Paris, France 5 Neuromuscular Morphology Unit, Institute of Myology, Pitié-Salpêtrière Hospital, 75013 Paris, France; [email protected] (E.L.); [email protected] (N.R.) 6 APHP, Reference Center for Neuromuscular Disorders, Pitié-Salpêtrière Hospital, Institute of Myology, 75013 Paris, France * Correspondence: [email protected]; Tel.: +33-1-1-4216-5708 Abstract: Laminopathies are a clinically heterogeneous group of disorders caused by mutations in the LMNA gene, which encodes the nuclear envelope proteins lamins A and C. The most frequent diseases associated with LMNA mutations are characterized by skeletal and cardiac involvement, and include autosomal dominant Emery–Dreifuss muscular dystrophy (EDMD), limb-girdle muscular Citation: Owens, D.J.; Messéant, J.; dystrophy type 1B, and LMNA-related congenital muscular dystrophy (LMNA-CMD). -

ARVC-Variants.Pdf
Updated gene list responsible for ARVC/D pathology Subtype Gene Location Reference ARVC1 TGFB3 14q24.3 Beffagna G, Occhi G, Nava A, et al. Regulatory mutations in transforming growth factor-beta3 gene cause arrhythmogenic right ventricular cardiomyopathy type 1. Cardiovasc Res. 2005;65:366–73. ARVC2 RYR2 1q43 Tiso N, Stephan DA, Nava A, et al. Identification of mutations in the cardiac ryanodine receptor gene in families affected with arrhythmogenic right ventricular cardiomyopathy type 2 (ARVD2). Hum Mol Genet. 2001;10:189–94. ARVC3 Unknown 14q12-q22 Severini GM, Krajinovic M, Pinamonti B, et al. A new locus for arrhythmogenic right ventricular dysplasia on the long arm of chromosome 14. Genomics. 1996;31:193–200. ARVC4 TTN 2q32.1-q32.3 Taylor M, Graw S, Sinagra G, et al. Genetic variation in titin in arrhythmogenic right ventricular cardiomyopathy-overlap syndromes. Circulation. 2011;124:876–85. ARVC5 TMEM43 3p25.1 Merner ND, Hodgkinson KA, Haywood AF, et al. Arrhythmogenic right ventricular cardiomyopathy type 5 is a fully penetrant, lethal arrhythmic disorder caused by a missense mutation in the TMEM43 gene. Am J Hum Genet. 2008;82:809–21. ARVC6 Unknown 10p14-p12 Li D, Ahmad F, Gardner MJ, et al. The locus of a novel gene responsible for arrhythmogenic right- ventricular dysplasia characterized by early onset and high penetrance maps to chromosome 10p12-p14. Am J Hum Genet. 2000;66:148–56. ARVC7 DES 2q35 Klauke B, Kossmann S, Gaertner A, et al. De novo desmin-mutation N116S is associated with arrhythmogenic right ventricular cardiomyopathy. Hum Mol Genet. 2010;19:4595–607. -

Genetic Mutations and Mechanisms in Dilated Cardiomyopathy
Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, … , Jessica R. Golbus, Megan J. Puckelwartz J Clin Invest. 2013;123(1):19-26. https://doi.org/10.1172/JCI62862. Review Series Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of congestive heart failure. In hypertrophic cardiomyopathy (HCM), cardiac output is limited by the thickened myocardium through impaired filling and outflow. Mutations in the genes encoding the thick filament components myosin heavy chain and myosin binding protein C (MYH7 and MYBPC3) together explain 75% of inherited HCMs, leading to the observation that HCM is a disease of the sarcomere. Many mutations are “private” or rare variants, often unique to families. In contrast, dilated cardiomyopathy (DCM) is far more genetically heterogeneous, with mutations in genes encoding cytoskeletal, nucleoskeletal, mitochondrial, and calcium-handling proteins. DCM is characterized by enlarged ventricular dimensions and impaired systolic and diastolic function. Private mutations account for most DCMs, with few hotspots or recurring mutations. More than 50 single genes are linked to inherited DCM, including many genes that also link to HCM. Relatively few clinical clues guide the diagnosis of inherited DCM, but emerging evidence supports the use of genetic testing to identify those patients at risk for faster disease progression, congestive heart failure, and arrhythmia. Find the latest version: https://jci.me/62862/pdf Review series Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, Jessica R. Golbus, and Megan J. Puckelwartz Department of Human Genetics, University of Chicago, Chicago, Illinois, USA. Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of conges- tive heart failure. -

Nuclear Titin Interacts with A- and B-Type Lamins in Vitro and in Vivo
Research Article 239 Nuclear Titin interacts with A- and B-type lamins in vitro and in vivo Michael S. Zastrow1,*, Denise B. Flaherty2‡, Guy M. Benian2 and Katherine L. Wilson1,§ 1Department of Cell Biology, The Johns Hopkins University School of Medicine, 725 N. Wolfe St, Baltimore, MD 21205, USA 2Department of Pathology, Emory University, Whitehead Biomedical Research Building, Atlanta, GA 30332, USA *Present address: Department of Developmental Biology, Stanford University School of Medicine, Beckman Center, B300, 279 Campus Drive, Stanford, CA 94305, USA ‡Department of Biology, Eckerd College, SHB 105, 4200 54th Ave, St Petersburg, FL 33711, USA §Author for correspondence (e-mail: [email protected]) Accepted 4 October 2005 Journal of Cell Science 119, 239-249 Published by The Company of Biologists 2006 doi:10.1242/jcs.02728 Summary Lamins form structural filaments in the nucleus. Mutations lamin-downregulated [lmn-1(RNAi)] embryos, Ce-titin was in A-type lamins cause muscular dystrophy, undetectable at the nuclear envelope suggesting its cardiomyopathy and other diseases, including progeroid localization or stability requires Ce-lamin. In human cells syndromes. To identify new binding partners for lamin A, (HeLa), antibodies against the titin-specific domain M-is6 we carried out a two-hybrid screen with a human skeletal- gave both diffuse and punctate intranuclear staining by muscle cDNA library, using the Ig-fold domain of lamin A indirect immunofluorescence, and recognized at least three as bait. The C-terminal region of titin was recovered twice. bands larger than 1 MDa in immunoblots of isolated HeLa Previous investigators showed that nuclear isoforms of titin nuclei. -

Tubulin: Are They Linced?
cells Review Microtubular and Nuclear Functions of γ-Tubulin: Are They LINCed? Jana Chumová, Hana Kourová, Lucie Trögelová, Petr Halada and Pavla Binarová * Institute of Microbiology of the Czech Academy of Sciences, Vídeˇnská 1083, 142 20 Prague, Czech Republic; [email protected] (J.C.); [email protected] (H.K.); [email protected] (L.T.); [email protected] (P.H.) * Correspondence: [email protected]; Tel.: +420-241-062-130 Received: 8 February 2019; Accepted: 14 March 2019; Published: 19 March 2019 Abstract: γ-Tubulin is a conserved member of the tubulin superfamily with a function in microtubule nucleation. Proteins of γ-tubulin complexes serve as nucleation templates as well as a majority of other proteins contributing to centrosomal and non-centrosomal nucleation, conserved across eukaryotes. There is a growing amount of evidence of γ-tubulin functions besides microtubule nucleation in transcription, DNA damage response, chromatin remodeling, and on its interactions with tumor suppressors. However, the molecular mechanisms are not well understood. Furthermore, interactions with lamin and SUN proteins of the LINC complex suggest the role of γ-tubulin in the coupling of nuclear organization with cytoskeletons. γ-Tubulin that belongs to the clade of eukaryotic tubulins shows characteristics of both prokaryotic and eukaryotic tubulins. Both human and plant γ-tubulins preserve the ability of prokaryotic tubulins to assemble filaments and higher-order fibrillar networks. γ-Tubulin filaments, with bundling and aggregating capacity, are suggested to perform complex scaffolding and sequestration functions. In this review, we discuss a plethora of γ-tubulin molecular interactions and cellular functions, as well as recent advances in understanding the molecular mechanisms behind them. -

Lamin A/C Cardiomyopathy: Implications for Treatment
Current Cardiology Reports (2019) 21:160 https://doi.org/10.1007/s11886-019-1224-7 MYOCARDIAL DISEASE (A ABBATE AND G SINAGRA, SECTION EDITORS) Lamin A/C Cardiomyopathy: Implications for Treatment Suet Nee Chen1 & Orfeo Sbaizero1,2 & Matthew R. G. Taylor1 & Luisa Mestroni1 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review The purpose of this review is to provide an update on lamin A/C (LMNA)-related cardiomyopathy and discuss the current recommendations and progress in the management of this disease. LMNA-related cardiomyopathy, an inherited autosomal dominant disease, is one of the most common causes of dilated cardiomyopathy and is characterized by steady progression toward heart failure and high risks of arrhythmias and sudden cardiac death. Recent Findings We discuss recent advances in the understanding of the molecular mechanisms of the disease including altered cell biomechanics, which may represent novel therapeutic targets to advance the current management approach, which relies on standard heart failure recommendations. Future therapeutic approaches include repurposed molecularly directed drugs, siRNA- based gene silencing, and genome editing. Summary LMNA-related cardiomyopathy is the focus of active in vitro and in vivo research, which is expected to generate novel biomarkers and identify new therapeutic targets. LMNA-related cardiomyopathy trials are currently underway. Keywords Lamin A/C gene . Laminopathy . Heart failure . Arrhythmias . Mechanotransduction . P53 . CRISPR–Cas9 therapy Introduction functions, including maintaining nuclear structural integrity, regulating gene expression, mechanosensing, and Mutations in the lamin A/C gene (LMNA)causelaminopathies, mechanotransduction through the lamina-associated proteins a heterogeneous group of inherited disorders including muscu- [6–11]. -

Lamin A/C: Function in Normal and Tumor Cells
cancers Review Lamin A/C: Function in Normal and Tumor Cells Niina Dubik and Sabine Mai * Department of Physiology and Pathophysiology, University of Manitoba, Winnipeg, MB R3E0V9, Canada; [email protected] * Correspondence: [email protected] Received: 9 November 2020; Accepted: 8 December 2020; Published: 9 December 2020 Simple Summary: The aim of this review is to summarize lamin A/C’s currently known functions in both normal and diseased cells. Lamin A/C is a nuclear protein with many functions in cells, such as maintaining a cell’s structural stability, cell motility, mechanosensing, chromosome organization, gene regulation, cell differentiation, DNA damage repair, and telomere protection. Mutations of the lamin A/C gene, incorrect processing of the protein, and lamin A/C deregulation can lead to various diseases and cancer. This review touches on diseases caused by mutation and incorrect processing of lamin A/C, called laminopathies. The effect of lamin A/C deregulation in cancer is also reviewed, and lamin A/C’s potential in helping to diagnose prostate cancers more accurately is discussed. Abstract: This review is focused on lamin A/C, a nuclear protein with multiple functions in normal and diseased cells. Its functions, as known to date, are summarized. This summary includes its role in maintaining a cell’s structural stability, cell motility, mechanosensing, chromosome organization, gene regulation, cell differentiation, DNA damage repair, and telomere protection. As lamin A/C has a variety of critical roles within the cell, mutations of the lamin A/C gene and incorrect processing of the protein results in a wide variety of diseases, ranging from striated muscle disorders to accelerated aging diseases. -

Hippocampal LMNA Gene Expression Is Increased in Late-Stage Alzheimer’S Disease
International Journal of Molecular Sciences Article Hippocampal LMNA Gene Expression is Increased in Late-Stage Alzheimer’s Disease Iván Méndez-López 1,2,*,†, Idoia Blanco-Luquin 1,†, Javier Sánchez-Ruiz de Gordoa 1,3, Amaya Urdánoz-Casado 1, Miren Roldán 1, Blanca Acha 1, Carmen Echavarri 1,4, Victoria Zelaya 5, Ivonne Jericó 3 and Maite Mendioroz 1,3,* 1 Neuroepigenetics Laboratory-Navarrabiomed, Complejo Hospitalario de Navarra, Universidad Pública de Navarra (UPNA), IdiSNA (Navarra Institute for Health Research), Pamplona, Navarra 31008, Spain; [email protected] (I.B.-L.); [email protected] (J.S.-R.d.G.); [email protected] (A.U.-C.); [email protected] (M.R.); [email protected] (B.A.); [email protected] (C.E.) 2 Department of Internal Medicine, Hospital García Orcoyen, Estella 31200, Spain 3 Department of Neurology, Complejo Hospitalario de Navarra- IdiSNA (Navarra Institute for Health Research), Pamplona, Navarra 31008, Spain; [email protected] 4 Hospital Psicogeriátrico Josefina Arregui, Alsasua, Navarra 31800, Spain 5 Department of Pathology, Complejo Hospitalario de Navarra- IdiSNA (Navarra Institute for Health Research), Pamplona, Navarra 31008, Spain; [email protected] * Correspondence: [email protected] (I.M.-L.); [email protected] (M.M.); Tel.: +34-848-422677 (I.M.-L.) † These authors contributed equally to this work. Received: 30 November 2018; Accepted: 14 February 2019; Published: 18 February 2019 Abstract: Lamins are fibrillary proteins that are crucial in maintaining nuclear shape and function. Recently, B-type lamin dysfunction has been linked to tauopathies. However, the role of A-type lamin in neurodegeneration is still obscure. -

Deficiencies in Lamin B1 and Lamin B2 Cause Neurodevelopmental Defects and Distinct Nuclear Shape Abnormalities in Neurons
M BoC | ARTICLE Deficiencies in lamin B1 and lamin B2 cause neurodevelopmental defects and distinct nuclear shape abnormalities in neurons Catherine Coffiniera, Hea-Jin Jungb, Chika Nobumoria, Sandy Changa, Yiping Tua, Richard H. Barnes IIa, Yuko Yoshinagac, Pieter J. de Jongc, Laurent Vergnesd, Karen Reued, Loren G. Fonga, and Stephen G. Younga,d aDepartment of Medicine and bMolecular Biology Institute, University of California, Los Angeles, Los Angeles, CA 90095; cChildren’s Hospital Oakland Research Institute, Oakland, CA 94609; dDepartment of Human Genetics, David Geffen School of Medicine, University of California, Los Angeles, Los Angeles, CA 90095 ABSTRACT Neuronal migration is essential for the development of the mammalian brain. Monitoring Editor Here, we document severe defects in neuronal migration and reduced numbers of neurons in Thomas Michael Magin lamin B1–deficient mice. Lamin B1 deficiency resulted in striking abnormalities in the nuclear University of Leipzig shape of cortical neurons; many neurons contained a solitary nuclear bleb and exhibited an Received: Jun 13, 2011 asymmetric distribution of lamin B2. In contrast, lamin B2 deficiency led to increased numbers Revised: Sep 9, 2011 of neurons with elongated nuclei. We used conditional alleles for Lmnb1 and Lmnb2 to create Accepted: Sep 23, 2011 forebrain-specific knockout mice. The forebrain-specificLmnb1- and Lmnb2-knockout models had a small forebrain with disorganized layering of neurons and nuclear shape abnormalities, similar to abnormalities identified in the conventional knockout mice. A more severe pheno- type, complete atrophy of the cortex, was observed in forebrain-specific Lmnb1/Lmnb2 double-knockout mice. This study demonstrates that both lamin B1 and lamin B2 are essential for brain development, with lamin B1 being required for the integrity of the nuclear lamina, and lamin B2 being important for resistance to nuclear elongation in neurons. -

Doubly Heterozygous LMNA and TTN Mutations Revealed by Exome Sequencing in a Severe Form of Dilated Cardiomyopathy
European Journal of Human Genetics (2013) 21, 1105–1111 & 2013 Macmillan Publishers Limited All rights reserved 1018-4813/13 www.nature.com/ejhg ARTICLE Doubly heterozygous LMNA and TTN mutations revealed by exome sequencing in a severe form of dilated cardiomyopathy Roberta Roncarati1,2, Chiara Viviani Anselmi2, Peter Krawitz3,4,5, Giovanna Lattanzi6, Yskert von Kodolitsch7, Andreas Perrot8,9, Elisa di Pasquale2,10, Laura Papa2, Paola Portararo2, Marta Columbaro6, Alberto Forni11, Giuseppe Faggian*,11, Gianluigi Condorelli*,1,12 and Peter N Robinson*,3,4,5 Familial dilated cardiomyopathy (DCM) is a heterogeneous disease; although 30 disease genes have been discovered, they explain only no more than half of all cases; in addition, the causes of intra-familial variability in DCM have remained largely unknown. In this study, we exploited the use of whole-exome sequencing (WES) to investigate the causes of clinical variability in an extended family with 14 affected subjects, four of whom showed particular severe manifestations of cardiomyopathy requiring heart transplantation in early adulthood. This analysis, followed by confirmative conventional sequencing, identified the mutation p.K219T in the lamin A/C gene in all 14 affected patients. An additional variant in the gene for titin, p.L4855F, was identified in the severely affected patients. The age for heart transplantation was substantially less for LMNA:p.K219T/ TTN:p.L4855F double heterozygotes than that for LMNA:p.K219T single heterozygotes. Myocardial specimens of doubly heterozygote individuals showed increased nuclear length, sarcomeric disorganization, and myonuclear clustering compared with samples from single heterozygotes. In conclusion, our results show that WES can be used for the identification of causal and modifier variants in families with variable manifestations of DCM. -
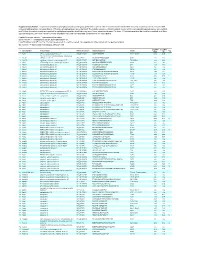
Supplementary Table 1
Supplementary Table 1. Large-scale quantitative phosphoproteomic profiling was performed on paired vehicle- and hormone-treated mTAL-enriched suspensions (n=3). A total of 654 unique phosphopeptides corresponding to 374 unique phosphoproteins were identified. The peptide sequence, phosphorylation site(s), and the corresponding protein name, gene symbol, and RefSeq Accession number are reported for each phosphopeptide identified in any one of three experimental pairs. For those 414 phosphopeptides that could be quantified in all three experimental pairs, the mean Hormone:Vehicle abundance ratio and corresponding standard error are also reported. Peptide Sequence column: * = phosphorylated residue Site(s) column: ^ = ambiguously assigned phosphorylation site Log2(H/V) Mean and SE columns: H = hormone-treated, V = vehicle-treated, n/a = peptide not observable in all 3 experimental pairs Sig. column: * = significantly changed Log 2(H/V), p<0.05 Log (H/V) Log (H/V) # Gene Symbol Protein Name Refseq Accession Peptide Sequence Site(s) 2 2 Sig. Mean SE 1 Aak1 AP2-associated protein kinase 1 NP_001166921 VGSLT*PPSS*PK T622^, S626^ 0.24 0.95 PREDICTED: ATP-binding cassette, sub-family A 2 Abca12 (ABC1), member 12 XP_237242 GLVQVLS*FFSQVQQQR S251^ 1.24 2.13 3 Abcc10 multidrug resistance-associated protein 7 NP_001101671 LMT*ELLS*GIRVLK T464, S468 -2.68 2.48 4 Abcf1 ATP-binding cassette sub-family F member 1 NP_001103353 QLSVPAS*DEEDEVPVPVPR S109 n/a n/a 5 Ablim1 actin-binding LIM protein 1 NP_001037859 PGSSIPGS*PGHTIYAK S51 -3.55 1.81 6 Ablim1 actin-binding