Smallpox in Countries Non-Endemic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EC06-1255 List and Description of Named Cultivars in the Genus Penstemon Dale T
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Historical Materials from University of Nebraska- Extension Lincoln Extension 2006 EC06-1255 List and Description of Named Cultivars in the Genus Penstemon Dale T. Lindgren University of Nebraska-Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/extensionhist Lindgren, Dale T., "EC06-1255 List and Description of Named Cultivars in the Genus Penstemon" (2006). Historical Materials from University of Nebraska-Lincoln Extension. 4802. https://digitalcommons.unl.edu/extensionhist/4802 This Article is brought to you for free and open access by the Extension at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Historical Materials from University of Nebraska-Lincoln Extension by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. - CYT vert . File NeBrasKa s Lincoln EXTENSION 85 EC1255 E 'Z oro n~ 1255 ('r'lnV 1 List and Description of Named Cultivars in the Genus Penstemon (2006) Cooperative Extension Service Extension .circular Received on: 01- 24-07 University of Nebraska, Lincoln - - Libraries Dale T. Lindgren University of Nebraska-Lincoln 00IANR This is a joint publication of the American Penstemon Society and the University of Nebraska-Lincoln Extension. We are grateful to the American Penstemon Society for providing the funding for the printing of this publication. ~)The Board of Regents oft he Univcrsit y of Nebraska. All rights reserved. Table -

Cy Martin Collection
University of Oklahoma Libraries Western History Collections Cy Martin Collection Martin, Cy (1919–1980). Papers, 1966–1975. 2.33 feet. Author. Manuscripts (1968) of “Your Horoscope,” children’s stories, and books (1973–1975), all written by Martin; magazines (1966–1975), some containing stories by Martin; and biographical information on Cy Martin, who wrote under the pen name of William Stillman Keezer. _________________ Box 1 Real West: May 1966, January 1967, January 1968, April 1968, May 1968, June 1968, May 1969, June 1969, November 1969, May 1972, September 1972, December 1972, February 1973, March 1973, April 1973, June 1973. Real West (annual): 1970, 1972. Frontier West: February 1970, April 1970, June1970. True Frontier: December 1971. Outlaws of the Old West: October 1972. Mental Health and Human Behavior (3rd ed.) by William S. Keezer. The History of Astrology by Zolar. Box 2 Folder: 1. Workbook and experiments in physiological psychology. 2. Workbook for physiological psychology. 3. Cagliostro history. 4. Biographical notes on W.S. Keezer (pen name Cy Martin). 5. Miscellaneous stories (one by Venerable Ancestor Zerkee, others by Grandpa Doc). Real West: December 1969, February 1970, March 1970, May 1970, September 1970, October 1970, November 1970, December 1970, January 1971, May 1971, August 1971, December 1971, January 1972, February 1972. True Frontier: May 1969, September 1970, July 1971. Frontier Times: January 1969. Great West: December 1972. Real Frontier: April 1971. Box 3 Ford Times: February 1968. Popular Medicine: February 1968, December 1968, January 1971. Western Digest: November 1969 (2 copies). Golden West: March 1965, January 1965, May 1965 July 1965, September 1965, January 1966, March 1966, May 1966, September 1970, September 1970 (partial), July 1972, August 1972, November 1972, December 1972, December 1973. -

CHAPTER THIRTY the AFFLUENT SOCIETY Objectives a Thorough Study of Chapter 30 Should Enable the Student to Understand: 1
CHAPTER THIRTY THE AFFLUENT SOCIETY Objectives A thorough study of Chapter 30 should enable the student to understand: 1. The strengths and weaknesses of the economy in the 1950s and early 1960s. 2. The changes in the American lifestyle in the 1 950s. 3. The significance of the Supreme Court’s desegregation decision and the early civil rights movement. 4. The characteristics of Dwight Eisenhower’s middle-of-the-road domestic policy. 5. The new elements of American foreign policy introduced by Secretary of State John Foster Dulles. 6. The causes and results of increasing United States involvement in the Middle East. 7. The sources of difficulties for the United States in Latin America. 8. The reasons for new tensions with the Soviet Union toward the end of the Eisenhower administration. Main Themes 1. That the technological, consumer-oriented society of the 1 950s was remarkably affluent and unified despite the persistence of a less privileged underclass and the existence of a small corps of detractors. 2. How the Supreme Court’s social desegregation decision of 1954 marked the beginning of a civil- rights revolution for American blacks. 3. How President Dwight Eisenhower presided over a business-oriented “dynamic conservatism” that resisted most new reforms without significantly rolling back the activist government programs born in the 1930s. 4. That while Eisenhower continued to allow containment by building alliances, supporting anticommunist regimes, maintaining the arms race, and conducting limited interventions, he also showed an awareness of American limitations and resisted temptations for greater commitments. Glossary 1. Third World A convenient way to refer to all the nations of the world besides the United States, Canada, the Soviet Union, Japan, Australia, New Zealand, Israel, China, and the countries of Europe. -

UC Berkeley Berkeley Planning Journal
UC Berkeley Berkeley Planning Journal Title Economic Development and Housing Policy in Cuba Permalink https://escholarship.org/uc/item/9p00546t Journal Berkeley Planning Journal, 2(1) ISSN 1047-5192 Author Fields, Gary Publication Date 1985 DOI 10.5070/BP32113199 Peer reviewed eScholarship.org Powered by the California Digital Library University of California ECONOMIC DEVELOPMENT AND HOUSING POLICY IN CUBA Gary Fields Introduction Since the triumph of the Cuban Revolution in 1959, Cuba's economic development has been marked by efforts to achieve fo ur basic objectives: I) agrarian reform, including land redistribution, creation of state and cooperative farms, and agricultural crop diversification; 2) economic growth and industrial development, including the siting of new industries and employment opportunities in the countryside; 3) wealth and income redistribution from rich to poor citizens and from urban to rural areas; 4) provision of social services in all areas of the country, including nationwide literacy, access to medical care in the rural areas, and the creation of adequate and affordable housing nationwide. It is important to note that all of these objectives contain an emphasis on rural development. This emphasis was the result of decisions by Cuban economic planners to correct what had been perceived as the most serious ·negative consequence of the Island's economic past--the economic imbalance between town and coun try. 1 The dependence of the Cuban economy on sugar production, with its dramatic seasonal employment shifts, the control of the Island's sugar industry by American companies and the siphoning of sugar profits out of Cuba, the concentration in Havana of the wealth created primarily in the countryside, and the lack of economic opportunities and social services in the rural areas, were the main features of an economic and social system that had impoverished the rural population, creating a movement for change. -

The Munich Massacre: a New History
The Munich Massacre: A New History Eppie Briggs (aka Marigold Black) A thesis submitted in partial fulfilment of the requirements of the degree of BA (Hons) in History University of Sydney October 2011 1 Contents Introduction and Historiography Part I – Quiet the Zionist Rage 1. The Burdened Alliance 2. Domestic Unrest Part II – Rouse the Global Wrath 3. International Condemnation 4. The New Terrorism Conclusion 2 Acknowledgments I would like to thank first and foremost Dr Glenda Sluga to whom I am greatly indebted for her guidance, support and encouragement. Without Glenda‟s sage advice, the writing of this thesis would have been an infinitely more difficult and painful experience. I would also like to thank Dr Michael Ondaatje for his excellent counsel, good-humour and friendship throughout the last few years. Heartfelt thanks go to Elise and Dean Briggs for all their love, support and patience and finally, to Angus Harker and Janie Briggs. I cannot adequately convey the thanks I owe Angus and Janie for their encouragement, love, and strength, and for being a constant reminder as to why I was writing this thesis. 3 Abstract This thesis examines the Nixon administration’s response to the Munich Massacre; a terrorist attack which took place at the 1972 Olympic Games in Munich. By examining the contextual considerations influencing the administration’s response in both the domestic and international spheres, this thesis will determine the manner in which diplomatic intricacies impacted on the introduction of precedent setting counterterrorism institutions. Furthermore, it will expound the correlation between the Nixon administration’s response and a developing conceptualisation of acts of modern international terrorism. -

CREEP [Committee for the Re-Election of the President (Richard M
Series 6: CREEP [Committee for the Re-election of the President (Richard M. Nixon)] Series, 1968-1973; bulk 1971-1972 6.75 cubic feet consisting of 194 folders. The CREEP [Committee for the Re-election of the President (Richard M. Nixon)] Series consists of articles, briefing materials, charts, clippings, correspondence, directories, fact sheets, manuals, lists, memoranda, memorabilia, newsletters, notes, press kits, press releases, reports, schedules, statements and speeches. Materials in this series cover the period 1968-1973, and document Steorts’ work as the Assistant National Director of Volunteers for the political campaign to re-elect Richard M. Nixon to a second term as President. The bulk of the materials date from 1971 to 1972. The series is arranged alphabetically by folder title, and chronologically within each folder. Files regarding volunteers and women speakers contain memoranda, correspondence, projected schedules, recap sheets, notes and charts, a direct mail overview for volunteers and a listing of procedures for letters to volunteers. In addition, there is an outline of the areas of responsibilities, and a brief paper on how the campaign must be predicated on a keen sensitivity to the new self- awareness of women. Some of the topics covered in the memoranda and correspondence include the “Pledged to the President” Volunteer Recruitment Program, a volunteer training film, the “Host for the President” Program, regional field directors, individuals who agreed to speak on behalf of the President during the campaign for the Spokesmen Resources Program, and the schedule of events for the Midwestern Regional Leadership Conference in Chicago. There are lists of speaking events in various states and questions regarding engagement/appearance criteria. -

December 1972
Volume 6, Issue 12 Issued December 14, 1972 monthly statistical report ECONOMY EXPANDS FASTER THAN EXPECTED weather in November, however, marred agricultural UNEMPLOYMENT FINALLY NUDGED DOWN expectations for a highly profitable season. Expectations for a bullish fourth quarter find DISTRICT SAVINGSFALL FROM 1971 PEAKS solid support in recent statistical releases. If anything, BUT REMAIN SUFFICIENT FOR LOAN DEMAND the district’s economy was stronger than anticipated in August and will undoubtedly move into the new Savings inflows continueto provide large supplies of funds to district financial institutions. Consumer- year on an upward swing. type time and savings deposits at district member Perhaps the most welcome sign of improvement: banks increased by a seasonally adjusted 14 percent newly released, adjusted unemployment figures for for the 12 months ending in September 1972. To October show a modest decline to 5.9 percent; the place this increase in perspective, savings inflows grew unemployment rate had been stuck at or above the 6 at a 21 percent seasonally adjusted annual rate in the percent mark in preceding months. Another sign of first quarter of 1971—the record to date. strength: September retail sales equalled August highs Recent growth of savings at district savings and and continued to run about 10 percent ahead of year-earlier figures. banks,loan associationsnevertheless(S&Ls),declinedalthoughfrom a strongerpeak 22 thanpercentat - As expected, the district’s construction sector growth rate in the first quarter of 1971 to a 17 percent remains strong. Seasonally adjusted housing unit au- rate for the 12 months ending in September. thorizations in October were down from September, but were up almost 16 percent from October ‘71. -

Innovator, 1981-04-14 Student Services
Governors State University OPUS Open Portal to University Scholarship Innovator Student Newspapers 4-14-1981 Innovator, 1981-04-14 Student Services Follow this and additional works at: http://opus.govst.edu/innovator Recommended Citation Governors State University Student Services, Innovator (1981, April 14). http://opus.govst.edu/innovator/186 This Newspaper is brought to you for free and open access by the Student Newspapers at OPUS Open Portal to University Scholarship. It has been accepted for inclusion in Innovator by an authorized administrator of OPUS Open Portal to University Scholarship. For more information, please contact [email protected]. THE GOVERNORS STATE UNIVERSITY INNOVATOR CHIVES Volume 7 Number 18 April 14, 1981 VETS URGE ''STOP THE CUTS'' by Jeff Leanna Along with the massive defaults due to the ten year delimiting date befal ling Many GSU student veterans now the Viet Nam era vets, an additional getting financial assistance to pursue factor may hurt veteran enrollment: the their education may find themselves VEAP system, which replaced the Gl without funds this year. And a great Bill as of January 1st, 1977. many more will lose out in fiscal '82. The VEAP, or Veterans Educat ional This in turn, may affect total veteran Assistance Program, is an educat ional enrollment here. benefits system allowing the ser GSU is not the only school to be vicemen to make contributions of up to experiencing this problem . The $2700 of their own pay toward an in nat ional total of vet enrollment may dividual educat ional fund. The service soon drop off sharply as a result of then matches the amount on a two-for factors independent of all the other one basis, thus giving the vet a total of current economic woes. -
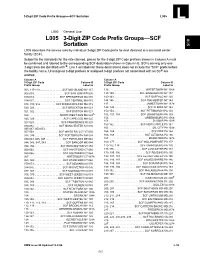
DMM L005 3-Digit ZIP Code Prefix Groups--SCF Sortation
3-Digit ZIP Code Prefix Groups—SCF Sortation L005 L L000 General Use L005 3-Digit ZIP Code Prefix Groups—SCF 005 Sortation L005 describes the service area by individual 3-digit ZIP Code prefix for mail destined to a sectional center facility (SCF). Subject to the standards for the rate claimed, pieces for the 3-digit ZIP Code prefixes shown in Column A must be combined and labeled to the corresponding SCF destination shown in Column B. SCFs serving only one 3-digit area are identified with S; Line 1 on labels for these destinations does not include the “SCF” prefix before the facility name. Unassigned 3-digit prefixes or assigned 3-digit prefixes not associated with an SCF are omitted. Column A Column A 3-Digit ZIP Code Column B 3-Digit ZIP Code Column B Prefix Group Label to Prefix Group Label to 005, 117-119. .SCF MID-ISLAND NY 117 136 . WATERTOWN NY 136S 006-009. SCF SAN JUAN PR 006 137-139. SCF BINGHAMTON NY 137 010-013. SCF SPRINGFIELD MA 010 140-143. .SCF BUFFALO NY 140 014-017. SCF CENTRAL MA 015 144-146. .SCF ROCHESTER NY 144 018, 019, 055 . SCF MIDDLESEX-ESX MA 018 147 . .JAMESTOWN NY 147S 020, 023 . .SCF BROCKTON MA 023 148, 149 . SCF ELMIRA NY 148 021, 022 . SCF BOSTON MA 021 150-154. SCF PITTSBURGH PA 150 024 . NORTHWEST BOS MA 024S 155, 157, 159 . SCF JOHNSTOWN PA 159 025, 026 . SCF CAPE COD MA 025 156 . GREENSBURG PA 156S 158 . DU BOIS PA 158S 027-029. -

Download This Article in PDF Format
A&A 500, 1327–1336 (2009) Astronomy DOI: 10.1051/0004-6361/200911802 & c ESO 2009 Astrophysics Observations of 44 extragalactic radio sources with the VLBA at 92 cm A list of potential calibrators and targets for LOFAR and RadioAstron H. Rampadarath1,2, M. A. Garrett3,2,4, and A. Polatidis1,3 1 Joint Institute for VLBI in Europe (JIVE), Postbus 2, 7990 AA Dwingeloo, The Netherlands e-mail: [rampadarath;polatidis]@astron.nl 2 Sterrewacht Leiden, Leiden University, Oort Building, Neils Bhorweg 2, 2333 CA, Leiden, The Netherlands 3 Netherlands Institute for Radio Astronomy (ASTRON), Postbus 2, 7990 AA Dwingeloo, The Netherlands e-mail: [email protected] 4 Centre for Supercomputing, Swinburne University of Technology, Mail number H39, PO Box 218, Hawthorn, Victoria 3122, Australia Received 5 February 2009 / Accepted 14 March 2009 ABSTRACT Aims. We have analysed VLBA 92 cm archive data of 44 extragalactic sources in order to identify early targets and potential calibrator sources for the LOFAR radio telescope and the RadioAstron space VLBI mission. Some of these sources will also be suitable as “in- beam” calibrators, permitting deep, wide-field studies of other faint sources in the same field of view. Methods. All publicly available VLBA 92 cm data observed between 1 January 2003 to December 31, 2006 have been analysed via an automatic pipeline, implemented within AIPS. The vast majority of the data are unpublished. Results. The sample consists of 44 sources, 34 of which have been detected on at least one VLBA baseline. 30 sources have sufficient data to be successfully imaged. Most of the sources are compact, with a few showing extended structures. -

Birds of Tarin Rock and North Tarin Rock Reserves
IV. BIRDS OF TARIN ROCK AND NORTH TARIN ROCK RESERVES J. DELL and R.E. JOHNSTONE INTRODUCTION Many aspects of the birds of the Western Australia wheatbelt are poorly known. There has been no attempt to document distributions before or after extensive clearing of about 80% of the region for agriculture. The small amount of information published since clearing has tended to include only local lists of species with no attempt to examine the avifauna of the wheatbelt or relate it to the vegetation, for example, McKenzie, Burbidge & Marchant (1973) and McKenzie and Youngson (1975). This paper is the first part of a series examining the avifauna of the wheatbelt (for outline of the wheatbelt vertebrate survey see Kitchener, Preface, this publication). This series will be presented as separate papers on bird assemblages of specific areas within the wheatbelt. They will then be synthesized to provide an evaluation of the avifauna of the wheatbelt. In this contribution we present observations on birds of the Tarin Rock area in the south-eastern wheatbelt and attempt to relate these to the plant associations described by Muir(this publication). We also compare the birds of this area with those outlined by Carnaby (1933) for Lake Grace, about 25 km east of Tarin Rock. Carnaby's list was compiled before most of the extensive agricultural clearing took place. It also included a considerable chllin ofsaltlakes and flats which provide habitat for waterfowl and waders not present at Tarin Rock. The rate of clearing in the wheatbelt and the resultant fragmentation of vegetation has not been documented. -

Tree-Ring Analysis of the Anglo-Scandinavian Oak Timbers by Cathy Tyers and Jennifer Hillam
The Archaeology of York Anglo-Scandinavian York 8/5 Anglo-Scandinavian Occupation at 16–22 Coppergate: Defining a Townscape Appendix 3: Tree-Ring Analysis of the Anglo-Scandinavian Oak Timbers by Cathy Tyers and Jennifer Hillam i List of Figures Fig.1 Bar diagram showing the relative positions of the dated ring sequences from Periods 2-5 and their associated felling dates. ................................................................................................................................ 4–6 Fig.2 Summary of the interpreted felling dates or date ranges ............................................................................................. 7 Fig. 3 Histogram showing the distribution of the sapwood values for the 13 measured samples with bark edge and the 2 sigma range of logarithmic values for the sapwood range ........................................... 15 Fig. 4 Histogram showing the distribution of the pseudo-sapwood values derived by assuming simultaneous felling of timbers with sapwood within structures with at least one timber with bark edge and the 2 sigma range of logarithmic values for the sapwood range .................................................... 15 Fig. 5a Diagram comparing the ring sequence length and average growth rates (average ring widths) of all of the dated timbers ............................................................................................................................................... 17 Fig.5b Diagram comparing the ring sequence length and average growth rates (average