Biopanic, Advanced Maternal Age and Fertility Outcomes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Induction Indication: Advanced Maternal Age
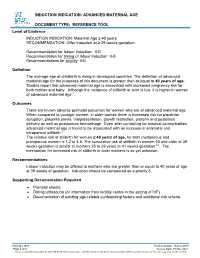
INDUCTION INDICATION: ADVANCED MATERNAL AGE DOCUMENT TYPE: REFERENCE TOOL Level of Evidence INDUCTION INDICATION: Maternal Age ≥ 40 years RECOMMENDATION: Offer Induction at ≥ 39 weeks gestation Recommendation for labour induction: II-B Recommendation for timing of labour induction: II-B Recommendations for priority: II-B Definition The average age of childbirth is rising in developed countries. The definition of advanced maternal age for the purposes of this document is greater than or equal to 40 years of age. Studies report that advanced maternal age is associated with increased pregnancy risk for both mother and baby. Although the incidence of stillbirth at term is low, it is higher in women of advanced maternal age.1 Outcomes There are known adverse perinatal outcomes for women who are of advanced maternal age. When compared to younger women, in older women there is increased risk for placental abruption, placenta previa, malpresentation, growth restriction, preterm and postdates delivery as well as postpartum hemorrhage. Even after controlling for medical co-morbidities, advanced maternal age is found to be associated with an increase in antenatal and intrapartum stillbirth.2 The relative risk of stillbirth for women ≥ 40 years of age, for both multiparous and primiparous women is 1.2 to 4.5. The cumulative risk of stillbirth in women 40 and older at 39 weeks gestation is similar to mothers 25 to 29 years at 41 weeks gestation3,4. The mechanism for increased risk of stillbirth in older mothers is as yet unknown. Recommendations Labour induction may be offered to mothers who are greater than or equal to 40 years of age at 39 weeks of gestation. -

Oocyte Or Embryo Donation to Women of Advanced Reproductive Age: an Ethics Committee Opinion
ASRM PAGES Oocyte or embryo donation to women of advanced reproductive age: an Ethics Committee opinion Ethics Committee of the American Society for Reproductive Medicine American Society for Reproductive Medicine, Birmingham, Alabama Advanced reproductive age (ARA) is a risk factor for female infertility, pregnancy loss, fetal anomalies, stillbirth, and obstetric com- plications. Oocyte donation reverses the age-related decline in implantation and birth rates of women in their 40s and 50s and restores pregnancy potential beyond menopause. However, obstetrical complications in older patients remain high, particularly related to oper- ative delivery and hypertensive and cardiovascular risks. Physicians should perform a thorough medical evaluation designed to assess the physical fitness of a patient for pregnancy before deciding to attempt transfer of embryos to any woman of advanced reproductive age (>45 years). Embryo transfer should be strongly discouraged or denied to women of ARA with underlying conditions that increase or exacerbate obstetrical risks. Because of concerns related to the high-risk nature of pregnancy, as well as longevity, treatment of women over the age of 55 should generally be discouraged. This statement replaces the earlier ASRM Ethics Committee document of the same name, last published in 2013 (Fertil Steril 2013;100:337–40). (Fertil SterilÒ 2016;106:e3–7. Ó2016 by American Society for Reproductive Medicine.) Key Words: Ethics, third-party reproduction, complications, pregnancy, parenting Discuss: You can discuss -

Pregnancy After Age 35
REFLECTING ON THE TREND: Pregnancy After Age 35 A guide to Advanced Maternal Age for Ontario service providers, including a summary of statistical trends, influencing factors, health benefits, health risks and recommendations for care. A collaborative project of: Best Start: Ontario’s Maternal, Newborn and Early Child Development Resource Centre and the Halton Region Health Department 2007 ACKNOWLEDGEMENTS This Best Start Resource Centre manual was developed in collaboration with the Halton Region Health Department. The Best Start Resource Centre would like to thank Halton Region’s Health Department for entering into this partnership, and Kathryn Bamford, Reproductive Health Manager, for her persistence in determining a strategy to make this happen. The Halton Region Health Department is located west of Toronto and is responsible for public health in the communities of Burlington, Halton Hills, Milton and Oakville. Halton region has one of the highest rates of pregnancy over the age of 35 in Ontario, and is very interested in strategies for care of this population. For more information on the Halton Region Health Department, call 905-825-6000 or visit www.halton.ca/health The Best Start Resource Centre would like to thank Michelle Schwarz, BScN, MPA, Public Health Nurse, at the Halton Region Health Department for her work in researching and drafting this publication. Best Start would also like to Key Informants and • Joyce Engel, PhD, • Hana Sroka, MSc, CCGC, acknowledge the important Expert Reviewers: Vice-President, Academic Genetic Counsellor, Mount Niagara College Sinai Hospital roles played by the following • Dr. Sean Blaine, BSc, MD Halton Region staff: CCFP, Lead Physician, STAR • Dr. -

Induction of Labour at Term in Older Mothers
Induction of Labour at Term in Older Mothers Scientific Impact Paper No. 34 February 2013 Induction of Labour at Term in Older Mothers 1. Background and introduction The average age of childbirth is rising markedly across Western countries.1 In the United Kingdom (UK) the proportion of maternities in women aged 35 years or over has increased from 8% (approximately 180 000 maternities) in 1985–87 to 20% (almost 460 000 maternities) in 2006–8 and in women aged 40 years and older has trebled in this time from 1.2% (almost 27 000 maternities) to 3.6% (approximately 82 000 maternities).2 There is a continuum of risk for both mother and baby with rising maternal age with numerous studies reporting multiple adverse fetal and maternal outcomes associated with advanced maternal age. Obstetric complications including placental abruption,3 placenta praevia, malpresentation, low birthweight,4–7 preterm8 and post–term delivery9 and postpartum haemorrhage,10 are higher in older mothers. As fertility declines with age, there is a greater use of assisted reproductive technologies (ARTs) and the possibility of multiple pregnancy increases. This may independently adversely affect the risks reported.11 Preexisting maternal medical conditions including hypertension, obesity and diabetes increase with advancing maternal age as do pregnancy–related maternal complications such as pre–eclampsia and gestational diabetes.12 These medical co–morbidities can all influence fetal health and are likely to compound the effect of age on the risk of pregnancy in an older -

Age and Fertility: a Guide for Patients
Age and Fertility A Guide for Patients PATIENT INFORMATION SERIES Published by the American Society for Reproductive Medicine under the direction of the Patient Education Committee and the Publications Committee. No portion herein may be reproduced in any form without written permission. This booklet is in no way intended to replace, dictate or fully define evaluation and treatment by a qualified physician. It is intended solely as an aid for patients seeking general information on issues in reproductive medicine. Copyright © 2012 by the American Society for Reproductive Medicine AMERICAN SOCIETY FOR REPRODUCTIVE MEDICINE Age and Fertility A Guide for Patients Revised 2012 A glossary of italicized words is located at the end of this booklet. INTRODUCTION Fertility changes with age. Both males and females become fertile in their teens following puberty. For girls, the beginning of their reproductive years is marked by the onset of ovulation and menstruation. It is commonly understood that after menopause women are no longer able to become pregnant. Generally, reproductive potential decreases as women get older, and fertility can be expected to end 5 to 10 years before menopause. In today’s society, age-related infertility is becoming more common because, for a variety of reasons, many women wait until their 30s to begin their families. Even though women today are healthier and taking better care of themselves than ever before, improved health in later life does not offset the natural age-related decline in fertility. It is important to understand that fertility declines as a woman ages due to the normal age- related decrease in the number of eggs that remain in her ovaries. -

Pregnancy Outcomes from More Than
Pregnancy outcomes from more than 1,800 in vitro fertilization cycles with the use of 24-chromosome single-nucleotide polymorphism–based preimplantation genetic testing for aneuploidy Alexander L. Simon, B.S.,a Michelle Kiehl, M.Sc.,a Erin Fischer, B.S.,b J. Glenn Proctor, M.H.A.,c Mark R. Bush, M.D.,c Carolyn Givens, M.D.,b Matthew Rabinowitz, Ph.D.,a and Zachary P. Demko, Ph.D.a a Natera, San Carlos, California; b Pacific Fertility Center, San Francisco, California; and c Conceptions Reproductive Associates of Colorado, Littleton, Colorado Objective: To measure in vitro fertilization (IVF) outcomes following 24-chromosome single‒nucleotide-polymorphism (SNP)–based preimplantation genetic testing for aneuploidy (PGT-A) and euploid embryo transfer. Design: Retrospective. Setting: Fertility clinics and laboratory. Patient(s): Women 20–46 years of age undergoing IVF treatment. Intervention(s): Twenty-four-chromosome SNP-based PGT-A of day 5/6 embryo biopsies. Main Outcome Measure(s): Maternal age–stratified implantation, clinical pregnancy, and live birth rates per embryo transfer; miscarriage rates; and number of embryo transfers per patient needed to achieve a live birth. Result(s): An implantation rate of 69.9%, clinical pregnancy rate per transfer of 70.6%, and live birth rate per transfer of 64.5% were observed in 1,621 nondonor frozen cycles with the use of SNP-based PGT-A. In addition, SNP-based PGT-A outcomes, when measured per cycle with transfer, remained relatively constant across all maternal ages; when measured per cycle initiated, they decreased as maternal age increased. Miscarriage rates were 5% in women %40 years old. -

Reaching Women Who Experience High Parity and Advanced Maternal Age Pregnancies
Using Family Planning to Address Drivers of Mortality: Reaching Women Who Experience High Parity and Advanced Maternal Age Pregnancies Maureen Norton, Ph.D. and Jane Ebot, Ph.D. United States Agency for International Development Global Maternal Newborn Health Conference Mexico City, Mexico Oct 18-21, 2015 FAMILY PLANNING SAVES LIVES • In one year, family planning prevented more than 272,000 maternal deaths, a 44% reduction • If all needs for family planning were met, an addition 104,00 maternal deaths could be prevented annually Source: Ahmed S, Quingfeng L, Tsui, A, (2012). Maternal deaths averted by contraceptive use: an analysis of 172 countries. The Lancet, 380(9837):111-125. 11/24/15 2 HEALTHY TIMES FOR A PREGNANCY OVER THE REPRODUCTIVE LIFE COURSE • For best maternal outcomes, healthiest times for a pregnancy are: • Age: After 18 and before 34 • Parity: Four or less than four children Photo credit is: © 2006 Marina Grayson, Courtesy of Photoshare Family planning can ensure that pregnancies occur at the healthiest times of a woman’s life. 11/24/15 3 Over 50% Stover J and Ross J. BMC Public Health, 2013(Suppl3):S4 High Parity: Percent birth order 4+ pregnancies - all women 15-49 years - USAID 24 priority countries 60 57 51 50 49 49 50 48 48 45 44 44 43 42 40 40 38 37 37 29 30 26 Percept 20 20 17 13 10 0 Source: DHS Surveys Note: No available data for Afghanistan, South Sudan, India. Advanced Maternal Age: Percent Advanced Maternal Age Pregnancies > age 34 – USAID 24 Priority Countries 20 18 17 18 17 17 16 16 16 15 15 15 15 15 14 14 -

Antioxidant Intervention Attenuates Aging-Related Changes in the Murine Ovary and Oocyte
life Article Antioxidant Intervention Attenuates Aging-Related Changes in the Murine Ovary and Oocyte Mandy G. Katz-Jaffe * , Sydney L. Lane , Jason C. Parks, Blair R. McCallie, Rachel Makloski and William B. Schoolcraft Colorado Center for Reproductive Medicine, Lone Tree, CO 80124, USA; [email protected] (S.L.L.); [email protected] (J.C.P.); [email protected] (B.R.M.); [email protected] (R.M.); [email protected] (W.B.S.) * Correspondence: MKatz-Jaff[email protected]; Tel.: +1-303-788-8300 Received: 15 September 2020; Accepted: 20 October 2020; Published: 22 October 2020 Abstract: Advanced maternal age (AMA) is associated with reduced fertility due in part to diminished ovarian follicle quantity, inferior oocyte quality, chromosome aneuploidy, and lower implantation rates. Ovarian aging is accompanied by increased oxidative stress and blunted antioxidant signaling, such that antioxidant intervention could improve reproductive potential. The first aim of this study was to determine the molecular effects of antioxidant intervention in the ovaries and oocytes of aged mice, utilizing a supplement containing only naturally occurring açaí (Euterpe oleracea) with an oxygen radical absorbance capacity of 208,628 µmol Trolox equivalent (TE)/100 g indicating high antioxidant activity. Nine month old female CF-1 mice were administered 80 mg/day antioxidants (n = 12) or standard diet (n = 12) for 12 weeks. In the ovary, antioxidant treatment upregulated β-adrenergic signaling, downregulated apoptosis and proinflammatory signaling, and variably affected cell growth and antioxidant pathways (p < 0.05). Exogenous antioxidants also increased the oocyte expression of antioxidant genes GPX1, SOD2, and GSR (p < 0.05). A feasibility analysis was then conducted on female AMA infertility patients as a proof-of-principle investigation. -

Patients of Advanced Maternal Age Should Only Transfer a Single
Clinical Obstetrics, Gynecology and Reproductive Medicine Research Article ISSN: 2059-4828 Patients of advanced maternal age should only transfer a single euploid blastocyst Catherine Gordon1, John B Whitney2, Ilene Hatch3, Nancy L Nugent2, Shane Zozula2, Robert E Anderson4 and Mitchel C Schiewe2* 1University of California-Irvine, Department of OB - GYN, Orange, CA 92868, USA 2Ovation Fertility/SCIRS, ART Lab, Newport Beach, CA 92663, USA 3Fertility Center of Southern California, Irvine, CA 92612, USA 4Southern California Center for Reproductive Medicine, Newport Beach, CA 92663, USA Abstract Background: The IVF industry has been trying to reduce high order multiple pregnancies by promoting single embryo transfer for nearly two decades. Although improvements in embryo culture practices concurrently occurred, poor prognosis patients and those of advanced maternal age (≥38 years old) proved to be challenging cases when determining the number of embryos to transfer and yet still optimize pregnancy success. It was not until preimplantation genetic screening (PGS) of blastocysts was coupled with conservative embryo transfer decisions that worldwide progress occurred. The objective of this study was to determine the efficacy of single embryo transfer (SET) compared to dual embryo transfer (DET) in older patients (age ≥38) performing vitrified-warmed, euploid ET cycles. Methods and findings: Retrospective cohort analysis was performed on 140 vitrified-warmed euploid blastocyst transfers of patients ≥38 years old performing either a SET (n=122) or DET (n=18). All full to hatched blastocysts were initially biopsied on Days 5, 6 or 7, and the trophectoderm samples were analyzed using NGS or aCGH. All transfers represented the patients first transfer attempt following PGS between January 2013 to June 2015. -

Examining Measurement Invariance for Parental Creativity Nurturing Behaviour (PCNB) Across Middle-East Nations and South-East As
Sys Rev Pharm 2021; 12(4): 242-246 Research Article A multifaceted review journal in the field of pharmacy E-ISSN 0976-2779 P-ISSN 0975-8453 Examining Measurement Invariance for Parental Creativity Nurturing Behaviour (PCNB) across Middle-East Nations and South-east Asian Nations Ekta Sharma1, Sandeep Sharma2, Muhammad Al-Kudah3, Angham Al-Tamimi4 Institut Agama Islam Negeri Palangka Raya, [email protected] Institut Agama Islam Negeri Palangka Raya, [email protected] Institut Agama Islam Negeri Tulungagung, [email protected] Article History: Submitted: 26.03.2021 Accepted: 16.04.2021 Published: 30.04.2021 ABSTRACT who pursued their carriers even after bearing a child. These advanced age women also reflected more Objective: In the recent years, the ratio of pregnancy developed background knowledge about pregnancy, has increased at advanced maternal age (AMA) in child care, labor and parental attitude. However, comparison to the previous times where giving birth was common around age 18. The purpose of this review medically speaking, these females faced more infertility issues, miscarriages and Caesarean sections in paper is to develop a comparative study of demographic and obstetric properties of primiparous females at young comparison to young primiparous females. and advanced maternal age. Conclusion: Pregnant ladies of advanced maternal age were different from young ladies in knowledge, Methods: A cross sectional study was carried out of the participants based upon the inclusion strategy. Two demographic, financial, and parental attitudes and groups with 150 participants in each was made; one characteristics. group had participants aged above 35 years and other Key words: In Vitro fertilization, Recurrent implantation group had participants with age between 20 to 29 years. -

Maternal Age-Specific Rates of Fetal Chromosomal Abnormalities in Korean Pregnant Women of Advanced Maternal
Original Article Obstet Gynecol Sci 2013;56(3):160-166 http://dx.doi.org/10.5468/ogs.2013.56.3.160 pISSN 2287-8572 · eISSN 2287-8580 Maternal age-specific rates of fetal chromosomal abnormalities in Korean pregnant women of advanced maternal age Young Joo Kim, Jee Eun Lee, Soo Hyun Kim, Sung Shin Shim, Dong Hyun Cha Department of Obstetrics and Gynecology, CHA Gangnam Medical Center, CHA University, Seoul, Korea Objective To evaluate the association of maternal age with occurrence of fetal chromosomal abnormalities in Korean pregnant women of advanced maternal age (AMA). Methods A retrospective review of the amniocentesis or chorionic villous sampling (CVS) database at Gangnam and Bundang CHA Medical Centers, between January 2001 and February 2012, was conducted. This study analyzed the incidence of fetal chromosomal abnormalities according to maternal age and the correlation between maternal age and fetal chromosomal abnormalities in Korean pregnant women ≥35 years of age. In addition, we compared the prevalence of fetal chromosomal abnormalities between women of AMA only and the others as the indication for amniocentesis or CVS. Results A total of 15,381 pregnant women were selected for this study. The incidence of aneuploidies increased exponentially with maternal age (P<0.0001). In particular, the risk of trisomy 21 (standard error [SE], 0.0378; odds ratio, 1.177; P<0.001) and trisomy 18 (SE, 0.0583; odds ratio, 1.182; P=0.0040) showed significant correlation with maternal age. Comparison between women of AMA only and the others as the indication for amniocentesis or CVS showed a significantly lower rate of fetal chromosomal abnormalities only in the AMA group, compared with the others (P<0.0001). -

Advanced Maternal Age and Assisted Reproductive Technologies in an Irish Population
Advanced maternal age and assisted reproductive technologies in an Irish population Item Type Article Authors O’Shea, L;Hughes, C;Mocanu, EV Publisher Irish Medical Journal Journal Irish Medical Journal Download date 28/09/2021 21:19:00 Link to Item http://hdl.handle.net/10147/578543 Find this and similar works at - http://www.lenus.ie/hse Original Paper 243 recipient twins after fetoscopic laser photocoagulation for twin-twin 23. Larroche JC, Girard N, Narcy F, Fallet C. Abnormal cortical plate transfusion syndrome. Fetal Diagn Ther. 2008;24:470-3. (polymicrogyria), heterotopias and brain damage in monozygous twins. 17. Lopriore E, van Wezel-Meijler G, Middeldorp JM, Sueters M, Biology of the neonate. 1994;65:343-52. Vandenbussche FP, Walther FJ. Incidence, origin, and character of 24. Spruijt M, Steggerda S, Rath M, van Zwet E, Oepkes D, Walther F, cerebral injury in twin-to-twin transfusion syndrome treated with Lopriore E. Cerebral injury in twin-twin transfusion syndrome treated fetoscopic laser surgery. Am J Obstet Gynecol. 2006;194:1215-20. with fetoscopic laser surgery. Obstet Gynecol. 2012;120:15-20. 18. Kline-Fath BM, Calvo-Garcia MA, O’Hara SM, Crombleholme TM, 25. Merhar SL, Kline-Fath BM, Meinzen-Derr J, Schibler KR, Leach JL. Racadio JM. Twin-twin transfusion syndrome: cerebral ischemia is not Fetal and postnatal brain MRI in premature infants with twin-twin the only fetal MR imaging finding. Pediatr Radiol. 2007;37:47-56. transfusion syndrome. J Perinatol. 2013;33:112-8. 19. Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE. Neonatal 26.