SRH and HIV LINKAGES COMPENDIUM Indicators & Related Assessment Tools 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NEW RELEASE GUIDE September 3 September 10 ORDERS DUE JULY 30 ORDERS DUE AUGUST 6
ada–music.com @ada_music NEW RELEASE GUIDE September 3 September 10 ORDERS DUE JULY 30 ORDERS DUE AUGUST 6 2021 ISSUE 19 September 3 ORDERS DUE JULY 30 SENJUTSU LIMITED EDITION SUPER DELUXE BOX SET Release Date: September 3, 2021 INCLUDES n Standard 2CD Digipak with 28-page booklet n Blu-Ray Digipak • “The Writing On The Wall” • Making Of “The Writing On The Wall” • Special Notes from Bruce Dickinson • 20-page booklet n 3 Illustrated Art Cards n 3D Senjutsu Eddie Lenticular n Origami Sheet with accompanying instructions to produce an Origami version of Eddie’s Helmet, all presented in an artworked envelope n Movie-style Poster of “The Writing On The Wall” n All housed in Custom Box made of durable board coated with a gloss lamination TRACKLIST CD 1 1. Senjutsu (8:20) 2. Stratego (4:59) 3. The Writing On The Wall (6:23) 4. Lost In A Lost World (9:31) 5. Days Of Future Past (4:03) 6. The Time Machine (7:09) CD 2 7. Darkest Hour (7:20) 8. Death of The Celts (10:20) 9. The Parchment (12:39) 10. Hell On Earth (11:19) BLU-RAY • “The Writing On The Wall” Video • “The Writing On The Wall” The Making Of • Special notes from Bruce Dickinson LIMITED EDITION SUPER DELUXE BOX SET List Price: $125.98 | Release Date: 9/3/21 | Discount: 3% Discount (through 9/3/21) Packaging: Super Deluxe Box | UPC: 4050538698114 Returnable: YES | Box Lot: TBD | Units Per Set: TBD | File Under: Rock SENJUTSU Release Date: September 3, 2021 H IRON MAIDEN Take Inspiration From The East For Their 17th Studio Album, SENJUTSU H Brand new double album shows band maintain -

Still Lost Inside the Velvet Trail: March New Album Reviews Pt. 2
Still Lost Inside The Velvet Trail: March New Album Reviews Pt. 2. Music | Bittles‘ Magazine Have you heard the new Madonna record yet? Terrible! The entire time I was listening to it the only thing I could think was »That poor woman!«. Whoever advised her that songs like Bitch I’m Madonna were a good idea deserves to be locked in a room with Mark Ronson for an entire day. Luckily there is some fantastic new music out there which more than makes up for the inane racket created by the Peter Pan of pop. By JOHN BITTLES For example we have Vessels, Fort Romeau, Phildel, Mu-Ziq, SCNTST, Mike Simonetti and more bringing out albums which ably counteract all the shit you find in the charts. You might also notice that this week begins a brand new trend where I give each album a rating out of ten. The powers that be were against it, and have made numerous attempts on my life, but until I get bored of it, this new regime is here to stay. So, put on your cowboy hat, ensure your whiskers are well groomed, that the cat is fed, and let us begin… This week we’ll start with an album which has been rocking my stereo ever since it came into my life. Dilate by former math rockers Vessels sees the Leeds-based four piece move away from the post rock of their previous output and into the world of groove-some techno and late night electronica. This is so good one listen can give you an erection for a week (not clinically proven). -

– Agenge D'épopées Musicales –
– AGENGE D’ÉPOPÉES MUSICALES – L’AGENCE SUPER! est une agence artistique créée en 2006 par Julien Catala, à la fois défricheuse de talent, producteur de concerts et festivals, tourneur, programmateur d’événements, agitateur… Représentant aujourd’hui plus de 300 artistes internationaux entre têtes d’affiches confirmées (The XX, Nicolas Jaar, Bon Iver, Cigarettes After Sex, Polo & Pan…) et jeunes loups de l’avant garde musicale internationale (Alex Cameron, Shame, Bicep, Tom Misch … ), SUPER! est devenu en quelques années un véritable “label”, symbole de la musique live indépendante mondiale. PLUS DE SUPER! est aussi producteur du Pitchfork Music Festival Paris 16 000 LIKES qui se déroule depuis 2011 à la Grande Halle de la Villette, coproducteur du Festival Cabourg Mon Amour en juin sur la côte normande et coproducteur de Biarritz En Eté! dont la première édition aura lieu en juillet 2018. PLUS DE 11 000 FOLLOWERS Au fil des années, SUPER! a également développé une activité de production évènementielle en travaillant avec des marques et médias comme Red Bull, Converse, Chanel, Society et de direction artistique avec le festival Villette Sonique, les Inrocks ou encore la Fondation Louis Vuitton. Enfin, SUPER! PLUS DE dirige la salle de concert Le Trabendo, lieu parisien des 3 000 FOLLOWERS musiques actuelles et émergentes, situé dans le Parc de la Villette. Défricheur des nouvelles tendances musicales : rock, folk, pop et électronique, SUPER! incarne un projet WWW.SUPERMONAMOUR.COM artistique fort, radar de l’innovation musicale internationale. -

2.+ENG Dossierprensa2018.Pdf
1 THE FESTIVAL 3 LINEUP 5 PLACES 11 ORGANIZATION AND PARTNERS 12 TICKETS 14 GRAPHIC CAMPAIGN 15 PRESS QUOTES 16 CONTACT 17 2 THE FESTIVAL Primavera Sound has always concentrated all its efforts on uniting the latest musical proposals from the independent scene together with already well established artists, while embracing any style or genre in the line up, fundamentally looking for quality and essentially backing pop and rock as well as underground electronic and dance music. Over the last years, the festival has had the most diverse range of artists. Some of those who have been on stage are Radiohead, Pixies, Arcade Fire, PJ Harvey, The National, Nine Inch Nails, Kendrick Lamar, Neil Young, Sonic Youth, Portishead, Pet Shop Boys, Pavement, Echo & The Bunnymen, Lou Reed, My Bloody Valentine, Brian Wilson, Pulp, Patti Smith, Nick Cave, Cat Power, Public Enemy, Franz Ferdinand, Television, Devo, Enrique Morente, The White Stripes, LCD Soundsystem, Tindersticks, Queens of the Stone Age, She- llac, Dinosaur Jr., New Order, Fuck Buttons, Swans, The Cure, Bon Iver, The xx, Iggy & The Stooges, De La Soul, Marianne Faithfull, Blur, Wu-Tang Clan, Phoenix, The Jesus and Mary Chain, Tame Impala, The Strokes, Belle & Sebastian, Antony & the Johnsons, The Black Keys, James Blake, Interpol and Sleater-Kinney amongst many others. Primavera Sound has consolidated itself as the urban festival par excellence with unique characteristics that have projected it internationally as a reference cultural event. The event stands out from other large music events and is faithful to its original artistic idea, keeping the same standards and maintaining the same qua- lity of organization of past years, without resorting to more commercial bands. -

2017 MAJOR EURO Music Festival CALENDAR Sziget Festival / MTI Via AP Balazs Mohai
2017 MAJOR EURO Music Festival CALENDAR Sziget Festival / MTI via AP Balazs Mohai Sziget Festival March 26-April 2 Horizon Festival Arinsal, Andorra Web www.horizonfestival.net Artists Floating Points, Motor City Drum Ensemble, Ben UFO, Oneman, Kink, Mala, AJ Tracey, Midland, Craig Charles, Romare, Mumdance, Yussef Kamaal, OM Unit, Riot Jazz, Icicle, Jasper James, Josey Rebelle, Dan Shake, Avalon Emerson, Rockwell, Channel One, Hybrid Minds, Jam Baxter, Technimatic, Cooly G, Courtesy, Eva Lazarus, Marc Pinol, DJ Fra, Guim Lebowski, Scott Garcia, OR:LA, EL-B, Moony, Wayward, Nick Nikolov, Jamie Rodigan, Bahia Haze, Emerald, Sammy B-Side, Etch, Visionobi, Kristy Harper, Joe Raygun, Itoa, Paul Roca, Sekev, Egres, Ghostchant, Boyson, Hampton, Jess Farley, G-Ha, Pixel82, Night Swimmers, Forbes, Charline, Scar Duggy, Mold Me With Joy, Eric Small, Christer Anderson, Carina Helen, Exswitch, Seamus, Bulu, Ikarus, Rodri Pan, Frnch, DB, Bigman Japan, Crawford, Dephex, 1Thirty, Denzel, Sticky Bandit, Kinno, Tenbagg, My Mate From College, Mr Miyagi, SLB Solden, Austria June 9-July 10 DJ Snare, Ambiont, DLR, Doc Scott, Bailey, Doree, Shifty, Dorian, Skore, March 27-April 2 Web www.electric-mountain-festival.com Jazz Fest Vienna Dossa & Locuzzed, Eksman, Emperor, Artists Nervo, Quintino, Michael Feiner, Full Metal Mountain EMX, Elize, Ernestor, Wastenoize, Etherwood, Askery, Rudy & Shany, AfroJack, Bassjackers, Vienna, Austria Hemagor, Austria F4TR4XX, Rapture,Fava, Fred V & Grafix, Ostblockschlampen, Rafitez Web www.jazzfest.wien Frederic Robinson, -
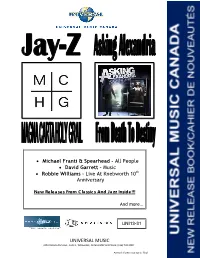
UNIVERSAL MUSIC • Michael Franti & Spearhead – All People • David
Michael Franti & Spearhead – All People David Garrett – Music Robbie Williams – Live At Knebworth 10th Anniversary New Releases From Classics And Jazz Inside!!! And more… UNI13-31 “Our assets on-line” UNIVERSAL MUSIC 2450 Victoria Park Ave., Suite 1, Willowdale, Ontario M2J 5H3 Phone: (416) 718.4000 Artwork shown may not be final UNIVERSAL MUSIC CANADA NEW RELEASE Artist/Title: JAY‐Z / MAGNA CARTA HOLY GRAIL (Standard Version) Bar Code: Cat. #: DEFW4027102 Price Code: SP Order Due: ASAP Release Date: July 9, 2013 8 57018 00418 2 File: Rap / Hip Hop Genre Code: 34 Box Lot: 25 Key Tracks: *SHORT SELL CYCLE “Holy Grail” ft. Justin Timberlake *NOT ACTUAL COVER Artist/Title: JAY‐Z / MAGNA CARTA HOLY GRAIL (Deluxe Version) Bar Code: Cat. #: B001887702 Price Code: SPS Order Due: July 4, 2013 Release Date: July 23, 2013 8 57018 00414 4 File: Rap / Hip Hop Genre Code: 34 Box Lot: 25 Key Tracks: *SHORT SELL CYCLE “Holy Grail” ft. Justin Timberlake *NOT ACTUAL COVER KEY POINTS: • Over 50 Million Albums sold worldwide – 1 million in Canada! • 10 Grammy Awards including 3 for his 2009 release “Blueprint 3” which debuted #1 in Canada • Previous album Watch The Throne with Kanye West has scanned over 130,000 units • Magna Carta Holy Grail includes 15 brand new songs! • Deluxe Version includes intricate 6‐panel soft pack, 28‐page booklet with black o‐card. The idea behind the package is that it needs to be destroyed in order for the information inside to be revealed. • Massive advertising & promotional campaigns running from release throughout the -

March 10, 2021 Jordan Rakei Announces Late Night Tales Compilation, out April
March 10, 2021 For Immediate Release Jordan Rakei Announces Late Night Tales Compilation, Out April 9th Listen to Rakei’s Exclusive Cover of Jeff Buckley’s “Lover, You Should've Come Over” (Photo Credit: Dan Medhurst) The artist-curated mix series, Late Night Tales, is pleased to announce its next compilation, this time curated by multi-instrumentalist, vocalist and producer Jordan Rakei, out April 9th. For Rakei’s Late Night Tales, the first mix of the acclaimed series’ 20th year, the 28-year-old modern soul icon effortlessly stamps his own jazz and hip-hop driven sound all over this gorgeous array of handpicked tracks. A beautifully layered blend that is mirrored in the music he’s made, it comes as no surprise that such a supremely gifted songwriter should deliver a mix that is all about the song. “I wanted to try and showcase as many people as I knew on this mix,” says Rakei. “My idea of Late Night Tales was to distil a series of relaxing moments; the whole conceptual sonic of relaxation. So, I was trying to think of all the collaborators and friends that I knew, who’d recorded stuff with this horizontal vibe. Plus, I was also trying to help my friends' stuff get into the world. I know the story of Khruangbin blowing up after appearing on the series (in fact, I think that's how I discovered them). So, the main idea was to create a certain atmosphere, but also to help some of my favourite collaborators and buddies to give their songs a little push out into the world. -

Audio/Video - Software - Hifi - High-End - Surround – Home Theatre
AUDIO/VIDEO - SOFTWARE - HIFI - HIGH-END - SURROUND – HOME THEATRE MAY 2013 NL € 5,45 BE € 5,95 TEST BP ACCUPHASE DP-550 The high- ACCUPHASE DP-550 SACD-PLAYER tested end Disc player with extended DAC functionality The first thing that I experience when The Japanese noble brand Accuphase was founded in June 1972 by the former Trio- unpacking the substantial and weighty Kenwood box (25 kg) of the DP-550 sa (CD) player, co-founder Jiro Kasuga and his older brother Nakaichi. In the same year the Kasuga left is the extremely serious impact in which brothers namely Trio-Kenwood, with the idea of hifi components of the highest caliber to go this Japanese company always manufacture. Unlike abroad where brands like McIntosh, Audio manufactures its products. Of course, Research, Mark Levinson and Revox set the tone. Was the Japanese offer in those years there are still more manufacturers that actually mainly low to medium-priced products at best mediocre quality. offer beautifully finished and carefully The ambitious plan was an extra push in the right direction by the oil crisis in 1973. constructed products now. As far as I am Investing in sustainability and high quality products that easily could go long, with concerned, very few go as far as became the new motto. An ideology that even today continues unabated Accuphase does. Not only has every detail Accuphase in all its products will continue and where the tested here DP-550 Super Audio been thought of thoroughly, but also the CD player is a wonderful example of materials used and the techniques are particularly solid and durable. -

Davide-Rossi-Discography.Pdf
Davide Rossi 2016 Superbowl Performance Flight Facilities Live Show Coldplay N/A String Arranger/Performer Debut / Album Flight Facilities x MSO N/A String Arranger/Performer Mylo Xyloto / Lucy O’Bryne Island String Arranger/Performer Coldplay Parlophone Every Teardrop Is A Waterfall Coldplay Parlophone String Arranger/Performer Prospekt’s March Coldplay Parlophone String Arranger/Performer Viva La Vida Coldplay Parlophone String Arranger/Performer Girl On Fire Alicia Keys RCA/Jive String Arranger/Performer The Element of Freedom Alicia Keys RCA/Jive String Arranger/Performer Something Great One Direction Sony String Arranger/Performer Score for the film ‘Monsters’ Jon Hopkins Domino String Arranger/Performer Insides Jon Hopkins Domino String Arranger/Performer If You Wait London Grammar Ministry Of String Arranger/Performer Sound Junior Röyksopp EMI String Arranger/Performer Senior Röyksopp EMI String Arranger/Performer Suite For A Robotic Girl Röyksopp EMI String Arranger/Performer New Shores Black Submarine Kobalt Writer/Producer/String Arranger The Singles Goldfrapp EMI/Mute String Arranger/Performer Head First Goldfrapp EMI/Mute String Arranger/Performer 2010 Believer Goldfrapp EMI/Mute String Arranger/Performer Seventh Tree Goldfrapp EMI/Mute String Arranger/Performer Wonderful Electric: Live in London Goldfrapp EMI/Mute String Arranger/Performer Black Cherry Goldfrapp EMI/Mute String Arranger/Performer Felt Mountain Goldfrapp EMI/Mute String Arranger/Performer Pale Horses Moby Little Idiot String Arranger/Performer Records Mistake -

Best of 2014 Listener Poll Nominees
Nominees For 2014’s Best Albums From NPR Music’s All Songs Considered Artist Album ¡Aparato! ¡Aparato! The 2 Bears The Night is Young 50 Cent Animal Ambition A Sunny Day in Glasgow Sea When Absent A Winged Victory For The Sullen ATOMOS Ab-Soul These Days... Abdulla Rashim Unanimity Actress Ghettoville Adia Victoria Stuck in the South Adult Jazz Gist Is Afghan Whigs Do To The Beast Afternoons Say Yes Against Me! Transgender Dysphoria Blues Agalloch The Serpent & The Sphere Ages and Ages Divisionary Ai Aso Lone Alcest Shelter Alejandra Ribera La Boca Alice Boman EP II Allah-Las Worship The Sun Alt-J This is All Yours Alvvays Alvvays Amason Duvan EP Amen Dunes Love Ana Tijoux Vengo Andrew Bird Things Are Really Great Here, Sort Of... Andrew Jackson Jihad Christmas Island Andy Stott Faith In Strangers Angaleena Presley American Middle Class Angel Olsen Burn Your Fire For No Witness Animal Magic Tricks Sex Acts Annie Lennox Nostalgia Anonymous 4 David Lang: love fail Anthony D'Amato The Shipwreck From The Shore Antlers, The Familiars The Apache Relay The Apache Relay Aphex Twin Syro Arca Xen Archie Bronson Outfit Wild Crush Architecture In Helsinki NOW + 4EVA Ariel Pink Pom Pom Arturo O’Farrill & the Afro Latin Orchestra The Offense of the Drum Ásgeir In The Silence Ashanti BraveHeart August Alsina Testimony Augustin Hadelich Sibelius, Adès: Violin Concertos The Autumn Defense Fifth Avey Tare Enter The Slasher House Azealia Banks Broke With Expensive Taste Band Of Skulls Himalayan Banks Goddess Barbra Streisand Partners Basement Jaxx Junto Battle Trance Palace Of Wind Beach Slang Cheap Thrills on a Dead End Street Bebel Gilberto Tudo Beck Morning Phase Béla Fleck & Abigail Washburn Béla Fleck & Abigail Washburn Bellows Blue Breath Ben Frost A U R O R A Benjamin Booker Benjamin Booker Big K.R.I.T. -

The Sync Project Teams with World-Renowned Artists, Peter Gabriel, St
The Sync Project Teams with World-Renowned Artists, Peter Gabriel, St. Vincent, Jon Hopkins and Esa-Pekka Salonen, to Advance Music as Medicine Company also appoints biotech industry veteran Steven Holtzman to Board of Directors Boston, Massachusetts, May 4, 2016 – The Sync Project, a clinical-stage company focused on developing music as personalized medicine, today announced the appointments of four world-renowned musical artists to its Advisory Board. The new advisors – Rock and Roll Hall of Famer Peter Gabriel; Grammy Award- winning alternative artist, Annie Clark (St. Vincent); critically acclaimed electronic musician, Mercury Music Prize and Ivor Novello nominee, Jon Hopkins; distinguished composer and conductor, Esa-Pekka Salonen – will collaborate with the Sync Project on product strategy. The Company also announced the appointment of former Biogen Idec Executive Vice President and Millennium Pharmaceuticals Chief Business Officer, Steven Holtzman, to its Board of Directors. “Peter, Annie, Jon and Esa-Pekka are all using technology in creative ways to push the boundaries of what music can be,” said Marko Ahtisaari, the Sync Project’s Co-Founder and CEO. “These extraordinary artists, together with Steve and our other board members and advisors, will help to advance our clinical strategy to develop music as precision medicine.” “Our senses provide us with different ways of inputting and experiencing ideas and emotions and also provide wonderful opportunities to change our physical and mental health,” said Peter Gabriel. “A good collection of music has always been used as a box of mood pills. I am delighted that The Sync Project is now using evidence-based science to explore and develop real tools and a platform to engage sound and music in the practice of medicine.” Recent research has shown that music can modulate neural systems like the dopamine response, autonomic nervous system and others related to stress, movement, learning and memory. -

COLDPLAY LIVE 2012 COMES to CINEMAS AROUND the WORLD for ONE NIGHT ONLY on NOVEMBER 13Th
2012-10-29 12:20 CET COLDPLAY LIVE 2012 COMES TO CINEMAS AROUND THE WORLD FOR ONE NIGHT ONLY ON NOVEMBER 13th Filmen vises Århus, Ålborg, Odense, Næstved og København! Køb billetter til filmen London 29 October 2012 – Coldplay Live 2012 - the band’s first concert film/live album for nine years, is to get a special one-night-only release in cinemas around the world. More than 50 countries will screen the full feature length film on the night of November 13th. Confirmed listings and links to book tickets can be found at http://www.coldplay.com/cinema The JA Digital production for EMI/Parlophone, is directed by Paul Dugdale, previously responsible for Adele’s Live at the Royal Albert Hall and The Prodigy’s World’s On Fire concert films. The film documents Coldplay’s acclaimed Mylo Xyloto world tour, which has been seen by more than three million people since it began in June 2011. Live 2012 includes footage from Coldplay’s shows at Paris’s Stade de France, Montreal’s Bell Centre and last year’s triumphant Pyramid Stage headline performance at Glastonbury Festival. The trailer for the film can be seen at: http://www.youtube.com/watch?v=EB-NbV4JTjU Coldplay’s Chris Martin said of the film: “The Mylo Xyloto tour has been the most fun we’ve ever had as a band. It’s felt very uplifting right from the start; partly because we are proud of the music, the LED wristbands, the pyrotechnics, the lasers and all of that stuff, but mainly because of the amazing audiences that we’ve been playing for.