Environmental Burden of Disease Associated with Inadequate Housing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HISTORY of LEAD POISONING in the WORLD Dr. Herbert L. Needleman Introduction the Center for Disease Control Classified the Cause
HISTORY OF LEAD POISONING IN THE WORLD Dr. Herbert L. Needleman Introduction The Center for Disease Control classified the causes of disease and death as follows: 50 % due to unhealthy life styles 25 % due to environment 25% due to innate biology and 25% due to inadequate health care. Lead poisoning is an environmental disease, but it is also a disease of life style. Lead is one of the best-studied toxic substances, and as a result we know more about the adverse health effects of lead than virtually any other chemical. The health problems caused by lead have been well documented over a wide range of exposures on every continent. The advancements in technology have made it possible to research lead exposure down to very low levels approaching the limits of detection. We clearly know how it gets into the body and the harm it causes once it is ingested, and most importantly, how to prevent it! Using advanced technology, we can trace the evolution of lead into our environment and discover the health damage resulting from its exposure. Early History Lead is a normal constituent of the earth’s crust, with trace amounts found naturally in soil, plants, and water. If left undisturbed, lead is practically immobile. However, once mined and transformed into man-made products, which are dispersed throughout the environment, lead becomes highly toxic. Solely as a result of man’s actions, lead has become the most widely scattered toxic metal in the world. Unfortunately for people, lead has a long environmental persistence and never looses its toxic potential, if ingested. -

Slave Housing Data Base
Slave Housing Data Base Building Name: Howard’s Neck, Quarter B Evidence Type: Extant Historical Site Name: Howard's Neck City or Vicinity: Pemberton (near Cartersville, and Goochland C.H.) County: Goochland State: Virginia Investigators: Douglas W. Sanford; Dennis J. Pogue Institutions: Center for Historic Preservation, UMW; Mount Vernon Ladies' Association Project Start: 8/7/08 Project End: 8/7/08 Summary Description: Howards’ Neck Quarter B is a one-story, log duplex with a central chimney and side-gable roof, supported by brick piers, and is the second (or middle) of three surviving currently unoccupied quarters arranged in an east-west line positioned on a moderately western sloping ridge. The quarters are located several hundred yards southwest of the main house complex. The core of the structure consists of a hewn log crib, joined at the corners with v-notches, with a framed roof (replaced), and a modern porch on the front and shed addition to the rear. Wooden siding currently covers the exterior walls, but the log rear wall enclosed by the shed is exposed; it is whitewashed. The original log core measures 31 ft. 9 in. (E-W) x 16 ft. 4 in. (N-S); the 20th-century rear addition is 11 ft. 8 in. wide (N-S) x 31 ft. 9 in. long (E-W). A doorway allows direct access between the two main rooms, which may be an original feature; a doorway connecting the log core with the rear shed has been cut by enlarging an original window opening in Room 1. As originally constructed, the structure consisted of two first-floor rooms, with exterior doorways in the south facade and single windows opposite the doorways in the rear wall. -
Environmental Health Playbook: Investing in a Robust Environmental Health System Executive Summary
Environmental Health Playbook: Investing in a Robust Environmental Health System Executive Summary Background and Need for Action Environmental Health is the branch of public health that focuses on the interrelationships between people and their environment, promotes human health and well-being, and fosters healthy and safe communities. As a fundamental component of a comprehensive public health system, environmental health works to advance policies and programs to reduce chemical and other environmental exposures in air, water, soil, and food to protect residents and provide communities with healthier environments. Environmental health protects the public by tracking environmental exposures in communities across the United States and potential links with disease outcomes. To achieve a healthy community, homes should be safe, affordable, and healthy places for families to gather. Workplaces, schools, and child care centers should be free of exposures that negatively impact the health of workers or children. Nutritious, affordable foods should be safe for all community members. Access to safe and affordable multimodal transportation options, including biking and public transit, improves the environment and drives down obesity and other chronic illnesses. Outdoor and indoor air quality in all communities should be healthy and safe to breathe for everyone. Children and adults alike should have access to safe and clean public spaces, such as parks. When a disaster strikes, a community needs to be prepared; it should have the tools and resources to be resilient against physical (infrastructure and human) and emotional damage. All these activities require the participation of federal, state, local, and tribal governments. Building a Robust Environmental Health System Investing in essential governmental environmental health services through dedicated resources will create an effective environmental health system that proactively protects communities and helps everyone attain good health. -

Advancing Healthy Housing: a Strategy for Action Abbreviations
healthyhomes.hud.gov Advancing Healthy Housing A STRATEGY FOR ACTION 2013 A Report from the Federal Healthy Homes Work Group Table of Contents Abbreviations __________________________________________________________________3 Executive Summary ________________________________________________________________4 Introduction __________________________________________________________________8 Advancing Healthy Housing Goals ___________________________________________________16 Goal 1 Establish Healthy Homes Recommendations _________________________________17 1.1 Establish Recommendations for Assessing Health and Safety Hazards ______17 Goal 2 Encourage Adoption of Healthy Homes Recommendations _____________________19 2.1 Obtain Commitments from Agencies to Advance Healthy Housing ________19 2.2 Strengthen Federal Efforts to Reduce Public Health Risks in Housing _______20 2.3 Explore Ways to Leverage Funding across Federal and Non-Federal Programs _______________________________________________21 Goal 3 Create and Support Training and Workforce Development to Address Health Hazards in Housing ______________________________________________________22 3.1 Support Enhanced Healthy Homes Training and Workforce Development __22 3.2 Accelerate Replication of Successful Local Healthy Housing Programs ______23 3.3 Encourage Pilots or Demonstration Programs that Advance Healthy Housing ____________________________________________23 Goal 4 Educate the Public about Healthy Homes ____________________________________24 4.1 Develop a Communications Strategy -

U.S. EPA, Pesticide Product Label, ARCH OIT 45, 01/15/2009
c (' UNITED STATES ENVIRONMENTAL PROTECTION AGENCY ro WASHINGTON, D.C. · 20460 JAN 1 5 2009 &EPA'~;;:IPttiectioo Office of Pesticide Programs Arch Chemical, Inc. 1955 Lake Park Drive, Suite 100 Smyrna, GA 30080 . Attention: Garret B. Schifilliti Senior Regulatory Manager Subject: Arch OIT 45 EPA Registration No. 1258-1323 Your Amendment Dated December 16,2008 This will acknowledge receipt of your notification of changes to the Storage and Disposal Statements for the "Container Rule", submitted under the provisions of FIFRA Section 3(c)(9). Based on a review of the submitted material, the following comments apply. The Notification dated December 18, 2008 is in compliance with PR Notice 98-10 and is acceptable. This Notification has been added to your file. If you have any questions concerning this letter, please contact Martha Terry at (703) 308-6217. Sincerely ~h1'b Marshall Swindell ~ Product Manager (33) Regulatory Management Branch 1 Antimcrobials Division (7510C) ( ( Forrt., _oroved. O. _No. 2070-0060 . emir.. 2·28·95 United States Registration OPP Identifier Number &EPA Environmental Protection Agency Amendment Washington, DC 20460 @.;. Other· Application for Pesticide - Section I 1. Company/Product Number 2. EPA Product Manager 3. Proposed Classification 1258-1323 Marshall Swindell [2] None D Restricted 4. Company/Product (Name) PM' Arch OIT 45 5. Nama and Address of Applicant (Include ZIP Code) 6. Expedited Reveiw. In accordance with FIFAA Section 3(c)(3) Arch Chemicals, Inc. (b)(il. my product is similar or identical in composition and labeling to: 1955 Lake Park Drive EPA Reg. No. ________________________________ Smyrna, GA 30080 D Check if this is a neW address Product Name Section - II Amendment - Explain below. -

California Licensed Contractor ©
WINTER/SPRING 2011 California © Licensed Contractor Stephen P. Sands, Registrar | Edmund G. Brown Jr., Governor 2011 Contracting Laws That Affect You CSLB Has an Licenses for Limited Liability Companies (LLCs) Coming App for That The passage of Senate Bill 392 (and various provisions of the Contractors State License Law CSLB recently including B&P Code Sections 7071.65 and 7071.19) authorizes CSLB to issue contractor launched its new licenses to limited liability companies (LLCs). The law says that CSLB shall begin processing “CSLB mobile” LLC applications no later than January 1, 2012. The LLC will be required to maintain website: www.cslb. liability insurance of between $1,000,000 and $5,000,000, and post a $100,000 surety ca.gov/mobile. bond in addition to the $12,500 bond already required of all licensees. (Senate Bill 392 is CSLB mobile now available at: www.leginfo.ca.gov/pub/09-10/bill/sen/sb_0351-0400/sb_392_bill_20100930_ enables users to chaptered.pdf.) check a license, get CSLB office locations, However, do not apply for an LLC license yet; CSLB is not issuing licenses to LLCs at this time. sign up for e-mail alerts, and help report unlicensed activity right from their “smart” CSLB staff is developing new application procedures, creating applications, and putting in phone. place important technology programming changes that are necessary for this new feature. CSLB anticipates that it will be able to accept and process LLC applications late in 2011. “This is an exciting new step for CSLB,” said Registrar Steve Sands. “This application The best way to receive future updates is to sign up for CSLB E-Mail Alerts at www.cslb.ca.gov. -
ACCESSIBLE:^^ Byes, Unrestricted
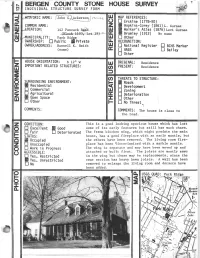
ACCESSIBLE:^^ BYes, Unrestricted CONSTRUCTION DATE/SOURCE: NUMBER OF STORIES: 1-1/2 c. 1770-1810/Architectural evidence CELLAR: B Yes —43 No DC BUILDER: An Ackerson, probably John. CHIMNEY FOUNDATION: O D Stone Arch V) FORM/PLAN TYPE: • Brick Arch, Stone Foundation 111 "F", 5 bay, center hall, 2 rooms deep D Other (32 f 6" x 43'8"). Frame addition Q added as kitchen. FLOOR JOISTS: 6-7" x 9" deep, 23-24" between, 1235-13" floorboards. FRAMING SYSTEM: FIRST FLOOR CEILING HEIGHT: 8'4" ~ In ermed late Bearing Wall FIRST FLOOR WALL THICKNESS: Clear Span 24" L Other GARRET FLOOR JOISTS: Not visible. EXTERIOR MALL FABRIC: GARRET: Well cut red sandstone all around, Unfinished Space except some rubble on west end. B Finished Space ROOF: FENESTRATION: Gable (wing) Not original. 32" x 58" in front, • Gambrel trapezoidal lintels. D Curb D Other ENTRANCE LOCATION/TYPE: EAVE TREATMENT: Plain entrance door in center 37" x 7*5", Sweeping Overhang not original. Supported Overhang (in front) No Overhang D Boxed Gutter D Other This house Is significant for its architecture and its association with the exploration and settlement of the Bergen County, New Jersey area. It is a reasonably well preserved example of the Form/Plan Type as shown and more fully described herein. As such, it is included in the Thematic Nomination to the National Register of Historic Places for the Early Stone Houses of Bergen County, New Jersey. FLOOR PLANS Howard I. Durie believes this house to have been built about 1775 for John G. Eckerson, son of Garret Eckerson, on land Garret and his 0s! cousin Garret Haring purchased on May 4, 1759 from Rev. -

Environmental Threats to Children's Health in Southeast Asia and The
Children’s Health Review Environmental Threats to Children’s Health in Southeast Asia and the Western Pacific William A. Suk,1 Kuhnying Mathuros Ruchirawat,2 Kalpana Balakrishnan,3 Martha Berger,4 David Carpenter,5 Terri Damstra,6 Jenny Pronczuk de Garbino,7 David Koh,8 Philip J. Landrigan,9 Irma Makalinao,10 Peter D. Sly,11 Y. Xu,12 and B.S. Zheng13 1Center for Risk and Integrated Sciences, National Institute of Environmental Health Sciences, Research Triangle Park, North Carolina, USA; 2Chulabhorn Research Institute, Bangkok, Thailand; 3Sri Ramachandra Medical College and Research Institute, Porur, Chennai, India; 4Office of Children’s Health Protection, U.S. Environmental Protection Agency, Washington, DC, USA; 5School of Public Health, University at Albany, Rensselaer, New York, USA; 6World Health Organization, International Programme on Chemical Safety, Research Triangle Park, North Carolina, USA; 7World Health Organization, International Programme on Chemical Safety, Geneva, Switzerland; 8National University of Singapore, Department of Community, Occupational and Family Medicine, Singapore; 9Center for Children’s Health and the Environment, Department of Community and Preventive Medicine, Mount Sinai School of Medicine, New York, New York, USA; 10Department of Pharmacology and Toxicology, University of the Philippines College of Medicine, Manila, Philippines; 11Princess Margaret Hospital for Children, Child Health Research, Subiaco, Washington, USA; 12Institute of Hydrobiology, Chinese Academy of Sciences, Wuhan, People’s Republic of China; 13Institute of Geochemistry, Chinese Academy of Sciences, Guiyang, People’s Republic of China chemicals. In recognition of these new threats, The Southeast Asia and Western Pacific regions contain half of the world’s children and are among the evaluation and management of risk to the most rapidly industrializing regions of the globe. -

Living Wage Report Urban Vietnam
Living Wage Report Urban Vietnam Ho Chi Minh City With focus on the Garment Industry March 2016 By: Research Center for Employment Relations (ERC) A spontaneous market for workers outside a garment factory in Ho Chi Minh City. Photo courtesy of ERC Series 1, Report 10 June 2017 Prepared for: The Global Living Wage Coalition Under the Aegis of Fairtrade International, Forest Stewardship Council, GoodWeave International, Rainforest Alliance, Social Accountability International, Sustainable Agriculture Network, and UTZ, in partnership with the ISEAL Alliance and Richard Anker and Martha Anker Living Wage Report for Urban Ho Chi Minh City, Vietnam with focus on garment industry SECTION I. INTRODUCTION ....................................................................................................... 3 1. Background ........................................................................................................................... 4 2. Living wage estimate ............................................................................................................ 5 3. Context ................................................................................................................................. 6 3.1 Ho Chi Minh City .......................................................................................................... 7 3.2 Vietnam’s garment industry ........................................................................................ 9 4. Concept and definition of a living wage ........................................................................... -
Download the Resource Guide
BIG COAT MEDIA 1 MICHAEL + BECKY Michael and Becky loved their sizeable lot and house when they first purchased it six years ago. Unfortunately, the finishes inside the house are artifacts of the 1970’s and their plans to update it have taken a back seat to their busy family life. Michael loves their large family room and bar, but Becky feels the entire floor plan is too cut off for entertaining, and simply dated and dysfunctional. She wants an open concept, updated house for her family and guests, but is determined to find a different house that better suits their needs. Michael is not ready to give up on their huge lot and great neighborhood, and hopes Hilary’s ex- pert designs can bring this time capsule of a house into the 21st century. Becky knows David will find them a house that Michael will love entertaining in for decades to come. BIG COAT MEDIA 2 KITCHEN General Contractor: Kusan Construction Lighting: Generation Lighting - Parker Place Mini Pendants | Savoy House - Townsend Pendants Counter Stools: Aidan Gray - Grace Counter Stools Cabinetry: 1st Choice Cabinetry - Perimeter: Bentley Maple White, Island: Bentley Maple Grit, Recessed Cabinetry: Bentley, Maple Grit | SMJ Cabinetry, LLC. Cabinetry Hardware: Schaub - Heathrow Round Knobs and Pulls Custom Roman Shade: Noble Design Home Studio Tile: Mosaic Home Interiors - Wooden White Honed Premium Marble Quartz: Absolute Stone Corporation - Pure Surfaces Calacatta Oro Quartz Appliances: Garner Appliance & Mattress Plumbing Fixtures: Vault Undermount Sinks, Simplice Faucet, HiRise -
EXECUTIVE SUMMARY WHO Library Cataloguing-In-Publication Data
PREVENTING DISEASE THROUGH HEALTHY ENVIRONMENTS Towards an estimate of the environmental burden of disease EXECUTIVE SUMMARY WHO Library Cataloguing-in-Publication Data Prüss-Üstün, Annette. Preventing disease through healthy environments : towards an estimate of the environmental burden of disease : executive summary / Prüss-Üstün A, Corvalán C. 1.Environmental monitoring. 2.Cost of illness. 3.Risk factors. I.Corvalán, Carlos F. II.World Health Organization. III.Title. ISBN 92 4 159420 9 (NLM classification: WA 30.5) ISBN 978 92 4 159420 2 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

EDWARD MOONEY HOUSE (18 BOWERY BUILDING) 1 Borough of Manhattan
~ndmarks Preservation Commission August 23, 19661 Number 1 LP-D084 EDWARD MOONEY HOUSE (18 BOWERY BUILDING) 1 Borough of Manhattan. Built between 1785 and 1789; architect unknown. Landmark Site: Borough of Manhattan Tax Map Block 162, Lot 53. On October 19, 1965, the Landmarks Preservation Commission held a public hearing on the proposed designation as a Landmark of the Edward Mooney House (the 18 Bowery Building) and the proposed designation of the related Landmark Site. (Item No, 56). The hearing had been du~ advertised in accordance ~th the provisions of Law. Two witnesses spoke in favor of designation. There were no speakers in opposition to designation. DESCRIPTION AND ANALYSIS This is the· only know town house surviving in Manhattan which dates from the period of the American Revolution. It was built between 1785 - a scant two years after the British evacuation of the City- and 1789, the year George Washington was inaugurated as first President of the United States and New York City became the first Capital of the nation. The house stands on its original site, at the southeast corner of Pell Street and the Bower,y, and its red brick facade above the street-floor level is in a remarkably good state of preservation, A brick extension, equalling the size of the original structure,. was added in l80J. l The architectural style of the house is EarlY Federal, reflecting strongly its Georgian antecedents in construction, proportions and design details. It is three stories in height, with s finished-garret beneath a gambrel roof, Two features of special note which verif,y the documented age of the building are the hand-hewn timbers framing the roof and the broad width of the front windows in proportion to their height.