2.3.2 Noise Sensitivity 7 References 9
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sweden As a Crossroads: Some Remarks Concerning Swedish Folk
studying culture in context Sweden as a crossroads: some remarks concerning Swedish folk dancing Mats Nilsson Excerpted from: Driving the Bow Fiddle and Dance Studies from around the North Atlantic 2 Edited by Ian Russell and Mary Anne Alburger First published in 2008 by The Elphinstone Institute, University of Aberdeen, MacRobert Building, King’s College, Aberdeen, AB24 5UA ISBN 0-9545682-5-7 About the author: Mats Nilsson works as a senior lecturer in folklore and ethnochoreology at the Department of Ethnology, Gothenburg University, Sweden. His main interest is couple dancing, especially in Scandinavia. The title of his1998 PhD dissertation, ‘Dance – Continuity in Change: Dances and Dancing in Gothenburg 1930–1990’, gives a clue to his theoretical orientation. Copyright © 2008 the Elphinstone Institute and the contributors While copyright in the volume as a whole is vested in the Elphinstone Institute, copyright in individual contributions remains with the contributors. The moral rights of the contributors to be identified as the authors of their work have been asserted in accordance with the Copyright, Designs and Patents Act 1988. This work is licensed under the Creative Commons Attribution- NonCommercial-NoDerivatives 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/. 8 Sweden as a crossroads: some remarks concerning Swedish folk dancing MATS NILSSON his article is an overview of folk dancing in Sweden. The context is mainly the Torganised Swedish folk-dance movement, which can be divided into at least three subcultures. Each of these folk dance subcultural contexts can be said to have links to different historical periods in Europe and Scandinavia. -
New Horizons Magazine from Uppsala University • Issue 1
NEW HORIZONS MAGAZINE FROM UPPSALA UNIVERSITY • ISSUE 1. 2014 theme: E-SCIENCE FROM THE CONTENT: MILLIONS OF IMAGES OF CANCER Page 10 GAME DESIGN IN RAPID DEVELOPMENT Page 26 HANS ROSLING REDRAWS THE MAP Page 36 1 NEW HORIZONS ISSUE 1. 2014 IN THIS ISSUE: THEME: E-SCIENCE 4 Large amounts of data require new tools 8 Computers calculate how the glaciers move 9 Language is difficult för Google’s computers 10 Millions of images of cancer New tools for large amounts of data . 4 He wants to redraw the map. 36 Resources for research 12 Genetic risk More and more information is stored Meet honorary doctor Hans Rosling, who wants AN INCREASINGLY IMPORTANT FACTOR for successful research and inn- 13 In focus: School on a downward slope digitally and is available to many. to show us our new world ovation, is the access to well-functioning research infrastructure. The research becomes more complex and dependent on different types of resources. Some 16 Positive trend for world peace of these are available at Uppsala University, others we gain access to through 20 Researcher profile: Erik Ingelssons driving force national and international collaborations. This ranges from major facilities to databases, libraries, biobanks, laboratories and data storage resources. 24 The shoal of fish is the model in studies of democracy Long-term planning and intelligent funding strategies are required in order for the research infrastructure to maintain a high level of quality. In recent 26 Report: Game design in Visby years, opportunities for external funding have declined. This means that a gre- 30 Student Kajsa Asplund: ”Psychologists are needed” ater financial responsibility for local infrastructure lies with the actual insti- tutions of higher education. -
Report on Inter-Calibration for Selected Sites and Execution of the Statistical Tests on Added Value
EBONE European Biodiversity Observation Network: Design of a plan for an integrated biodiversity observing system in space and time D5.4: Report on inter-calibration for selected sites and execution of the statistical tests on added value Ver 1.0 Document date: 2012-02-17 Document Ref.: EBONE-D5.4-1.0 Authors: Mats Nilsson, Anna Allard, Sören Holm, and Håkan Olsson (SLU) Hans Van Calster and Dirk Bauwens (INBO) www.inbo.be EBONE - Cost-effective design biodiversity monitoring for Europe 1 EC-FPV Contract Ref: ENV-CT-2008-212322 D5.4: Report on inter-calibration for selected sites and execution of the statistical tests on added value Authors: Mats Nilsson, Anna Allard, Sören Holm, and Håkan Olsson (SLU) Hans Van Calster and Dirk Bauwens (INBO) Contents: Integrating in situ data with Earth Observation data for estimating the area coverage of habitats: post-stratification Abstract ................................................................................................................................ 4 Introduction .......................................................................................................................... 5 Objective .............................................................................................................. 6 Materials and methods ....................................................................................................... 6 Study area ............................................................................................................ 6 NILS data ............................................................................................................ -

Here in Liverpool, Both As a Physiologist and a Tourist
Contents Welcome 2 Programme Tuesday, 17 December 4 Wednesday, 18 December 8 Poster Communications 11 General Information 35 Abstracts Symposia 38 Oral Communications 45 Poster Communications 70 Future Physiology 2019: Translating Cellular Mechanisms into Lifelong Health Strategies 17–18 December 2019 Liverpool John Moores University, UK Organised by: Katie Hesketh and Mark Viggars Liverpool John Moores University, UK Welcome As co-organisers of Future Physiology 2019 and on behalf of Liverpool John Moores University and The Physiological Society, we would like to warmly welcome you to Liverpool as guests to attend the second Future Physiology conference. A conference dedicated to the development of early career researchers, which has been organised by early career researchers. The two day meeting will take place at Liverpool John Moores University, on the edge of Liverpool city centre, known worldwide for its culture and heritage in music, sport and art. Across the two days, we are delighted to offer four diverse sessions, eight keynote talks, 20 selected oral presentations and over 90 posters showcasing international experts and current early career researchers supporting the conference’s theme of ‘Translating Cellular Mechanisms into Lifelong Health Strategies’. We hope this conference will inspire you to engage in research and will help you feel a part of a wider community of physiologists. We are also offering four professional development sessions aimed specifically at early career researchers, along with an exciting evening social programme with a Beatles theme at the Hard Days Night Hotel, just a stone’s throw away from the iconic Cavern Club which will provide plenty of chance to network and meet other like-minded physiologists. -

Ladda Ner Den Från Den Nya Hemsidan (
Tävling Träning Tradition www.budokampsport.se Verksamheten 2012 Svenska Budo & Kampsportsförbundet Tävling Träning Tradition Svenska Budo & Kampsportsförbundet är ett specialförbund inom RF (Riksidrottsförbundet) som hyser en lång rad österländska och andra kampsporter. Förbundet bildades 1960. Här berättas om verksamheten under år 2012. Omslagbild framsidan: Uppvisning i taido av Philip Högberg och Syl- vester Sandin på Kampsportsgalan. Baksidan: Guldtsuban, Folkets pris på Kampsportsgalan. Foto: Hamid Shokatyan. budokampsport.se Verksamheten 2012. Svenska Budo & Kampsportsförbundet Redaktion: Jonathan Broberg och Stefan Stenudd © Svenska Budo & Kampsportsförbundet och artikelförfattarna, 2013 Grafisk form av Stefan Stenudd Svenska Budo & Kampsportsförbundet, Stockholm Tryckt hos ScandinavianBook, Århus ISBN 978-91-7894-058-5 (Arriba) Innehåll Gott slut på ett gott år 7 Medaljerna 2012 10 Kampsportsgalan 2012 21 Världsmästare i kickboxning 29 Jodo-framgångar på EM i Bryssel 31 Tre svenska VM-guld i thaiboxning 32 Budokampsport.se mötte Sanny Dahlbeck 34 Budokampsport.se mötte Hanna Sillén 38 Svenska framgångar i EM i iaido 44 Succé under submission wrestling-EM 45 Svensk titelmästare i thaiboxning 46 Kvällen då kampsport var i allas blickfång 47 Kampsportsexperter om UFC 51 Kurt Durewall till idrottens Hall of fame 55 Thaiboxningsgymnasium startas i Varberg 56 August Wallén ska ena MMA-världen 58 Framtiden är vigd åt kampsport 60 Ny i styrelsen – Mats Asplund 62 Böter för illegal MMA-gala 64 Fler ansvarsfulla ambassadörer och ledare 65 Fångad i en bur 69 Aftonbladets satsning på kampsport 73 Tufft för budo 76 Hur många liv räddar kampsporten? 80 Verksamheten 2010 83 Årsredovisning SB&K 99 Resultat 2012 SB&K centralt 106 Svenska Budo & Kampsportsförbundet 5 Reza Madadi, vinnare av Folkets pris – Guldtsuban för andra året i rad, på Kampsportsgalan. -
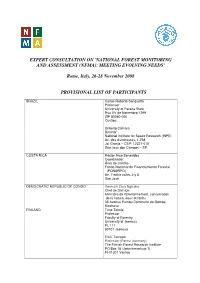
Expert Consultation on 'National Forest Monitoring and Assessment (Nfma): Meeting Evolving Needs'
EXPERT CONSULTATION ON 'NATIONAL FOREST MONITORING AND ASSESSMENT (NFMA): MEETING EVOLVING NEEDS' Rome, Italy, 26-28 November 2008 PROVISIONAL LIST OF PARTICIPANTS BRAZIL Carlos Roberto Sanquetta Professor University of Parana State Rua XV de Novembro 1299 ZIP 80060-000 Curitiba Gilberto Câmara Director National Institute for Space Research (INPE) Av. dos Astronautas, 1.758 Jd. Granja – CEP: 12227-010 São José dos Campos – SP COSTA RICA Héctor Arce Benavides Coordinador Área de Crédito Fondo Nacional de Financiamiento Forestal (FONAFIFO) Av. 7 entre calles 3 y 5 San José DEMOCRATIC REPUBLIC OF CONGO Germain Zasy Ngisako Chef de Division Ministère de l'Environnement, conservation de la nature, eaux et forêts 35 Avenue Pumbu Commune de Gombe Kinshasa FINLAND Timo Tokola Professor Faculty of Forestry University of Joensuu PL 111 80101 Joensuu Erkki Tomppo Professor (Forest Inventory) The Finnish Forest Research Institute PO Box 18 (Jokiniemenkuja 1) FI-01301 Vantaa Jussi Viitanen Adviser (Forest Sector) Department for Development Policy Ministry of Foreign Affairs PO Box 511, Katajanokanlaituri 3 FI-00023 Helsinki GERMANY Christoph Kleinn Director, Center for Tropical and Subtropical Agriculture and Forestry (CeTSAF) Tropenzentrum University of Goettingen Buesgenweg 1 37077 Goettingen Aljoscha Requardt University of Hamburg (UHH)/Johann Heinrich von Thünen-Institute (vTI) Institute for World Forestry International Forest Development and Forest Policy Leuschnerstr. 91 D-21031 Hamburg Germany GUATEMALA Carla Ramírez Zea Consultora para asesoría técnica de la FAO Evaluaciones Nacionales Forestales en Centroamérica Residenciales Bosques de Nejapa, Caso G-87 Guatemala City INDIA Devendra Pandey Director-General Forest Survey of India Ministry of Environment and Forests Dehradun INDONESIA Chaerudin Mangkudisastra Deputy Director for Evaluation of Implementation Forestry Development Plan Ministry of Forestry Manggala Wanabakti Building, Block VII, Level 5, Jl. -

New Sweden Living Tradition of 2011
New Sweden Living Tradition of 2011 Womex A fine selection of outstanding * Folk & World Music from Sweden! NEW Meet Welcome to SWEDEN MCV & at WOMEX MCV musicians from the Stand New Sweden delegation New Sweden! E: 09 / 10 The Musicians’ Own in stand E: 09 / 10 Artist Agency MCV is also participating A fine selection of outstanding in the official Swedish Folk & World Music from Sweden! MCV in collaboration with New Sweden is stand Sweden@ proud to present a selection of top class acts WOMEX. at WOMEX 2011. The musical span, which NEW SWEDEN represents, mirrors a Swe- The Swedish melting pot of ethnicities has den seething of musical junctions. Unique fusions of Folk Music resulted in a literal explosion of musical influences genres, of tradition and innovation, of rural and urban culture, all from all over the globe! give a new meaning to the concept of Living Tradition. The bands of the NEW SWEDEN delegation all originates from the It´s truly exciting to see new styles of music arise, but also to hear west of Sweden, in and around the seaport of Gothenburg, a city musicians embrace a musical genre, and perform original compo- with a long history as a meeting point and cultural hub where music sitions on the highest international level. styles blend and new arise. NEW SWEDEN proudly presents ten of Sweden’s most prominent The MCV office is situated in Gothenburg, the capital of western and acknowledged groups within Folk & World Music. Their music Sweden. The primary purposes of MCV are: has its origin in Nordic, Eastern European, Caribbean, Macedo- • to offer free-of-charge intermediary services between our artists nian, Greek, Arabic and Latin American folk music. -
Arv Nordic Yearbook of Folklore 2012 2 3 ARVARV Nordic Yearbook of Folklore Vol
1 Arv Nordic Yearbook of Folklore 2012 2 3 ARVARV Nordic Yearbook of Folklore Vol. 68 Editor ARNE BUGGE AMUNDSEN OSLO, NORWAY Editorial Board Anders Gustavsson, Oslo; Gustav Henningsen, Copenhagen Bengt af Klintberg, Lidingö; Ann Helene Bolstad Skjelbred, Oslo Ulrika Wolf-Knuts, Åbo (Turku) Published by THE ROYAL GUSTAVUS ADOLPHUS ACADEMY UPPSALA, SWEDEN Distributed by SWEDISH SCIENCE PRESS UPPSALA, SWEDEN 4 © 2012 by The Royal Gustavus Adolphus Academy, Uppsala ISSN 0066-8176 All rights reserved Printed with grants from Vetenskapsrådet (Swedish Research Council), Stockholm, Sweden Articles appearing in this yearbook are abstracted and indexed in Historical Abstracts and America: History and Life 1998– Editorial address: Prof. Arne Bugge Amundsen Department of Culture Studies and Oriental Languages University of Oslo Box 1010 Blindern NO–0315 Oslo, Norway phone + 4722857629 fax + 4722854828 http://www.hf.uio.no/ikos/forskning/publikasjoner/tidsskrifter/arv/index.html Cover: Kirsten Berrum For index of earlier volumes, see http://www.kgaa.nu/tidskrift.php Distributor Swedish Science Press Box 118, SE–751 04 Uppsala, Sweden phone: +46(0)18365566 fax: +46(0)18365277 e-mail: [email protected] Printed in Sweden Textgruppen i Uppsala AB, Uppsala 2012 5 Contents Articles Ane Ohrvik: “… For All Honest Christian and Science-Loving Readers”. Religious Encounters in Early Modern Norwegian Black Books . 7 Nils-Arvid Bringéus: “Nowadays We All Look to Sweden as the Chief Centre of Folklore-work” . 27 Terry Gunnell: Clerics as Collectors of Folklore in Nineteenth- Century Iceland . 45 Arne Bugge Amundsen: The Folk in the Church. Magnus Brostrup Landstad (1812–1880) as a Clerical Folklore Collector . 67 Bjarne Rogan: An Internationalist among Norwegian Folklorists. -
Monday, July 5, 2021
SBHD 2021 – Schedule Monday, July 5, 2021 08:00 Registration and Welcome Coffee 10:00 Roland Eils Opening and welcome remarks Berlin, Germany Session: 1 Precision anatomical mapping of human organs using targeted in situ 10:20 Mats Nilsson Stockholm, Sweden sequencing The Human Lung Cell Atlas in health and disease - revealing unique, disease- 11:00 Martijn Nawijn Groningen, Netherlands associated cell states in asthma 11:40 Maren Büttner scCODA: A bayesian model for compositional single-cell data analysis Neuherberg, Germany Quantitative modelling of clinical data and molecular disease mechanisms in 12:00 Tamara Raschka Sankt Augustin, Germany Alzheimer’s disease via Variational Autoencoder Modular Bayesian Networks Short Talks 12:20 Lunch Break 14:00 Virtual Poster Session 1 Session: 2 15:30 Orit Rozenblatt-Rosen Cell atlases as roadmaps to understanding disease Boston, USA 16:10 Coffee Break Systems engineering of IL-2 Identifies multivalency as a critical, 16:40 Brian Orcutt-Jahns Los Angeles, USA unexplored axis of regulatory T cell-specific therapies Montgomery Multiomics network analysis of three liver diseases using UK Biobank 17:00 Blencowe data Short Talks Los Angeles, USA 17:20 Peter Kharchenko Single-cell transcriptomics and comparative analysis of disease tissues Boston, USA Bree Aldridge 18:00 Design of combination therapies for tuberculosis Boston, USA 18:40 Welcome Reception Tuesday, July 6, 2021 Session: 3 09:00 Niko Beerenwinkel Computational analysis of tumor single-cell sequencing data Zurich, Switzerland Systems level -

Counting Carrots… a Quantitative Cross-Section Study on the Distri- Bution of Motivation Incentives in Central Stock- Holm’S Banks According to Bank-Employees
COUNTING CARROTS… A QUANTITATIVE CROSS-SECTION STUDY ON THE DISTRI- BUTION OF MOTIVATION INCENTIVES IN CENTRAL STOCK- HOLM’S BANKS ACCORDING TO BANK-EMPLOYEES Frank B. Francisson , SH17HP1845 SUPERVISOR: Thomas Marmefelt SÖDERTÖRN UNIVERSITY | Institution of Social Science ECONOMICS | BSc Thesis 15 Credits SPRING TERM 2020 | EXAMINER: Mats Nilsson THE ABSTRACT Counting Carrots… as this cross-section study is entitled studied the distribution of motivation incentives in Central Stockholm’s banking sector and if it varied for different groups of bank- employees, according to bank-employees. This variation in the distribution of employee benefits was examined quantitatively in accordance to three explanatory variables: 1 – Job position, 2 – Bank size and 3 – the Gender of respondents. On account of the above variables, three hypotheses were propounded from: the concept of separating firm ownership and control, economies of scale and experience and the theory on labor market dualism. Concerning Bank size, empirical proof showed that the distribution of employee incentives in Big banks varied more than it did in Small banks thanks to cost and resource saving advantages. Nevertheless, this study was unsuccessful in producing adequate empirical evidence to indicate such variation in motivation incentives when considering employees’ Job position and Gender. This lack of empirical proof contradicted notions from relevant theoretical constructs on divorcing firm ownership from control and from the dual labor market theory. In some respects, conclusions arrived at were not consistent with what Davydenko et al. (2017) observed in Poznan, Poland on a similar topic about incentives diversity. In future, more work remains to be done which should include more features of motivation incentives such as their quality versus quantity or/and their degree of effectiveness in elevating employee engagement with the intent to improve or complement the produced findings from this study. -

Issue 58 BHPC Newsletter - Issue 58
The British Human B H P C Power Club Exclusive!!! First Racing Bike To Conform To New UCI Regulations Revealed! Autumn 1999 Issue 58 BHPC Newsletter - Issue 58 Front Cover: Bike rack outside Barclays Bank, Romsey, Hampshire. Back Cover: I Predict The Future... Contents Events 3 News, Views, and Membership Matters Various 4 Secretarial Stuff Steve ‘n’ Sherri Donaldson 10 Ron’s House Party Ron Beams 12 Advices For Faired Bike Builders Paul Davies 14 2 Plus 1 Harry Fullagar 18 Tyre Rolling Resistance Data John Lafford 21 Tales Of The City Tina Larrington 24 Racing News Dave Larrington, Nigel Sleigh, Clan Donaldson 26 Stop Press!!! Peter Bainbridge, Dave Holladay, John Keen... 39 European Championships 2000 HPV-Belgium 41 Suppliers & Wants 43 Back page Tina Larrington 48 Objectives: The British Human Power Club was formed to foster all aspects of human-powered vehicles - air, land & water - for competitive, recreational and utility activities, to stimulate innovation in design and development in all spheres of HPV's, and to promote and to advertise the use of HPV's in a wide range of activities. Never buy a second- hand boat from a hippie... OFFICERS Chairman & Press Officer Dave Cormie ( Home 0131 552 3148 143 East Trinity Road Edinburgh, EH5 3PP Competition Secretary gNick Green ...is in the middle of moving... E-mail: [email protected] Secretary Steve Donaldson ( Home 01224 772164 Touring Secretary Sherri Donaldson 15 Station Road Dyce, Aberdeen AB21 7BA Treasurer & Membership ...volunteer(s) required - see within Newsletter Editorial Team Dave & Tina Larrington ( Home 0181 531 4496 166 Higham Hill Road (after 19:00 weekdays...) London E17 6EJ E-mail: [email protected] or: [email protected] Librarian Pete Cox ( Home 01244 376776 11a Lorne St Chester CH1 4AE Issue 59 closes: 1st December 1999 (in time for the Millennium Bug!) Letters, articles, pictures, vintage port, etc. -

Full Text.Pdf
THURSDAY MORNING, 17 MAY 2012 HALL B, 8:20 A.M. TO 9:20 A.M. Keynote Lecture Invited Paper 8:20 Acoustics of traditional Chinese theatres. Ji-qing Wang (Institute of Acoustics, Tongji University, Shanghai, Shanghai 200092, China) The traditional Chinese theatre is a unique architectural form. Chinese opera is a form of imaginary performing art; therefore, it does not require large stage and realistic stage settings. A pavilion stage open on three sides and thrusting into the audience area is its com- monly applied characteristic feature. A comparatively low ceiling with elegant dome-like caisson acts as a sound shell, providing benefi- cial reflections to the audience, and to actors on the stage as well. The older generation Chinese opera goers used the term ?going to listen opera??which well explains how they placed great demands on vocal performance. In Chinese theatrical history, there were differ- ent types of theatre from open-air theatre to hall theatre, built both in cities and rural areas all over the country. Nevertheless, the court- yard theatre was the most popular. Up to the present day, thousands of ancient traditional theatres still exist in China, and many of them are well preserved. Interesting results are reported in this paper after acoustical surveys of these theatres. Acoustical issues are raised from these studies, such as, does the classical parameter of reverberation time still adequate for qualifying the acoustics for a roofless courtyard theatre, or for an amphitheatre as well? A primary subjective survey conducted in our laboratory recently presents the negative conclusion. Another presentation is involved in this paper: the puzzle of vase resonators beneath the traditional stage which was long believed to be effective for sound enhancement as recorded in the Chinese historical accounts.