Small Cell Lung Cancer from Traditional to Innovative Therapeutics: Building a Comprehensive Network to Optimize Clinical and Translational Research
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Precision Medicine for Human Cancers with Notch Signaling Dysregulation (Review)
INTERNATIONAL JOURNAL OF MOleCular meDICine 45: 279-297, 2020 Precision medicine for human cancers with Notch signaling dysregulation (Review) MASUKO KATOH1 and MASARU KATOH2 1M & M PrecMed, Tokyo 113-0033; 2Department of Omics Network, National Cancer Center, Tokyo 104-0045, Japan Received September 16, 2019; Accepted November 20, 2019 DOI: 10.3892/ijmm.2019.4418 Abstract. NOTCH1, NOTCH2, NOTCH3 and NOTCH4 are conjugate (ADC) Rova-T, and DLL3-targeting chimeric antigen transmembrane receptors that transduce juxtacrine signals of receptor‑modified T cells (CAR‑Ts), AMG 119, are promising the delta-like canonical Notch ligand (DLL)1, DLL3, DLL4, anti-cancer therapeutics, as are other ADCs or CAR-Ts targeting jagged canonical Notch ligand (JAG)1 and JAG2. Canonical tumor necrosis factor receptor superfamily member 17, Notch signaling activates the transcription of BMI1 proto-onco- CD19, CD22, CD30, CD79B, CD205, Claudin 18.2, fibro- gene polycomb ring finger, cyclin D1, CD44, cyclin dependent blast growth factor receptor (FGFR)2, FGFR3, receptor-type kinase inhibitor 1A, hes family bHLH transcription factor 1, tyrosine-protein kinase FLT3, HER2, hepatocyte growth factor hes related family bHLH transcription factor with YRPW receptor, NECTIN4, inactive tyrosine-protein kinase 7, inac- motif 1, MYC, NOTCH3, RE1 silencing transcription factor and tive tyrosine-protein kinase transmembrane receptor ROR1 transcription factor 7 in a cellular context-dependent manner, and tumor-associated calcium signal transducer 2. ADCs and while non-canonical Notch signaling activates NF-κB and Rac CAR-Ts could alter the therapeutic framework for refractory family small GTPase 1. Notch signaling is aberrantly activated cancers, especially diffuse-type gastric cancer, ovarian cancer in breast cancer, non-small-cell lung cancer and hematological and pancreatic cancer with peritoneal dissemination. -

Predictive QSAR Tools to Aid in Early Process Development of Monoclonal Antibodies
Predictive QSAR tools to aid in early process development of monoclonal antibodies John Micael Andreas Karlberg Published work submitted to Newcastle University for the degree of Doctor of Philosophy in the School of Engineering November 2019 Abstract Monoclonal antibodies (mAbs) have become one of the fastest growing markets for diagnostic and therapeutic treatments over the last 30 years with a global sales revenue around $89 billion reported in 2017. A popular framework widely used in pharmaceutical industries for designing manufacturing processes for mAbs is Quality by Design (QbD) due to providing a structured and systematic approach in investigation and screening process parameters that might influence the product quality. However, due to the large number of product quality attributes (CQAs) and process parameters that exist in an mAb process platform, extensive investigation is needed to characterise their impact on the product quality which makes the process development costly and time consuming. There is thus an urgent need for methods and tools that can be used for early risk-based selection of critical product properties and process factors to reduce the number of potential factors that have to be investigated, thereby aiding in speeding up the process development and reduce costs. In this study, a framework for predictive model development based on Quantitative Structure- Activity Relationship (QSAR) modelling was developed to link structural features and properties of mAbs to Hydrophobic Interaction Chromatography (HIC) retention times and expressed mAb yield from HEK cells. Model development was based on a structured approach for incremental model refinement and evaluation that aided in increasing model performance until becoming acceptable in accordance to the OECD guidelines for QSAR models. -

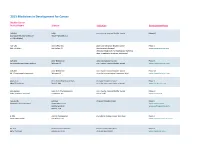
2017 Immuno-Oncology Medicines in Development
2017 Immuno-Oncology Medicines in Development Adoptive Cell Therapies Drug Name Organization Indication Development Phase ACTR087 + rituximab Unum Therapeutics B-cell lymphoma Phase I (antibody-coupled T-cell receptor Cambridge, MA www.unumrx.com immunotherapy + rituximab) AFP TCR Adaptimmune liver Phase I (T-cell receptor cell therapy) Philadelphia, PA www.adaptimmune.com anti-BCMA CAR-T cell therapy Juno Therapeutics multiple myeloma Phase I Seattle, WA www.junotherapeutics.com Memorial Sloan Kettering New York, NY anti-CD19 "armored" CAR-T Juno Therapeutics recurrent/relapsed chronic Phase I cell therapy Seattle, WA lymphocytic leukemia (CLL) www.junotherapeutics.com Memorial Sloan Kettering New York, NY anti-CD19 CAR-T cell therapy Intrexon B-cell malignancies Phase I Germantown, MD www.dna.com ZIOPHARM Oncology www.ziopharm.com Boston, MA anti-CD19 CAR-T cell therapy Kite Pharma hematological malignancies Phase I (second generation) Santa Monica, CA www.kitepharma.com National Cancer Institute Bethesda, MD Medicines in Development: Immuno-Oncology 1 Adoptive Cell Therapies Drug Name Organization Indication Development Phase anti-CEA CAR-T therapy Sorrento Therapeutics liver metastases Phase I San Diego, CA www.sorrentotherapeutics.com TNK Therapeutics San Diego, CA anti-PSMA CAR-T cell therapy TNK Therapeutics cancer Phase I San Diego, CA www.sorrentotherapeutics.com Sorrento Therapeutics San Diego, CA ATA520 Atara Biotherapeutics multiple myeloma, Phase I (WT1-specific T lymphocyte South San Francisco, CA plasma cell leukemia www.atarabio.com -

The Two Tontti Tudiul Lui Hi Ha Unit
THETWO TONTTI USTUDIUL 20170267753A1 LUI HI HA UNIT ( 19) United States (12 ) Patent Application Publication (10 ) Pub. No. : US 2017 /0267753 A1 Ehrenpreis (43 ) Pub . Date : Sep . 21 , 2017 ( 54 ) COMBINATION THERAPY FOR (52 ) U .S . CI. CO - ADMINISTRATION OF MONOCLONAL CPC .. .. CO7K 16 / 241 ( 2013 .01 ) ; A61K 39 / 3955 ANTIBODIES ( 2013 .01 ) ; A61K 31 /4706 ( 2013 .01 ) ; A61K 31 / 165 ( 2013 .01 ) ; CO7K 2317 /21 (2013 . 01 ) ; (71 ) Applicant: Eli D Ehrenpreis , Skokie , IL (US ) CO7K 2317/ 24 ( 2013. 01 ) ; A61K 2039/ 505 ( 2013 .01 ) (72 ) Inventor : Eli D Ehrenpreis, Skokie , IL (US ) (57 ) ABSTRACT Disclosed are methods for enhancing the efficacy of mono (21 ) Appl. No. : 15 /605 ,212 clonal antibody therapy , which entails co - administering a therapeutic monoclonal antibody , or a functional fragment (22 ) Filed : May 25 , 2017 thereof, and an effective amount of colchicine or hydroxy chloroquine , or a combination thereof, to a patient in need Related U . S . Application Data thereof . Also disclosed are methods of prolonging or increasing the time a monoclonal antibody remains in the (63 ) Continuation - in - part of application No . 14 / 947 , 193 , circulation of a patient, which entails co - administering a filed on Nov. 20 , 2015 . therapeutic monoclonal antibody , or a functional fragment ( 60 ) Provisional application No . 62/ 082, 682 , filed on Nov . of the monoclonal antibody , and an effective amount of 21 , 2014 . colchicine or hydroxychloroquine , or a combination thereof, to a patient in need thereof, wherein the time themonoclonal antibody remains in the circulation ( e . g . , blood serum ) of the Publication Classification patient is increased relative to the same regimen of admin (51 ) Int . -

Gastrointestinal Cancer Tumor Panel
POST-TEST Gastrointestinal Cancer Tumor Panel: Clinical Investigators Provide Their Perspectives on Current Cases and Clinical Issues in the Management of Colorectal, Gastric and Pancreatic Cancer THE CORRECT ANSWER IS INDICATED WITH YELLOW HIGHLIGHTING. 1. The Phase III TML trial evaluating 5. The results from the Phase III bevacizumab beyond disease progression RECOURSE trial of TAS-102 for patients for patients with metastatic colorectal with metastatic colorectal cancer cancer demonstrated a statistically refractory to standard therapies demon- significant improvement in overall strated a statistically significant improve- survival (OS) with bevacizumab beyond ment in ___________ with TAS-102/best progression compared to chemotherapy supportive care compared to placebo/ alone. best supportive care. a. True a. OS b. False b. Progression-free survival c. Both a and b 2. Similar to those with other agents in d. Neither a nor b the same class, the adverse events of note that were associated with the VEGF 6. Results from the Phase II RECAP trial inhibitor ramucirumab on the RAISE trial of capecitabine in combination with include ___________. ___________ or placebo as second-line a. Bleeding/hemorrhage therapy for patients with metastatic b. Hypertension pancreatic cancer indicated improved c. Proteinuria OS with that agent in a subgroup of d. Both a and b patients with high C-reactive protein levels. e. All of the above a. Ruxolitinib 3. The ongoing Phase III JACOB trial is b. Brivanib evaluating chemotherapy/trastuzumab c. Nanoparticle albumin-bound (nab) with or without ___________ as first-line paclitaxel therapy for patients with HER2-positive metastatic gastric or gastroesophageal- 7. -

High Delta-Like Ligand 4 Expression Correlates with a Poor Clinical
Journal of Cancer 2019, Vol. 10 3172 Ivyspring International Publisher Journal of Cancer 2019; 10(14): 3172-3178. doi: 10.7150/jca.30257 Research Paper High delta-like ligand 4 expression correlates with a poor clinical outcome in gastric cancer Youjin Kim1,2*, Sun-ju Byeon3,4*, Joonyoung Hur1, Kangkook Lee1, Dongin Kim5, Jin-Hyung Ahn5, Sang Hoon Lee5, Weon-Kyoo You5, Seung Tae Kim1, Se Hoon Park1, Won Ki Kang1, Kyoung-Mee Kim3, Jeeyun Lee1 1. Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea 2. Division of Hematology-Oncology, Department of Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea 3. Department of Pathology and Translational Genomics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea 4. Department of Pathology, Hallym University Dongtan Sacred Heart Hospital, Korea 5. ABL Bio, Korea *Equal contributing authors Corresponding authors: Jeeyun Lee, MD, Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul, 06351 (Korea). Tel. +82 2 3410 1779; Fax +82 2 3410 1754; Email: [email protected] and Kyoung-Mee Kim, MD, Department of Pathology and Translational Genomics, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul, 06351 (Korea). Tel. +82 2 3410 2807; Fax +82 2 3410 1754; Email: [email protected] © Ivyspring International Publisher. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY-NC) license (https://creativecommons.org/licenses/by-nc/4.0/). -

WO 2016/176089 Al 3 November 2016 (03.11.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/176089 Al 3 November 2016 (03.11.2016) P O P C T (51) International Patent Classification: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, A01N 43/00 (2006.01) A61K 31/33 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, (21) International Application Number: KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, PCT/US2016/028383 MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (22) International Filing Date: PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, 20 April 2016 (20.04.2016) SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of regional protection available): ARIPO (BW, GH, (30) Priority Data: GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, 62/154,426 29 April 2015 (29.04.2015) US TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, (71) Applicant: KARDIATONOS, INC. [US/US]; 4909 DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, Lapeer Road, Metamora, Michigan 48455 (US). -

ABOUT the TEST: PATIENT RESULTS TUMOR TYPE: BREAST CARCINOMA (NOS) Genomic Alterations Identified† Additional Findings† THER
Patient Name Report Date Tumor Type Breast carcinoma (NOS) Date of Birth Medical Facility Sex Female Ordering Physician Specimen Received FMI Case # Additional Recipient Specimen Site Lung Medical Record # Medical Facility ID # Date of Collection Specimen ID Pathologist Specimen Type ABOUT THE TEST: FoundationOne™ is a next-generation sequencing (NGS) based assay that identifies genomic alterations within hundreds of cancer-related genes. PATIENT RESULTS TUMOR TYPE: BREAST CARCINOMA (NOS) 20 genomic findings Genomic Alterations Identified† ERBB2 R678Q 13 therapies associated with potential clinical benefit ⧺ ⧺ PIK3CA H1047R – subclonal , N1044K, R88Q – subclonal , V344M – subclonal⧺ 0 therapies associated with lack of response TSC1 L203fs*7 ARID1A splice site 2420-2A>G 34 clinical trials ASXL1 G645fs*58 LZTR1 Q10fs*24 MLH1 S446fs*32, V267fs*1 MLL2 A1105fs*14 MSH2 A230fs*16 NOTCH3 A2233fs*9 PPP2R1A R183W – subclonal⧺ RAD50 N934fs*6 SETD2 R1492* SMARCA4 R1157W Additional Findings† Microsatellite status MSI-High Tumor Mutation Burden TMB-High; 26 Muts/Mb † For a complete list of the genes assayed and performance specifications, please refer to the Appendix ⧺ See Appendix for details THERAPEUTIC IMPLICATIONS Genomic Findings FDA-Approved Therapies FDA-Approved Therapies Potential Clinical Trials Detected (in patient’s tumor type) (in another tumor type) ERBB2 Ado-trastuzumab emtansine Afatinib Yes, see clinical trials R678Q Lapatinib section Neratinib Pertuzumab Trastuzumab For more comprehensiveSAMPLE information please log on to the Interactive Cancer Explorer™ To set up your Interactive Cancer Explorer account, contact your sales representative or call 1-888-988-3639. Electronically Signed by Sample Preparation: 7010 Kit Creek Road, Morrisville, NC 27560 / CLIA:34D2044309 Foundation Medicine, Inc. -

2016 Medicines in Development for Rare Diseases a LIST of ORPHAN DRUGS in the PIPELINE
2016 Medicines in Development for Rare Diseases A LIST OF ORPHAN DRUGS IN THE PIPELINE Autoimmune Diseases Product Name Sponsor Official FDA Designation* Development Status Actemra® Genentech treatment of systemic sclerosis Phase III tocilizumab South San Francisco, CA www.gene.com Adempas® Bayer HealthCare Pharmaceuticals treatment of systemic sclerosis Phase II riociguat Whippany, NJ www.pharma.bayer.com ARA 290 Araim Pharmaceuticals treatment of neuropathic pain in patients Phase II Tarrytown, NY with sarcoidosis www.ariampharma.com ARG201 arGentis Pharmaceuticals treatment of diffuse systemic sclerosis Phase II (type 1 native bovine skin Collierville, TN www.argentisrx.com collagen) BYM338 Novartis Pharmaceuticals treatment of inclusion body myositis Phase III (bimagrumab) East Hanover, NJ www.novartis.com CCX168 ChemoCentryx treatment of anti-neutrophil cytoplasmic Phase II (5a receptor antagonist) Mountain View, CA auto-antibodies associated vasculitides www.chemocentryx.com (granulomatosis with polyangitis or Wegener's granulomatosis), microscopic polyangitis, and Churg-Strauss syndrome * This designation is issued by the FDA's Office of Orphan Products Development while the drug is still in development. The designation makes the sponsor of the drug eligible for entitlements under the Orphan Drug Act of 1983. The entitlements include seven years of marketing exclusivity following FDA approval of the drug for the designated use. Medicines in Development: Rare Diseases | 2016 1 Autoimmune Diseases Product Name Sponsor Official FDA -
Adis R&D Insight
2015 Medicines in Development for Cancer Bladder Cancer Product Name Sponsor Indication Development Phase ABI-009 AADi non-muscle invasive bladder cancer Phase I/II (nanoparticle albumin-bound Pacific Palisades, CA mTOR inhibitor) ACP-196 Acerta Pharma platinum-refractory bladder cancer Phase II (Btk inhibitor) San Carlos, CA (combination therapy) www.acerta-pharma.com (see also head/neck, hematological, leukemia, lung, lymphoma, myeloma, pancreatic) ALT-801 Altor BioScience advanced bladder cancer, Phase II (immunotherapy fusion protein) Miramar, FL non-muscle invasive bladder cancer www.altorbioscience.com ALT-803 Altor BioScience non-muscle invasive bladder cancer Phase I/II (IL-15 superagonist complex) Miramar, FL (see also hematological, myeloma, skin) www.altorbioscience.com apatorsen OncoGenex Pharmaceuticals metastatic bladder cancer Phase II (Hsp27 inhibitor) Bothell, WA (see also lung, pancreatic, prostate) www.oncogenex.com apaziquone Spectrum Pharmaceuticals non-muscle invasive bladder cancer Phase III (DNA synthesis inhibitor) Henderson, NV (Fast Track) www.sppirx.com ASG-15ME Agensys relapsed bladder cancer Phase I (antibody drug conjugate) Santa Monica, CA www.agensys.com Seattle Genetics www.seattlegenetics.com Bothell, WA B-701 BioClin Therapeutics metastatic bladder cancer (2nd-line) Phase II (anti-FGFR3 mAb) San Ramon, CA www.bioclintherapeutics.com BC-819 BioCancell Therapeutics bladder cancer (2nd-line) Phase II (gene therapy) Jerusalem, Israel (see also pancreatic) www.biocancell.com Bladder Cancer Product Name Sponsor -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Management of Metastatic Pancreatic Adenocarcinoma
Management of Metastatic Pancreatic Adenocarcinoma a,b c,d, Ahmad R. Cheema, MD , Eileen M. O’Reilly, MD * KEYWORDS Pancreatic cancer Metastatic disease Gemcitabine Nab-paclitaxel FOLFIRINOX Targeted agents Immune therapy KEY POINTS Progress in the treatment of pancreatic ductal adenocarcinoma (PDAC) has been incre- mental, mainly ensuing from cytotoxic systemic therapy, which continues to be a standard of care for metastatic disease. Folinic acid, 5-fluorouracil (5-FU), irinotecan, and oxaliplatin (FOLFIRINOX) and gemcita- bine plus nab-paclitaxel have emerged as new standard therapies, improving survival in patients with good performance status. Novel therapeutics targeting the peritumoral stroma and tumor-driven immune suppres- sion are currently a major focus of research in metastatic disease. Identification of reliable and validated predictive biomarkers to optimize therapeutics con- tinues to be a challenge. Continued efforts toward better understanding of tumor biology and developing new drugs are warranted because a majority of patients succumb within a year of diagnosis, despite an increasing number of therapeutic options available today. INTRODUCTION In the year 2016, there will be approximately 53,000 estimated new individuals diag- nosed with PDAC in the United States, representing approximately 3% of all cancer Financial Disclosures: None (A.R. Cheema). Research support: Sanofi Pharmaceuticals, Celgene, Astra-Zenica, MedImmune, Bristol-Myers Squibb, Incyte, Polaris, Myriad Genetics, Momenta Pharmaceuticals, OncoMed. Consulting: Celgene, MedImmune, Sanofi Pharmaceutical, Threshold Pharmaceuticals, Gilead, Merrimack (E.M. O’Reilly). Funding support: Cancer Center Support Grant (P30 CA008748). a Department of Medicine, Icahn School of Medicine at Mount Sinai, 1 Gustave Levy Pl, New York, NY 10029, USA; b Department of Medicine, Mount Sinai St.