Orthodontic Treatment for Crowded Teeth in Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
1 Self-Ligating Brackets
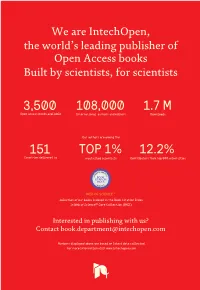
We are IntechOpen, the world’s leading publisher of Open Access books Built by scientists, for scientists 3,500 108,000 1.7 M Open access books available International authors and editors Downloads Our authors are among the 151 TOP 1% 12.2% Countries delivered to most cited scientists Contributors from top 500 universities Selection of our books indexed in the Book Citation Index in Web of Science™ Core Collection (BKCI) Interested in publishing with us? Contact [email protected] Numbers displayed above are based on latest data collected. For more information visit www.intechopen.com 1 Self-Ligating Brackets: An Overview Maen Zreaqat and Rozita Hassan School of Dental Sciences, Universiti Sains Malaysia, Kelantan, Malaysia 1. Introduction The specialty of orthodontics has continued to evolve since its advent in the early 20th century. Changes in treatment philosophy, mechanics, and appliances have helped shape our understanding of orthodontic tooth movement. In the 1890‘s, Edward H. Angle published his classification of malocclusion based on the occlusal relationships of the first molars. This was a major step toward the development of orthodontics because his classification defined normal occlusion. Angle then helped to pioneer the means to treat malocclusions by developing new orthodontic appliances. He believed that if all of the teeth were properly aligned, then no deviation from an ideal occlusion would exist. Angle and his followers strongly believed in non-extraction treatment. His appliance, (Fig. 1), consisted of a tube on each tooth to provide a horizontally positioned rectangular slot. Angle’s edgewise appliance received its name because the archwire was inserted at a 90-degree angle to the plane of insertion. -

Contemporary Esthetic Orthodontic Archwires – a Review
Review Article Contemporary Esthetic Orthodontic Archwires – A Review Jitesh Haryani1, Rani Ranabhatt2 1Senior Resident, Department of Orthodontics and Dentofacial Orthopaedics, Faculty of Dental Sciences, King George’s Medical University, Lucknow, Uttar Pradesh, India 2 Junior Resident, Department of Prosthodontics, Faculty of Dental Sciences, King George’s Medical University, Lucknow, Uttar Pradesh, India Received 2 February 2016 and Accepted 9 June 2016 Abstract Introduction Growing demand of invisible braces by esthetically With increasing number of adult patients seeking conscious patients has led to remarkable inventions in orthodontic treatment, the demand for esthetic orthodontic materials for esthetic labial archwires. Archwires with appliances has increased dramatically, creating a need for the excellent optical clarity and mechanical properties so-called invisible orthodontic appliances like Invisalign (1) and lingual braces (2). However, esthetics of fixed labial comparable to conventional archwires have been appliances has also evolved by inclusion of ceramic brackets3, manufactured by almost all the leading companies of esthetic ligatures and tooth colored archwires. Attractiveness orthodontic products in the past two decades, but their evaluation reveals that sapphire brackets with esthetic clinical use is still limited. Esthetic archwires can be archwires are preferred just next to clear aligner trays.4 to divided into two main types, which are transparent non- complement the esthetic brackets with invisible archwires, metallic archwires (composite wires) and metallic wires esthetic archwires have rapidly evolved in the last decade.(5). with esthetic coatings. This article intends to provide an Esthetic archwire materials are basically a composite overview of various types of esthetic archwires of two materials which can be broadly classified into available, and to gather evidence from the literature two major groups (5,6). -

The Effects of Elastic Size and Archwire Type on 3-Dimensional Force Systems When Using Class II Interarch Elastics
The Effects of Elastic Size and Archwire Type on 3-Dimensional Force Systems When Using Class II Interarch Elastics by Joseph Stanley A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science Medical Sciences – Orthodontics University of Alberta ©Joseph Stanley, 2017 Abstract Objectives: An orthodontic simulator (OSIM) device was used to compare the force systems generated by class II elastics on a ½ cusp class II malocclusion using four combinations of two elastic types and two archwire types. Methods: 3-dimensional forces and moments due to class II elastics were measured individually for each tooth (7-7) using Damon Q brackets on the maxillary and mandibular arches. Four test groups (n=44) were compared, each of a different combination of two elastic types (3/16", 2oz and 4.5oz) and two archwire types (0.014" nickel titanium and 0.019" x 0.025" stainless steel). Results: Only the upper canines and lower first molars recorded clinically significant forces (0.3N) and moments (5Nmm). 2oz and 4.5oz class II elastics produced clinically significant vertical extrusive forces and horizontal forces along the archwire to normalize a class II malocclusion. Stainless steel archwire minimized the extrusive forces of the 4.5oz elastics compared to nickel titanium archwire Conclusions: 2oz and 4oz class II elastics produced clinically significant vertical extrusive forces and horizontal forces along the archwire. Archwire type had no effect on 2oz class II elastics whereas 0.019" x 0.025"stainless steel significantly reduced the vertical extrusive effects of the larger 4.5oz elastics. ii Dedication To Jennifer, this was a tag team effort. -

Coated and Uncoated Nickel-Titanium Archwires: Mechanical Property
COATED AND UNCOATED NICKEL-TITANIUM ARCHWIRES: MECHANICAL PROPERTY AND SURFACE TOPOGRAPHY RESPONSE TO A SIMULATED ORAL ENVIRONMENT WITH AND WITHOUT BRACKET-RELATED LOAD-DEFLECTION INDUCED STRESS A THESIS IN Oral and Craniofacial Sciences Presented to the Faculty of the University of Missouri-Kansas City in partial fulfillment of the requirements for the degree MASTER OF SCIENCE by KELCEY LOVELAND B.S., Utah State University, 2008 D.M.D., University of Nevada – Las Vegas, 2015 Kansas City, Missouri 2017 COATED AND UNCOATED NICKEL-TITANIUM ARCHWIRES: MECHANICAL PROPERTY AND SURFACE TOPOGRAPHY RESPONSE TO A SIMULATED ORAL ENVIRONMENT WITH AND WITHOUT BRACKET-RELATED LOAD DEFLECTION INDUCED STRESS Kelcey Loveland, DMD, Candidate for the Master of Science Degree University of Missouri-Kansas City, 2017 ABSTRACT This study examined the effect of exposure to bracket-related load deflection on the mechanical properties and surface characteristics of esthetic coated and uncoated nickel- titanium archwires. Two types of coated archwires were tested: one with a rhodium ion coating and another with a polymer coating. Corresponding uncoated wires of the same size were also tested. These four different wires were divided into treatment groups based on exposure to bracket-related load deflection and storage in PBS at 37±1°C. A three-point bend test in DI water at 37±1°C was performed on specimens at three time points: 4 weeks, 8 weeks, and 12 weeks. Unloading forces at 1, 2, and 3 mm of deflection were recorded. After 12 weeks exposure, three representative specimens from each treatment group along with untested wires were viewed using scanning electron microscopy (SEM) to provide a qualitative surface topography analysis. -

Metal Free Orthodontics: a Review
I J Pre Clin Dent Res 2014;1(4):100-106 International Journal of Preventive & October-December Clinical Dental Research All rights reserved Metal Free Orthodontics: A Review Abstract With the increase in the number of adults undergoing orthodontic 1 2 Syed Rafiuddin , Reji Abraham treatment, there has been a corresponding increase in demand for more esthetic orthodontic appliances. These new appliances combine both 1Senior Lecturer, Department of Orthodontics acceptable esthetics and adequate technical performance. This article & Dentofacial Orthopedics, Sri Hasanamba presents the currently available appliances and discusses the potential Dental College & Hospital, Hassan, Karnataka, problems associated with each. Recent advances have also been India 2Professor, Department of Orthodontics & described. Dentofacial Orthopedics, Sri Hasanamba Key Words Dental College & Hospital, Hassan, Karnataka, Esthetics; brackets; archwires India INTRODUCTION to moderate alignment cases, especially in the adult Since 1990’s there has been a growing demand for patient. However, complex cases still require fixed esthetic orthodontic appliances. Orthodontic appliance treatment and numerous brackets & patients, including a growing population of adults, archwires are now available for those clinicians and not only want an improved smile, but they are also patients that are aesthetically orientated. increasingly demanding better aesthetics during BRACKETS treatment. This demand has led to the development Two of the materials used for traditional aesthetic of orthodontic appliances with acceptable esthetics bracket manufacturing are plastic and ceramic both for patients and clinicians. The development of brackets. appliances that combine both acceptable aesthetics Plastic Brackets for the patient and adequate technical performance Plastic brackets were introduced into the market in for the clinician is the ultimate goal. -

Orthodontic Arch Wires
European Journal of Molecular & Clinical Medicine ISSN 2515-8260 Volume 07, Issue 8, 2020 Orthodontic Arch Wires Dr. Saikrupa ganeshan¹, Dr.Padmavati², Dr.M.S.Kannan³ ¹post graduate student, Sree Balaji Dental College and Hospital, Pallikaranai, Chennai- 100 ²senior lecturer, department of orthodontics and Dentofacial orthopaedics, Sree Balaji Dental College and Hospital, Pallikaranai, Chennai -100 ³Head of the Department, Department of Orthodontics and Dentofacial Orthopaedics, Sree Balaji Dental College and Hospital, Pallikaranai, Chennai -100 Abstract: The materials used by orthodontists have changed rapidly in the last 8 decades and will continue to do so in the future. As esthetic wires are introduced, metallic wires will likely be replaced for most orthodontic applications. Wires are assessed by their properties like strength, stiffness, range, formability and weldability. As an ideal archwire has not yet been found, archwires should be selected within the context of their intended use during treatment. This article throws light on the different types of archwires available for orthodontic use. INTRODUCTION: The archwire has been an integral part of the orthodontic appliance, ever since Dr. Edward Angle placed the first appliance into the patient’s mouth. Archwires are designed to move teeth with light continuous forces. These forces may reduce the potential for patient discomfort, tissue hyalinization and undermining resorption. Archwire should behave elastically when a force is applied. To achieve this various archwires are available. Stainless Steel Wires: Stainless steel was first introduced by Dr. F.Hauptmeyer during the First World War at Krupp’s dental polyclinic in Germany for making the prosthesis. The refinement of the drawing process to form wires was invented in the late 1930s by ANGLE. -

Copper, Aluminum and Nickel: a New Monocrystalline Orthodontic Alloy Mark Wierenga
Loma Linda University TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works Loma Linda University Electronic Theses, Dissertations & Projects 9-2014 Copper, Aluminum and Nickel: A New Monocrystalline Orthodontic Alloy Mark Wierenga Follow this and additional works at: http://scholarsrepository.llu.edu/etd Part of the Orthodontics and Orthodontology Commons Recommended Citation Wierenga, Mark, "Copper, Aluminum and Nickel: A New Monocrystalline Orthodontic Alloy" (2014). Loma Linda University Electronic Theses, Dissertations & Projects. 195. http://scholarsrepository.llu.edu/etd/195 This Thesis is brought to you for free and open access by TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works. It has been accepted for inclusion in Loma Linda University Electronic Theses, Dissertations & Projects by an authorized administrator of TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works. For more information, please contact [email protected]. LOMA LINDA UNIVERSITY School of Dentistry in conjunction with the Faculty of Graduate Studies ____________________ Copper, Aluminum and Nickel: A New Monocrystalline Orthodontic Alloy by Mark Wierenga ____________________ A Thesis submitted in partial satisfaction of the requirements for the degree Master of Science in Orthodontics and Dentofacial Orthopedics ____________________ September 2014 © 2014 Mark Wierenga All Rights Reserved Each person whose signature appears below certifies that this thesis in his opinion is adequate, in scope and quality, as a thesis for the degree of Master of Science. , Chairperson V. Leroy Leggitt, Professor of Orthodontics Gregory Olson, Associate Professor of Orthodontics and Pediatric Dentistry Kitichai Rungcharassaeng, Professor of Orthodontics iii ACKNOWLEDGEMENTS I would like to express my appreciation to the individuals who helped me complete this study. -

Effects of Nickel-Titanium and Stainless Steel Leveling Wires on the Position of Mandibular Incisors
A RTIGO I NÉDITO Efeitos dos fios de nivelamento de níquel-titânio e de aço inoxidável na posição dos incisivos inferiores Ricardo Moresca*, Alexandre Moro**, Gladys Cristina Dominguez***, Julio Wilson Vigorito**** Resumo Objetivo: estudar os efeitos do nivelamento realizado com fios de NiTi termoativado e de aço inoxidável, avaliando-se as possíveis alterações na posição dos incisivos inferiores, em casos com extrações, correlacionando com o tempo de tratamento. Métodos: a amostra foi composta de 36 indivíduos, de ambos os sexos, leucodermas brasileiros, com idade média inicial de 15 anos e 5 meses, portadores de más oclusões de Classes I e II, distribuídos em dois grupos. No Grupo 1 (n=17), o nivelamento foi realizado com a sequência 1, utilizan- do-se três fios — 0,016” e 0,019”x0,025” de NiTi termoativado, e 0,019”x0,025” de aço inoxidável. No Grupo 2 (n=19), foi testada a sequência 2, na qual foram utilizados apenas fios de aço inoxidável (0,014”; 0,016”; 0,018”; 0,020” e 0,019”x0,025” com torque passivo nos incisivos inferiores). Os dados foram coletados utilizando-se o método cefalométrico computadorizado e comparados pelo teste t de Student com o nível de significância de 5%. Resultados: no Grupo 1, os incisivos inferiores inclinaram-se para lingual, com movimento significativo apenas da coroa (1,6mm). No Grupo 2, os incisivos inferiores permaneceram estáveis. Não houve alteração vertical em nenhum dos grupos. Conclusões: a sequência 2 proporcionou um melhor controle dos incisivos inferiores, não alterando suas posições ini- ciais, enquanto a sequência 1 permitiu a expressão do torque da prescrição utilizada, levan- do a uma inclinação lingual desses dentes. -

Orthodontics 2018
1 Orthodontics 2018 Contents Brackets 2-5 Bands 6-7 Buccal tubes 8-9 Wire Products 10-15 Accessories 16-24 Instruments 25-55 Lab Supplies 56-69 Appliances 70-77 InterProximal Reduction 78-83 Mini screws 84-87 Miscellaneous 88-96 2 Magic Miniature Twin Brackets BRACKETS Provide all the proven clinical characteristics of full size brackets, in a smaller size and low profi le design for greater comfort and improved aesthetics. Roth Prescription / MBT. Product Code Set 20 pcs (with hook #3, 4, 5) MG-MINI-M-BRACKET Single bracket MG-S-M-BRACKET Magic Ceramic Brackets Give patients the look they want with the functionality they need: Aesthetically pleasing with consistent and reliable bonding/debonding performance. Those ceramic brackets represent an excellent alternative to metal brackets. Roth Prescription / MBT. Product Code Set 20 pcs (with hook #3, 4, 5) MG-CER-BRACKETS Single bracket MG-S-M-BRACKET Magic 2d Lingual Brackets 2D brackets are smaller and have reduced thickness. These brackets most comfortable and cost-effective fi tted behind the patient teeth, rendering them practically invisible to others. Extremely fl at construction that is great for patient’s comfort. It is a simple and inexpensive alternative. Product Code Set 28 pcs MG-LINGUAL2D Slim Prescription Edgewise Brackets System An Advanced Morelli slim edgewise brackets are considered as a universal aesthetic solution for a large variety of cases. Thanks to being an edgewise these slim brackets can be used on any teeth surface with any angle correction and can be rotated as needed. Product Code Set 20 pcs MO-10-65-902 SLP Ligating Passive Prescription Roth Brackets Brackets with SLP (Self Ligating Passive) allow several treatment possibilities due to the lower friction of the set. -

Root Resorption Associated with Orthodontic Tooth Movement: a Systematic Review
Root resorption associated with orthodontic tooth movement: A Systematic Review A Thesis Presented in Partial Fulfillment of the Requirement for The Degree Master of Science in the Graduate School of The Ohio State University By Belinda Jessica Weltman, H.B.Sc., D.M.D., M.Sc. ***** The Ohio State University 2009 Master‘s Examination Committee: Dr. Katherine Vig, Advisor Approved by: Dr. Henry W. Fields, Jr. Dr. Shiva Shanker __________________________ Dr. Eloise Kaizar Advisor Graduate Program in Dentistry ABSTRACT Background It is generally accepted that one of the risks associated with orthodontic treatment is apical root resorption. Currently the orthodontic literature on root resorption does not provide a consensus on the factors associated with the onset, severity, and management of root resorption. Root resorption may affect the long-term prognosis and stability of the dentition, which is a compelling reason to identify causal factors so that the risks may be minimized, and the amount of root resorption reduced. Objective To evaluate root resorption as a primary outcome for a population of patients who received orthodontic tooth movement, in order to provide the best available evidence upon which clinical decisions can be made to minimize the risks and severity of root resorption. Search strategy Electronic databases were searched, non-electronic journals hand searched and experts in the field consulted. No language restrictions were placed. Additional missing information was obtained by contacting study authors. ii Selection criteria The following criteria were met for study selection: a randomized clinical trial involving human subjects for orthodontic tooth movement, with fixed appliances, and recording root resorption during or after treatment. -

Effectiveness of Medical Coating Materials in Decreasing Friction Between Orthodontic Brackets and Archwires
THE KOREAN JOURNAL of Original Article ORTHODONTICS pISSN 2234-7518 • eISSN 2005-372X https://doi.org/10.4041/kjod.2021.51.4.270 Effectiveness of medical coating materials in decreasing friction between orthodontic brackets and archwires Nursel Aricia Objective: The aim of this in vitro study was to evaluate the changes in friction b Berat S. Akdeniz between orthodontic brackets and archwires coated with aluminum oxide (Al2O3), Abdullah A. Oza titanium nitride (TiN), or chromium nitride (CrN). In addition, the resistance Yucel Gencerc of the coatings to intraoral conditions was evaluated. Methods: Stainless steel Mehmet Tarakcic canine brackets, 0.016-inch round nickel–titanium archwires, and 0.019 × a Selim Arici 0.025-inch stainless steel archwires were coated with Al2O3, TiN, and CrN using radio frequency magnetron sputtering. The coated materials were examined using scanning electron microscopy, an X-ray diffractometer, atomic force microscopy, and surface profilometry. In addition, the samples were subjected to thermal cycling and in vitro brushing tests, and the effects of the simulated a intraoral conditions on the coating structure were evaluated. Results: Coating Department of Orthodontics, Faculty of Dentistry, Ondokuz Mayıs University, of the metal bracket as well as nickel–titanium archwire with Al2O3 reduced the Samsun, Turkey coefficients of friction (CoFs) for the bracket–archwire combination (p < 0.01). bDepartment of Orthodontics, Faculty When the bracket and stainless steel archwire were coated with Al2O3 and TiN, of Dentistry, Kırıkkale University, the CoFs were significantly lower (0.207 and 0.372, respectively) than that Kırıkkale, Turkey recorded when this bracket–archwire combination was left uncoated (0.552; cMaterials Science and Engineering p < 0.01). -

An Archwire for Non-Invasive Improvement of Occlusal Cant And
www.apospublications.com APOS Trends in Orthodontics Special Feature An archwire for non-invasive improvement of occlusal cant and soft tissue chin deviation Eric Jein-Wein Liou1, Kunal Mehta2,3,4, James Cheng-Yi Lin5,6 Departments of Craniofacial Orthodontics, 1Craniofacial Research Center, Chang Gung Memorial Hospital and Graduate Institute of Craniofacial Medicine, Chang Gung University, Taipei, 105, 2Chang Gung Memorial Hospital, Taipei, Taiwan, 3Private Practice of Orthodontics, Dr. Mehta’s Dental Care and Cure 402, Pune, Maharashtra, India, 4Consultant Orthodontist, Inlaks and Budhrani Hospital and Poona Hospital and Research Centre, Pune, Maharashtra, India, 5Department of Orthodontics and Pediatric Dentistry, School of Dentistry, National Defense Medical University, Taipei, Taiwan, 6Private Practice of Orthodontics and Implantology, Dr. James Lin Clinic, Taipei, Taiwan. ABSTRACT Nonsurgical improvement of an occlusal cant, lip cant, and soft tissue chin deviation has been considered not possible merely through orthodontic treatment without surgical intervention. e purpose of this report was to illustrate a possible new field in orthodontics for a non-invasive improvement of the occlusal cant and soft tissue chin deviation through orthodontic approach by an innovative orthodontic archwire (Yin-Yang wire) and the others. *Corresponding author: Dr. Eric Jein-Wein Liou, Keywords: Orthodontic archwire, Occusal cant, Asymmetry. Department of Craniofacial Orthodontics, Chang Gung Memorial Hospital. 6F 199 Tung-Hwa North Road, INTRODUCTION