Recalcitrant Periprosthetic Joint Infection with Iliac Fossa Abscess After Total Hip Arthroplasty
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Expert-Based Assessment Model for Evaluating Habitat Suitability of Pond-Breeding Amphibians
sustainability Article An Expert-Based Assessment Model for Evaluating Habitat Suitability of Pond-Breeding Amphibians Shin-Ruoh Juang 1, Szu-Hung Chen 2 and Chen-Fa Wu 1,* 1 Department of Horticulture, National Chung Hsing University, Taichung City 402, Taiwan; [email protected] 2 Department of Ecosystem Science & Management, Texas A&M University, College Station, TX 77843, USA; [email protected] * Correspondence: [email protected]; Tel./Fax: +886-4-2285-9125 Academic Editor: Iain Gordon Received: 8 November 2016; Accepted: 10 February 2017; Published: 16 February 2017 Abstract: Farm ponds are important habitats for amphibians, birds, and other wildlife. In Taiwan, artificial ponds were originally created on farmlands for irrigation purposes and the needs of the domestic water supply. Although pond creation is a typical farming practice, it also provides habitats for pond-breeding amphibians. Thus, it is essential to understand the current status of habitats and their vulnerability regarding urgent conservation needs for target species. Günther’s frog (Hylarana guentheri), a pond-breeding amphibian, has a high sensitivity towards surrounding environmental changes, and can be used as an indicator species to assess habitat suitability. The purpose of this study is to establish a systematic framework to assess the habitat suitability of pond-breeding amphibians by using Günther’s frog as a pilot-study species. First, we collected frog survey data from Chiayi, Taiwan, from winter 2013 to spring 2015, and investigated the present status of the environmental conditions around the ponds. Next, expert questionnaires and the fuzzy Delphi method were applied to establish the hierarchical evaluation criteria regarding the habitat suitability assessment. -

The History and Politics of Taiwan's February 28
The History and Politics of Taiwan’s February 28 Incident, 1947- 2008 by Yen-Kuang Kuo BA, National Taiwan Univeristy, Taiwan, 1991 BA, University of Victoria, 2007 MA, University of Victoria, 2009 A Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY in the Department of History © Yen-Kuang Kuo, 2020 University of Victoria All rights reserved. This dissertation may not be reproduced in whole or in part, by photocopy or other means, without the permission of the author. ii Supervisory Committee The History and Politics of Taiwan’s February 28 Incident, 1947- 2008 by Yen-Kuang Kuo BA, National Taiwan Univeristy, Taiwan, 1991 BA, University of Victoria, 2007 MA, University of Victoria, 2009 Supervisory Committee Dr. Zhongping Chen, Supervisor Department of History Dr. Gregory Blue, Departmental Member Department of History Dr. John Price, Departmental Member Department of History Dr. Andrew Marton, Outside Member Department of Pacific and Asian Studies iii Abstract Taiwan’s February 28 Incident happened in 1947 as a set of popular protests against the postwar policies of the Nationalist Party, and it then sparked militant actions and political struggles of Taiwanese but ended with military suppression and political persecution by the Nanjing government. The Nationalist Party first defined the Incident as a rebellion by pro-Japanese forces and communist saboteurs. As the enemy of the Nationalist Party in China’s Civil War (1946-1949), the Chinese Communist Party initially interpreted the Incident as a Taiwanese fight for political autonomy in the party’s wartime propaganda, and then reinterpreted the event as an anti-Nationalist uprising under its own leadership. -

Atmospheric PM2.5 and Polychlorinated Dibenzo-P-Dioxins and Dibenzofurans in Taiwan
Aerosol and Air Quality Research, 18: 762–779, 2018 Copyright © Taiwan Association for Aerosol Research ISSN: 1680-8584 print / 2071-1409 online doi: 10.4209/aaqr.2018.02.0050 Atmospheric PM2.5 and Polychlorinated Dibenzo-p-dioxins and Dibenzofurans in Taiwan Yen-Yi Lee 1, Lin-Chi Wang2*, Jinning Zhu 3**, Jhong-Lin Wu4***, Kuan-Lin Lee1 1 Department of Environmental Engineering, National Cheng Kung University, Tainan 70101, Taiwan 2 Department of Civil Engineering and Geomatics, Cheng Shiu University, Kaohsiung 83347, Taiwan 3 School of Resources and Environmental Engineering, Hefei University of Technology, Hefei 246011, China 4 Sustainable Environment Research Laboratories, National Cheng Kung University, Tainan 70101, Taiwan ABSTRACT In this study, the atmospheric PM2.5, increases/decreases of the PM2.5, the PM2.5/PM10 ratio, total PCDD/Fs-TEQ concentrations, PM2.5-bound total PCDD/Fs-TEQ content, and PCDD/F gas-particle partition in Taiwan were investigated for the period 2013 to 2017. In Taiwan, the annual average PM2.5 concentrations were found to be 28.9, 24.1, 21.4, 20.2, –3 and 19.9 µg m in 2013, 2014, 2015, 2016, and 2017, respectively, which indicated that the annual variations in PM2.5 levels were decreasing during the study period. The average increases (+)/decreases (–) of PM2.5 concentrations were –16.7%, –11.1%, –5.75%, and –1.73% from 2013 to 2014, from 2014 to 2015, from 2015 to 2016, and from 2016 to 2017, respectively. Based to the relationship between PM10 values and total PCDD/F concentrations obtained from previous studies, we estimated that in 2017, the annual average total PCDD/Fs-TEQ concentrations ranged between 0.0148 –3 –3 (Lienchiang County) and 0.0573 pg WHO2005-TEQ m (Keelung City), and averaged 0.0296 pg WHO2005-TEQ m , while –1 the PM2.5-bound total PCDD/Fs-TEQ content ranged from 0.302 (Kaohsiung City) to 0.911 ng WHO2005-TEQ g –1 (Keelung City), at an average of 0.572 ng WHO2005-TEQ g . -

Relationships Between Floods and Social Fragmentation: a Case Study of Chiayi, Taiwan
Relationships between floods and social fragmentation: A case study of Chiayi, Taiwan • Yung-Jaan Lee • Chung-Hua Institution for Economic Research, Taiwan • Li-Pei Peng* • Ting-Jay Lee • National Taiwan University, Taiwan *Corresponding author Abstract Resumen Lee, Y.-J. Peng, L.-P., & Lee, T.-J. (March-April, 2017). Lee, Y.-J. Peng, L.-P., & Lee, T.-J. (marzo-abril, 2017). Las Relationships between floods and social fragmentation: A relaciones entre las inundaciones y la fragmentación social: un case study of Chiayi, Taiwan. Water Technology and Sciences estudio de caso de Chiayi, Taiwán. Tecnología y Ciencias del (in Spanish), 8(2), 5-18. Agua, 8(2), 5-18. The social vulnerability approach has been recognized El enfoque de la vulnerabilidad social ha sido reconocido como una de las as one of the most important tools for exploring contexts herramientas más importantes para explorar contextos y estrategias and coping strategies in relation to contemporary disasters. de afrontamiento en relación con los desastres contemporáneos. Sin However, social vulnerability is such a multi-faceted and embargo, la vulnerabilidad social es un constructo tan multifacético complex construct that scholars from different fields have not y complejo que estudiosos de diversas disciplinas no han llegado a un consenso sobre la mejor manera de medirlo y continúa el debate reached consensus on how best to measure it, and discussions 5 on this issue continue. Some scholars consider that this sobre dicha cuestión. Algunos estudiosos consideran que este enfoque puede manifestar el papel de la intervención humana. Sin approach can manifest the role of human agency. However, embargo, dada la falta de observaciones históricas, interpretar las given a lack of historical observations, interpreting the causes causas de los desastres a través de perspectivas basadas en eventos of disasters through event-based perspectives cannot easily no puede reflejar el mecanismo institucional detrás de tales eventos. -

Hemigobius Crassa (HERRE, 1945)
86 Journal of Marine Science and Technology, Vol. 21, Suppl., pp. 86-93 (2013) DOI: 10.6119/JMST-013-1220-4 THE MOLECULAR PHYLOGENY OF GENUS Hemigobius (TELEOSTEI: GOBIIDAE), WITH THE CONFIRMATION OF VALIDITY OF Hemigobius crassa (HERRE, 1945) Shih-Pin Huang1, I-Shiung Chen1, and Kwang-Tsao Shao2 Key words: Hemigobius, mangrove, gobies, Taiwan. in Thailand, Singapore and Indonesia [20, 21]. There are two possible Hemigobius species have been de- scribed in southern China. The Vaimosa crassa Herre, 1945 ABSTRACT collected from Hong Kong, and Mugilogobius obliquifascia- The genus Hemigobius Bleeker, 1874 is has been regarded tus Wu and Ni, 1985 collected from Hainan Island, Goung- as only two valid species in previous study including H. dong and Fujian Province, southern China. Previous studies hoevenii (Bleeker, 1851) and H. mingi (Herre, 1936). Tradi- consider they should be considered that two species are the tionally, the both Vaimosa crassa Herre, 1945 and Mugilogo- junior synonyms of Hemigobius hoevenii [20, 21]. On the bius obliquifasciatus Wu and Ni, 1985 found from Chinese other hand, the Hemigobius bleekeri Koumans, 1953 [19] and Taiwanese waters had ever been regarded as the junior collected from Java and Sphenentogobius vanderbilti Fowler, synonyms of H. hoevenii. However, our present study have 1940 [12] collected from Sumatra also be regarded as syno- been confirm that H. crassa collected from Hong Kong and nym of H. mingi [20, 21]. So far, merely two species including Taiwan is a valid species. The H. crassa can be well distin- H. hoevenii and H. mingi would be regarded as valid member guished from H. -

The Potential SARS-Cov-2 Entry Inhibitor
bioRxiv preprint doi: https://doi.org/10.1101/2020.03.26.009803; this version posted March 26, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. The potential SARS-CoV-2 entry inhibitor Jrhau Lung1, Yu-Shih Lin2, Yao-Hsu Yang3,4,5, Yu-Lun Chou6, Geng-He Chang 7, 8, Ming-Shao Tsai 7, Cheng-Ming Hsu 7 , Reming-Albert Yeh 7,Li-Hsin Shu 3, Yu-Ching Cheng 3, Hung Te Liu 3, Ching-Yuan Wu 3, 5* 1 Department of Research and Development, Chiayi Chang Gung Memorial Hospital, Chiayi Branch, Putzu, Taiwan 2 Department of Pharmacy, Chiayi Chang Gung Memorial Hospital, Chiayi Branch, Putzu, Taiwan. 3 Department of Traditional Chinese Medicine, Chang Gung Memorial Hospital, Chiayi Branch, Putzu, Taiwan. 4 Health Information and Epidemiology Laboratory of Chang Gung Memorial Hospital, Chiayi Branch, Putzu, Taiwan. 5 School of Chinese medicine, College of Medicine, Chang Gung University, Tao-Yuan, Taiwan. 6 Department of surgery, Kaohsiung Chang Gung Memorial Hospital 7 Department of Otolaryngology, Chang Gung Memorial Hospital, Chiayi, Taiwan 8 Center of Excellence for Chang Gung Research Datalink, Chang Gung Memorial Hospital, Chiayi, Taiwan *Correspondence to: Ching-Yuan Wu, M.D., Ph. D. 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.03.26.009803; this version posted March 26, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Promoted Human Oral Cancer Cells Metastatic Potential
Surfactin from Bacillus subtilis attenuates ambient air particulate matter- promoted human oral cancer cells metastatic potential Thi Thuy Tien Vo1,#, Chiang-Wen Lee2,3,4,5,#, Ching-Zong Wu1, Ju-Fang Liu6, Wei- Ning Lin7, Yuh-Lien Chen8, Lee-Fen Hsu9,10, Ming-Horng Tsai11,12, I-Ta Lee1,* 1School of Dentistry, College of Oral Medicine, Taipei Medical University, Taipei, Taiwan 2Department of Orthopaedic Surgery, Chang Gung Memorial Hospital, Puzi City, Chiayi County 61363, Taiwan 3Department of Nursing, Division of Basic Medical Sciences, and Chronic Diseases and Health Promotion Research Center, and Research Center for Chinese Herbal Medicine, Chang Gung University of Science and Technology, Puzi City, Chiayi County 61363, Taiwan 4Department of Safety Health and Environmental Engineering, Ming Chi University of Technology, New Taipei City 24301, Taiwan 5College of Medicine, Chang Gung University, Guishan Dist., Taoyuan City 33303, Taiwan 6School of Oral Hygiene, College of Oral Medicine, Taipei Medical University, Taipei, Taiwan 7Graduate Institute of Biomedical and Pharmaceutical Science, Fu Jen Catholic University, New Taipei City, Taiwan 8Department of Anatomy and Cell Biology, College of Medicine, National Taiwan University, Taipei, Taiwan 9Department of Respiratory Care, Chang Gung University of Science and Technology, Puzi City, Chiayi County 613, Taiwan 10Division of Neurosurgery, Department of Surgery, Chang Gung Memorial Hospital, Puzi City, Chiayi County 613, Taiwan 11Department of Pediatrics, Division of Pediatric Hematology/Oncology and Neonatology, Yunlin Chang Gung Memorial Hospital, Yunlin, Taiwan 12College of Medicine, Chang Gung University, Taoyuan, Taiwan #These authors contributed equally to this work Running Title: Inhibition of oral cancer cell invasion by surfactin *Corresponding Author: I-Ta Lee School of Dentistry, College of Oral Medicine, Taipei Medical University, Taipei, Taiwan 250 Wuxing St. -
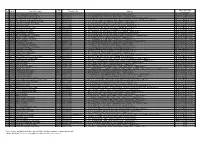
No. Area Post Office Name Zip Code Telephone No. Address Same Day
Zip Same Day Flight No. Area Post Office Name Telephone No. Address Code Cutoff Time* 1 Tainan Chiayi Wunhua Rd. Post Office 60044 (05)2259-408(05)2227-881 No. 134, Wunhua Rd., East District, Chiayi 600-44, Taiwan (R.O.C.) Next-Day-Flight Service** 2 Tainan Chiayi Jhongshan Rd. Post Office 60041 (05)2785-145 No. 107, Jhongshan Rd., East District, Chiayi 600-41, Taiwan (R.O.C.) Next-Day-Flight Service** 3 Tainan Shueishang Nanjing Post Office 60859 (05)2682-035 No. 1, Sanjhen Rd., Sanjhen Village, Shueishang, Chiayi County 608-59, Taiwan (R.O.C.) Next-Day-Flight Service** 4 Tainan Shueishang Jhongjhuang Post Office 60857 (05)2890-344 No. 61-61, Jhongjhuang, Jhongjhuang Village, Shueishang, Chiayi County 608-57, Taiwan (R.O.C.) Next-Day-Flight Service** 5 Tainan Chiayi Railway Station Front Post Office 60042 (05)2242-021 No. 647, Jhongjheng Rd., West District, Chiayi 600-42, Taiwan (R.O.C.) Next-Day-Flight Service** 6 Tainan Chiayi Mincyuan Rd. Post Office 60044 (05)2273-547 No. 467, Mincyuan Rd., West District, Chiayi 600-44, Taiwan (R.O.C.) Next-Day-Flight Service** 7 Tainan Taibao Post Office 61250 (05)3711-040 No. 439-2, Houtan Village, Taibao, Chiayi County 612-50, Taiwan (R.O.C.) Next-Day-Flight Service** 8 Tainan Chiayi Jhongsiao Post Office 60044 (05)2783-079 No. 2(08)1, Mincyuan Rd., East District, Chiayi 600-44, Taiwan (R.O.C.) Next-Day-Flight Service** 9 Tainan Chiayi Beishe Post Office 60092 (05)2320-200 No. 245, Beising St., West District, Chiayi 600-92, Taiwan (R.O.C.) Next-Day-Flight Service** 10 Tainan Shueishang Post Office 60848 (05)2682-140 No. -

Article Formatting Requirements
APPLYING GEO-DATA TO EVALUATE THE APPROPRIATENESS OF BUS NETWORK Chih-Hung Chang1, Jau-Ming Su2, Chao-Neng Chang3,, Chih-Kang Lin4,Mei-Hui Shen5, and Chin-Tung Tsai6 1,2,3,4Chih-Hung Chang, Chung Hua University, Department of Transportation Technology and Logistics Management [email protected], [email protected], [email protected], [email protected] 5Chung Hua University, Department of Transportation Technology and Logistics Management, [email protected] 6Operation and Management Division, Institute of Transportation, Ministry of Transportation and Communications, [email protected] Abstract In recent years, a great deal of resources have been invested in public transportation development in Taiwan. Although the Ratio of the Users of Public Transport has increased significantly, the pace of growth has already started to slow down. As a result, all levels of the governments are attempting to boost the ratio of the users of public transport by planning new transit service routes with potential. Due to the limitations of forecasts derived from conventional transportation demand data, some local and foreign scholars and research organizations have employed the service population indicator to plan transit service routes. In this study, we utilize a variety of geospatial data, such as village and street number diagrams from the Taiwan Geospatial One-Stop Portal, created by the Information Center, Ministry of the Interior; the Household Registration Statistics database; the Bus Dynamic Information System implemented by the Directorate General of Highways, Ministry of Transportation and Communications (MOTC); and other big data sources such as income and land use data. This will enable government transportation agencies to assess the benefits of new transit routes using transportation demand data and the service population indicator. -

Atmospheric Arsenic Deposition in Chiayi County in Southern Taiwan
Aerosol and Air Quality Research, 13: 932–942, 2013 Copyright © Taiwan Association for Aerosol Research ISSN: 1680-8584 print / 2071-1409 online doi: 10.4209/aaqr.2012.11.0315 Atmospheric Arsenic Deposition in Chiayi County in Southern Taiwan Long-Full Lin1, Shu Hsien Wu2, Sheng-Lun Lin3,4*, John Kennedy Mwangi2, Yi-Ming Lin5, Chia-Wei Lin2, Lin-Chi Wang4,6, Guo-Ping Chang-Chien4,7 1 Department of Environmental Engineering, Kun Shan University, Yung Kang, Tainan City 71003, Taiwan 2 Department of Environmental Engineering, National Cheng Kung University, Tainan City 70101, Taiwan 3 Center of General Education, Cheng Shiu University, Kaohsiung City 83347, Taiwan 4 Super Micro Mass Research and Technology Center, Cheng Shiu University, Kaohsiung City 83347, Taiwan 5 College of Environmental Science and Engineering, South China University of Technology, Guangzhou 510640, China 6 Department of Civil Engineering and Engineering Informatics, Cheng Shiu University, Kaohsiung City 83347, Taiwan 7 Department of Cosmetic and Fashion Styling, Cheng Shiu University, Kaohsiung City 83347, Taiwan ABSTRACT Although arsenic contamination of underground water in southern Taiwan is well known, few studies examine atmospheric arsenic deposition in this area, which might be the major source of such pollution to the soil, water, and even underground water. This research focused on the atmospheric arsenic concentration, dry and wet depositions, and the As distribution around Chiayi County, located in the south of Taiwan. Eight sampling sites are used, both upwind and downwind of an area with heavy industrial and human activities. All samples were collected by a PS-1 high volume sampler at each site, pretreated by a digestion process, and further analyzed with an ICP-MS. -

2016Taiwan Health and Welfare Report
ISSN-24092630 2016 Taiwan Health and Welfare Report Taiwan Health and 2016 Welfare Report Promote the health and well-being of all citizens Being the most trustworthy government agency Health Happiness Fairness Sustainability Ministry of Health and Welfare, R.O.C.(Taiwan) Ministry of Health and Welfare, ISSN 2409-2630 0 0 3 0 0 9 772409 263003 GPN : 2010302163 Price:NT$300 Advertisement Ministry of Health and Welfare, R.O.C. (Taiwan) Taiwan Health and Welfare Report 2016 Adhering to the Whole-Person Care Value, Achieving Holistic Health and Social Welfare Policies. Ministry of Health and Welfare, R.O.C.(Taiwan) Foreword The Ministry of Health and Welfare's responsibilities include health planning and promotion, prevention and control of disease, food safety, drug management, social insurance, and welfare, relief and protective services. Our mandate also includes biotechnology R&D, international health cooperation, and diverse other areas affecting public health and well-being far beyond Taiwan. To explain our agency's health and social administration initiatives, we publish this annual report outlining our major policies and their concrete results. Some important trends continue to develop. Taiwan has officially been an "aging society" since 1993, and the government has been building better living environments and a long-term care system for senior citizens. This system focuses on economic security, health care and maintenance, and living care. June 2015 saw the enactment of the Long-term Care Services Act, which will be implemented beginning in 2017. Our agency continues to formulate the Act's sub-statutes and ancillary measures, and to implement the plan's second phase. -

(Dry + Wet) Deposition of PCDD/Fs in Taiwan
Aerosol and Air Quality Research, 18: 2788–2800, 2018 Copyright © Taiwan Association for Aerosol Research ISSN: 1680-8584 print / 2071-1409 online doi: 10.4209/aaqr.2018.10.0363 Atmospheric (Dry + Wet) Deposition of PCDD/Fs in Taiwan Yen-Yi Lee 1, Wen-Che Hou1*, Jinning Zhu2*, Weiwei Wang2* 1 Department of Environmental Engineering, National Cheng Kung University, Tainan 70101, Taiwan 2 School of Resources and Environmental Engineering, Hefei University of Technology, Hefei 246011, China ABSTRACT Air pollution is becoming increasingly worse with economic development, and atmospheric deposition is an important mechanism for the removal of air pollutants. In 2017, the average dry deposition fluxes of total-PCDD/Fs-WHO2005-TEQ –2 –1 in various areas in Taiwan ranged between 57 (Lienchiang County in autumn) and 589 pg WHO2005-TEQ m month –2 –1 (Keelung City in winter), with an average of 221 pg WHO2005-TEQ m month . The average total deposition fluxes of total-PCDD/Fs-WHO2005-TEQ in various areas in Taiwan ranged between 65 (Lienchiang County in autumn) and 681 pg –2 –1 –2 –1 WHO2005-TEQ m month (Keelung City in winter), with an average of 263 pg WHO2005-TEQ m month . The fractions of dry deposition fluxes contributing to the total deposition fluxes ranged between 37.8% (Yilan County in winter) and 99.9% (Kaohsiung City in winter), with an average of 82.1%. This study provided valuable information for the control strategies of PCDD/Fs. Keywords: PM2.5; PCDD/Fs; Dry deposition; Total deposition. INTRODUCTION almost invariably as unwanted byproducts in all thermal systems and are distributed ubiquitously (U.S.