SYNDROME in QUESTION* 175 S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Dermoscopic Features of Trichoadenoma
Dermatology Practical & Conceptual Broadening the List of Basal Cell Carcinoma Mimickers: Dermoscopic Features of Trichoadenoma Riccardo Pampena1, Stefania Borsari1, Simonetta Piana2, Caterina Longo1,3 1 Centro Oncologico ad Alta Tecnologia Diagnostica, Azienda Unità Sanitaria Locale - IRCCS di Reggio Emilia, Italy 2 Pathology Unit, Azienda Unità Sanitaria Locale - IRCCS di Reggio Emilia, Italy 3 Department of Dermatology, University of Modena and Reggio Emilia, Modena, Italy Key words: trichoadenoma, basal cell carcinoma, adnexal tumors, dermoscopy Citation: Pampena R, Borsari S, Piana S, Longo C. Broadening the list of basal cell carcinoma mimickers: dermoscopic features of trichoadenoma. Dermatol Pract Concept. 2019;9(2):160-161. DOI: https://doi.org/10.5826/dpc.0902a17 Accepted: January 10, 2019; Published: April 30, 2019 Copyright: ©2019 Pampena et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Funding: This research was supported by Italian Ministry of Health (Project Code: NET-2011-02347213). Competing interests: The authors have no conflicts of interest to disclose. Authorship: All authors have contributed significantly to this publication. Corresponding author: Riccardo Pampena, MD, Centro Oncologico ad Alta Tecnologia Diagnostica, Azienda Unità Sanitaria Locale – IRCCS, Viale Risorgimento 80, 42123, Reggio Emilia, Italy. Email: [email protected] Introduction Case Presentation A wide spectrum of skin tumors may mimic basal cell carci- Dermoscopic evaluation was performed with a contact polar- noma (BCC) on both clinical and dermoscopic appearance. ized dermatoscope (DermLite Foto, 3Gen LLC, Dana Point, Among these, adnexal skin neoplasms and in particular CA, USA) and showed a general BCC-like appearance. -

Trichoblastoma Arising from the Nevus Sebaceus of Jadassohn
Open Access Case Report DOI: 10.7759/cureus.15325 Trichoblastoma Arising From the Nevus Sebaceus of Jadassohn Fatimazahra Chahboun 1 , Madiha Eljazouly 1 , Mounia Elomari 2 , Faycal Abbad 3 , Soumiya Chiheb 1 1. Dermatology Unit, Cheikh Khalifa International University Hospital, Mohammed VI University of Health Sciences, Casablanca, MAR 2. Plastic and Reconstructive Surgery, Cheikh Khalifa International University Hospital, Mohammed VI University of Health Sciences, Casablanca, MAR 3. Pathology, Cheikh Khalifa International University Hospital, Mohammed VI University of Health Sciences, Casablanca, MAR Corresponding author: Fatimazahra Chahboun, [email protected] Abstract Trichoblastoma is a rare benign skin adnexal tumour, belonging to the category of trichogenic tumours. The clinical and histological findings may often be confused with basal cell carcinoma, a malignant epidermal skin tumour. We report here a case of a 70-year-old man presented with a dome-shaped, dark-pigmented nodule within a yellowish hairless plaque on the scalp. The plaque had existed since childhood. However, the central pigmented nodule began appearing three months ago and enlarging gradually. The patient had no medical history. Furthermore the physical examination revealed a translucent, verrucous, and yellowish plaque, with central and pigmented nodule measuring 0.7 × 0.5 cm. Also basal cell carcinoma and trichoblastoma’s diagnosis were discussed. The patient was subsequently referred to the plastic surgery department, where he underwent a total excision. The histological examination was in favour of trichoblastoma arising from the nevus sebaceus. After 24 months of checking, no recurrence was observed. Trichoblastoma is a benign adnexal tumour. Its progression to malignant trichoblastoma (or trichoblastic carcinoma) is possible, but remains exceptional. -

The Best Diagnosis Is: H&E, Original Magnification 2
Dermatopathology Diagnosis The best diagnosis is: H&E, original magnification 2. a. adenoid cysticcopy carcinoma arising within a spiradenoma b. cylindroma and spiradenoma collision tumor c. microcysticnot change within a spiradenoma d. mucinous carcinoma arising within a spiradenoma Doe. trichoepithelioma and spiradenoma collision tumor CUTIS H&E, original magnification 100. PLEASE TURN TO PAGE 211 FOR DERMATOPATHOLOGY DIAGNOSIS DISCUSSION Amanda F. Marsch, MD; Jeffrey B. Shackelton, MD; Dirk M. Elston, MD Dr. Marsch is from the Department of Dermatology, University of Illinois at Chicago. Drs. Shackelton and Elston are from the Ackerman Academy of Dermatopathology, New York, New York. The authors report no conflict of interest. Correspondence: Amanda F. Marsch, MD, University of Illinois at Chicago, 808 S Wood St, Chicago, IL 60612 ([email protected]). 192 CUTIS® WWW.CUTIS.COM Copyright Cutis 2015. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. Dermatopathology Diagnosis Discussion Trichoepithelioma and Spiradenoma Collision Tumor he coexistence of more than one cutaneous adnexal neoplasm in a single biopsy specimen Tis unusual and is most frequently recognized in the context of a nevus sebaceous or Brooke-Spiegler syndrome, an autosomal-dominant inherited disease characterized by cutaneous adnexal neoplasms, most commonly cylindromas and trichoepitheliomas.1-3 Brooke-Spiegler syndrome is caused by germline muta- tions in the cylindromatosis gene, CYLD, located on band 16q12; it functions as a tumor suppressor gene and has regulatory roles in development, immunity, and inflammation.1 Weyers et al3 first recognized the tendency for adnexal collision tumors to present in patients with Brooke-Spiegler syndrome; they reported a patient with Brooke-Spiegler syndrome with spirad- Figure 1. -

Rippled-Pattern Sebaceoma: a Report of a Lesion on the Back with a Review of the Literature
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Fukui Repository Rippled-pattern sebaceoma: A report of a lesion on the back with a review of the literature Takahiro Kiyohara, M.D., Masanobu Kumakiri, M.D., Hiroaki Kuwahara, M.D., Atsuko Saitoh, M.D., and Shinichi Ansai, M.D. Department of Dermatology (T.K., M.K.), University of Fukui, Fukui; Division of Plastic Surgery (H.K.), Obihiro-Kousei General Hospital, Obihiro: Sapporo Institute for Dermatopathology (S.A.), Sapporo, Japan Address correspondence and reprint requests to: Takahiro Kiyohara, M.D. Department of Dermatology, University of Fukui 23-3 Shimoaizuki, Matsuoka-cho, Yoshida-gun, Fukui 910-1193, Japan Tel: +81 776 61 3111 Fax: +81 776 61 8112 e-mail: kiyo @ fmsrsa.fukui-med.ac.jp Abstract A 68-year-old Japanese man presented with a tumor that had been present for 5 to 6 years on the right back. Physical examination revealed a dome-shaped, 12x13-mm, dark red tumor. The tumor was excised with a 2 to 3-mm margin. The patient has remained free of disease during 77-months of follow-up. Microscopic examination revealed a bulb-like tumor in the dermis, contiguous with the overlying epidermis. It was composed of small, monomorphous, cigar-shaped basaloid cells in linear, parallel rows, resembling the palisading of nuclei of Verocay bodies, and presenting a rippled-pattern. There were scattered cells showing sebaceous differentiation with vacuolated cytoplasm and scalloped nuclei. There were tiny, duct-like spaces. The tumor revealed characteristics of rippled-pattern sebaceoma. -

Sebaceous Cell Carcinoma: a Persistent Challenge in Clinical And
erimenta xp l D E e r & m l a a t c o i l n o i Journal of Clinical & Experimental l g y C f R o e l ISSN: 2155-9554 s a e n Miyamoto et al., J Clin Exp Dermatol Res 2016, 7:3 a r r u c o h J Dermatology Research DOI: 10.4172/2155-9554.1000353 Review Article Open Access Sebaceous Cell Carcinoma: A Persistent Challenge in Clinical and Histopathological Diagnosis Denise Miyamoto1*, Beatrice Wang2, Cristina Miyamoto3,4, Valeria Aoki1, Li Anne Lim4, Paula Blanco4 and Miguel N Burnier4 1Department of Dermatology, University of São Paulo Medical School, Brazil 2Department of Dermatology, McGill University, Canada 3Department of Ophthalmology, Federal University of São Paulo, Brazil 4From the Henry C. Witelson Ocular Pathology Laboratory, McGill University, Canada *Corresponding author: Denise Miyamoto, University of São Paulo Medical School, São Paulo-State of São Paulo, Brazil, Tel: 514-934-76129; E-mail: [email protected] Received date: April 25, 2016; Accepted date: May 20, 2016; Published date: May 25, 2016 Copyright: © 2016 Miyamoto D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Sebaceous cell carcinoma continues to defy clinicians and pathologists in terms of early diagnosis. The tumor may be mistaken as benign lesions such as chalazion and blepharitis, and also as malignant neoplasms, mainly basal cell carcinoma and squamous cell carcinoma. Despite advances in immunohistochemical analysis and treatment options during the last decades, morbidity and metastasis rates remain high. -

Giant Vascular Eccrine Spiradenoma Ann Dermatol Vol
Giant Vascular Eccrine Spiradenoma Ann Dermatol Vol. 23, Suppl. 2, 2011 http://dx.doi.org/10.5021/ad.2011.23.S2.S197 CASE REPORT Giant Vascular Eccrine Spiradenoma Min Ho Kim, M.D., Eujin Cho, M.D., Jeong Deuk Lee, M.D., Ph.D., Sang Hyun Cho, M.D., Ph.D. Department of Dermatology, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea Giant vascular eccrine spiradenomas (GVESs) are a rare The diagnosis of GVES was made via histopathological variant of the eccrine spiradenoma that develops from the examination. sweat gland. It is different from the eccrine spiradenoma in its larger size and greater degree of vascularity. Bleeding CASE REPORT and/or ulceration are common clinical features of this tumor, and are the reason why it is often clinically confused with a A 49-year-old woman presented with a solitary deep mass vascular or malignant tumor. Here, a rare case of GVES of 10-year duration on the right upper arm. The lesion was without bleeding or ulceration is reported. (Ann Dermatol asymptomatic, firm, and 2.5×2.5 cm in size, with a bluish 23(S2) S197∼S200, 2011) color in the overlying intact skin (Fig. 1). On physical ex- amination, there were no abnormal findings other than the -Keywords- cutaneous lesion. An excisional biopsy was performed Eccrine spiradenoma, Giant vascular eccrine spiradenoma, and the specimen was grossly hemorrhagic. The histo- Sweat gland neoplasms pathological findings of the lesion showed a large, well-circumscribed, encapsulated, multilobulated tumor in the dermis. There was extensive hemorrhage and numer- INTRODUCTION ous dilated vascular spaces containing red blood cells or pale pinkish lymph fluid in the tumor (Fig. -
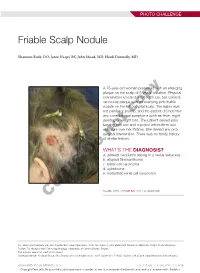
Friable Scalp Nodule
PHOTO CHALLENGE Friable Scalp Nodule Shannon Buck, DO; Jaree Naqvi, BS; John Moad, MD; Heidi Donnelly, MD A 75-year-old woman presented with an enlarging plaque on the scalp of 5 years’ duration. Physical examination revealed a 5.6×2.9-cm, tan-colored, verrucous plaque with an overlying pink friable nodule on the left occipital scalp. The lesion was not painful or pruritic,copy and the patient did not have any constitutional symptoms such as fever, night sweats, or weight loss. The patient denied prior tanning bed use and reported intermittent sun exposure over her lifetime. She denied any prior surgicalnot intervention. There was no family history of similar lesions. WHAT’S THE DIAGNOSIS? Doa. adnexal neoplasm arising in a nevus sebaceus b. atypical fibroxanthoma c. basal cell carcinoma d. cylindroma e. metastatic renal cell carcinoma CUTIS PLEASE TURN TO PAGE E20 FOR THE DIAGNOSIS Drs. Buck and Donnelly are from Dayton Skin Care Specialists, Ohio. Mr. Naqvi is from Boonshoft School of Medicine, Wright State University, Dayton. Dr. Moad is from Dermatopathology Laboratory of Central States, Dayton. The authors report no conflict of interest. Correspondence: Shannon Buck, DO, Dayton Skin Care Specialists, 3025 Governor’s Pl Blvd, Dayton, OH 45409 ([email protected]). WWW.MDEDGE.COM/DERMATOLOGY VOL. 105 NO. 1 I JANUARY 2020 E19 Copyright Cutis 2020. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. PHOTO CHALLENGE DISCUSSION THE DIAGNOSIS: Adnexal Neoplasm Arising in a Nevus Sebaceus iopsy of the lesion showed a proliferation of basa- secondary neoplasms, 88% of which were benign.2 The loid-appearing cells with focal ductal differentiation origins of these neoplasms can be epithelial, sebaceous, Band ulceration consistent with poroma (Figure 1). -

Trichoadenoma of the Upper Lip Gian Paolo Bombeccari, Gianpaolo Guzzi, Umberto Mariani, Andrea Gianatti, Diego Ruffoni, Franco Santoro, Francesco Spadari
CASE REPORTS SCIENTIFIC ARTICLES Stomatologija, Baltic Dental and Maxillofacial Journal, 17: 102-4, 2015 Trichoadenoma of the upper lip Gian Paolo Bombeccari, Gianpaolo Guzzi, Umberto Mariani, Andrea Gianatti, Diego Ruffoni, Franco Santoro, Francesco Spadari SUMMARY Background. Trichoadenoma of Nikolowski, who describe the first cases in 1958, is a rare and benign tumor of the hair follicle. It is well-differentiated and slowly-growing. The clinical appearance of Trichoadenoma (TA) can be similar to basal cell carcinoma or epidermal cyst. Results. We describe a 44-year-old male who was referred for nodular lesion on the upper lip and a TA was diagnosed. Oral examination showed exophytic yellow mass located between mucous membrane of the upper lip and vestibular gingiva, 1.2 per 0.8 cm. Anamnestic data was non-contributory. An excisional biopsy of the lesion was performed. Microscopically, the lesion consisted of multiple keratinous cysts lined with stratified squamous epithelium and intermingled with solid islands of basaloid cells lying within sclerotic stroma. The pathological diagnosis was TA. The surgical wound healed uneventfully. Conclusion. Because the lesion is unique, it is uncertain how aggressive or indolent the tumor might be. Therefore, the microscopical analysis is mandatory. At the best of our knowledge, this is the second case of trichoadenoma of the lip. Keywords: lip lesion, oral nodule, lip tumor, oral tumor, oral follicular hamartoma. INTRODUCTION Trichoadenoma (TA) is a rare benign tumor of than trichofolliculoma and is more differentiated the hair follicle, which was first described in 1958 by than trichoepithelioma (4). It is often apparent a dif- Nikolowsky as “organoid follicular hamartoma” (1). -

A Case of Trichogerminoma
Ann Dermatol Vol. 22, No. 4, 2010 DOI: 10.5021/ad.2010.22.4.431 CASE REPORT A Case of Trichogerminoma Minji Kim, M.D., Mira Choi, M.D., Jong Soo Hong, M.D., Jong Hee Lee, M.D.1, Soyun Cho, M.D.1 Department of Dermatology, Seoul National University College of Medicine, 1Seoul National University Boramae Hospital, Seoul, Korea Trichogerminoma is a rare neoplasm which was first We report here on a case of trichogerminoma that described in 1992 and there is still controversy over its developed on the nape of the neck of an elderly woman. inclusion into the spectrum of trichoblastoma. A 79-year-old We believe this is the first reported case of tricho- woman presented with a 5-year history of an asymptomatic germinoma in the Korean dermatological literature. nodule on the left posterior neck. Histologically, the lesion revealed a well-demarcated deep dermal nodule surrounded CASE REPORT by a pseudocapsule. The tumor was composed of lobules with basophilic cells and some of the lobules displayed a A 79-year-old woman presented with a 5-year history of distinctive pattern of densely packed ‘cell balls’ with an asymptomatic solitary nodule on the left posterior peripheral condensation. Immunohistochemically, the neck. It was a non-ulcerated, hemispheric, well-demar- tumor cells showed zonal CK5/6 immunoactivity in contrast cated, movable nodule with no subjective symptoms (Fig. with the negatively stained ‘cell balls’. These characteristics 1). The clinical diagnosis was epidermal cyst. were compatible with the diagnosis of trichogerminoma. We Excisional biopsy was performed and the lesion was report here on a rare case of a hair germ tumor called totally removed. -

The Immunohistochemical Differential Diagnosis of Microcystic Adnexal
J Cutan Pathol 2013: 40: 363–370 © 2013 John Wiley & Sons A/S. doi: 10.1111/cup.12085 Published by Blackwell Publishing Ltd John Wiley & Sons. Printed in Singapore Journal of Cutaneous Pathology The immunohistochemical differential diagnosis of microcystic adnexal carcinoma, desmoplastic trichoepithelioma and morpheaform basal cell carcinoma using BerEP4 and stem cell markers Background: Microcystic adnexal carcinoma (MAC), desmoplastic Klaus Sellheyer1,2, Paula trichoepithelioma (DTE) and morpheaform basal cell carcinoma (BCC) Nelson2, Heinz Kutzner3 and frequently impose a considerable differential diagnostic challenge and Rajiv M. Patel4 immunohistochemistry is often used as a differentiating diagnostic 1 adjunct. Department of Dermatology, Cleveland Clinic Foundation, Cleveland, OH, USA, Methods: Using standard immunohistochemical techniques, we 2Nelson Dermatopathology Associates, examined 21 examples of DTE, 17 examples of morpheaform BCC Atlanta, GA, USA, and 10 examples of MAC for the expression of BerEP4, a marker of 3Dermatopathologie Friedrichshafen, Friedrichshafen, Germany, and epithelial cells, and of three stem cell markers, pleckstrin homology-like 4Departments of Pathology and Dermatology, domain, family A, member 1 (PHLDA1) [T cell death-associated gene University of Michigan Medical Center, Ann 51 (TDAG51)], cytokeratin 15 (CK15) and cytokeratin (CK19). Arbor, MI, USA Results: All but one MAC was negative for BerEP4 and all morpheaform BCC expressed BerEP4. Sixteen out of 21 DTE were immunoreactive for BerEP4. All 21 DTE were PHLDA1 positive and all 17 morpheaform BCC were PHLDA1 negative. MAC showed a mixed staining pattern for PHLDA1. CK15 was expressed in 20/21 DTE, whereas the majority of cases of MAC and morpheaform BCC were CK15 negative. CK19 stained more MAC than DTE and morpheaform BCC. -

Current Diagnosis and Treatment Options for Cutaneous Adnexal Neoplasms with Apocrine and Eccrine Differentiation
International Journal of Molecular Sciences Review Current Diagnosis and Treatment Options for Cutaneous Adnexal Neoplasms with Apocrine and Eccrine Differentiation Iga Płachta 1,2,† , Marcin Kleibert 1,2,† , Anna M. Czarnecka 1,* , Mateusz Spałek 1 , Anna Szumera-Cie´ckiewicz 3,4 and Piotr Rutkowski 1 1 Department of Soft Tissue/Bone Sarcoma and Melanoma, Maria Sklodowska-Curie National Research Institute of Oncology, 02-781 Warsaw, Poland; [email protected] (I.P.); [email protected] (M.K.); [email protected] (M.S.); [email protected] (P.R.) 2 Faculty of Medicine, Medical University of Warsaw, 02-091 Warsaw, Poland 3 Department of Pathology and Laboratory Diagnostics, Maria Sklodowska-Curie National Research Institute of Oncology, 02-781 Warsaw, Poland; [email protected] 4 Department of Diagnostic Hematology, Institute of Hematology and Transfusion Medicine, 00-791 Warsaw, Poland * Correspondence: [email protected] or [email protected] † Equally contributed to the work. Abstract: Adnexal tumors of the skin are a rare group of benign and malignant neoplasms that exhibit morphological differentiation toward one or more of the adnexal epithelium types present in normal skin. Tumors deriving from apocrine or eccrine glands are highly heterogeneous and represent various histological entities. Macroscopic and dermatoscopic features of these tumors are unspecific; therefore, a specialized pathological examination is required to correctly diagnose patients. Limited Citation: Płachta, I.; Kleibert, M.; treatment guidelines of adnexal tumor cases are available; thus, therapy is still challenging. Patients Czarnecka, A.M.; Spałek, M.; should be referred to high-volume skin cancer centers to receive an appropriate multidisciplinary Szumera-Cie´ckiewicz,A.; Rutkowski, treatment, affecting their outcome. -

Trichoblastic Carcinoma
SM Journal of Clinical Pathology Case Report © Azevedo C. et al. 2020 Trichoblastic Carcinoma: A Case Report and Literature Review of an Extremely Rare and Diagnostically Challenging Cutaneous Malignancy of the Hair Follicle Chelsea Azevedo*, Joseph Varney, Karina Leyva, Matthew White, Nicole DiTommaso, Alexandria Kim, Emily Alimia, Cameron Volpe, and Mohamed Aziz Department of Pathology- American University of the Caribbean, School of Medicine, USA Abstract Trichoblastic carcinoma (TBC) is an extremely rare cutaneous malignancy of the hair follicle, first described in the literature in 1962 as a “primary neoplasm of the hair matrix” (1). Besides its rarity, TBC shares many clinical and histologic characteristics with basal cell carcinoma (BCC), making the diagnosis of TBC difficult to make. Many authors have described TBC as a malignant transformation of a benign trichoblastoma (TB), but a universal understanding of the pathophysiological origin of TBC has not been established (2, 3). We present a case of this uncommon tumor with the hope that this report will add to the small repertoire of available research, and aid clinicians in diagnosis and management of this rare tumor. Keywords: Trichoblastic, Carcinoma, Cutaneous, Basal cell carcinoma, Stroma, Hair follicle neoplasm. Mitosis Abbreviations TBC, it is important to distinguish TBC from other skin tumors with similar clinical presentations such as TB and BCC as TBC is : Trichoblastic Carcinoma. : Basal Cell Carcinoma. TBC BCC typically aggressive and has a high propensity to metastasize and TB: Trichoblastoma. TBCS: Trichoblastic Carcinosarcoma Introduction recurThis [11]. case represents an extremely rare entity with very few Trichoblastic carcinoma (TBC) is a rare malignant skin published cases and reports available.