Molecular Genetics of Von Willebrand Disease”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human ADAM12 Quantikine ELISA
Quantikine® ELISA Human ADAM12 Immunoassay Catalog Number DAD120 For the quantitative determination of A Disintegrin And Metalloproteinase domain- containing protein 12 (ADAM12) concentrations in cell culture supernates, serum, plasma, and urine. This package insert must be read in its entirety before using this product. For research use only. Not for use in diagnostic procedures. TABLE OF CONTENTS SECTION PAGE INTRODUCTION .....................................................................................................................................................................1 PRINCIPLE OF THE ASSAY ...................................................................................................................................................2 LIMITATIONS OF THE PROCEDURE .................................................................................................................................2 TECHNICAL HINTS .................................................................................................................................................................2 MATERIALS PROVIDED & STORAGE CONDITIONS ...................................................................................................3 OTHER SUPPLIES REQUIRED .............................................................................................................................................3 PRECAUTIONS .........................................................................................................................................................................4 -

Quantikine® ELISA
Quantikine® ELISA Human ADAMTS13 Immunoassay Catalog Number DADT130 For the quantitative determination of human A Disintegrin And Metalloproteinase with Thombospondin type 1 motif, 13 (ADAMTS13) concentrations in cell culture supernates, serum, and plasma. This package insert must be read in its entirety before using this product. For research use only. Not for use in diagnostic procedures. TABLE OF CONTENTS SECTION PAGE INTRODUCTION .....................................................................................................................................................................1 PRINCIPLE OF THE ASSAY ...................................................................................................................................................2 LIMITATIONS OF THE PROCEDURE .................................................................................................................................2 TECHNICAL HINTS .................................................................................................................................................................2 MATERIALS PROVIDED & STORAGE CONDITIONS ...................................................................................................3 OTHER SUPPLIES REQUIRED .............................................................................................................................................4 PRECAUTIONS .........................................................................................................................................................................4 -

ADAMTS13 and 15 Are Not Regulated by the Full Length and N‑Terminal Domain Forms of TIMP‑1, ‑2, ‑3 and ‑4
BIOMEDICAL REPORTS 4: 73-78, 2016 ADAMTS13 and 15 are not regulated by the full length and N‑terminal domain forms of TIMP‑1, ‑2, ‑3 and ‑4 CENQI GUO, ANASTASIA TSIGKOU and MENG HUEE LEE Department of Biological Sciences, Xian Jiaotong-Liverpool University, Suzhou, Jiangsu 215123, P.R. China Received June 29, 2015; Accepted July 15, 2015 DOI: 10.3892/br.2015.535 Abstract. A disintegrin and metalloproteinase with thom- proteolysis activities associated with arthritis, morphogenesis, bospondin motifs (ADAMTS) 13 and 15 are secreted zinc angiogenesis and even ovulation [as reviewed previously (1,2)]. proteinases involved in the turnover of von Willebrand factor Also known as the VWF-cleaving protease, ADAMTS13 and cancer suppression. In the present study, ADAMTS13 is noted for its ability in cleaving and reducing the size of the and 15 were subjected to inhibition studies with the full-length ultra-large (UL) form of the VWF. Reduction in ADAMTS13 and N-terminal domain forms of tissue inhibitor of metallo- activity from either hereditary or acquired deficiency causes proteinases (TIMPs)-1 to -4. TIMPs have no ability to inhibit accumulation of UL-VWF multimers, platelet aggregation and the ADAMTS proteinases in the full-length or N-terminal arterial thrombosis that leads to fatal thrombotic thrombocy- domain form. While ADAMTS13 is also not sensitive to the topenic purpura [as reviewed previously (1,3)]. By contrast, hydroxamate inhibitors, batimastat and ilomastat, ADAMTS15 ADAMTS15 is a potential tumor suppressor. Only a limited app can be effectively inhibited by batimastat (Ki 299 nM). In number of in-depth investigations have been carried out on the conclusion, the present results indicate that TIMPs are not the enzyme; however, expression and profiling studies have shown regulators of these two ADAMTS proteinases. -

ADAMTS Proteases in Vascular Biology
Review MATBIO-1141; No. of pages: 8; 4C: 3, 6 ADAMTS proteases in vascular biology Juan Carlos Rodríguez-Manzaneque 1, Rubén Fernández-Rodríguez 1, Francisco Javier Rodríguez-Baena 1 and M. Luisa Iruela-Arispe 2 1 - GENYO, Centre for Genomics and Oncological Research, Pfizer, Universidad de Granada, Junta de Andalucía, 18016 Granada, Spain 2 - Department of Molecular, Cell, and Developmental Biology, Molecular Biology Institute, University of California, Los Angeles, Los Angeles, CA 90095, USA Correspondence to Juan Carlos Rodríguez-Manzaneque and M. Luisa Iruela-Arispe: J.C Rodríguez-Manzaneque is to be contacted at: GENYO, 15 PTS Granada - Avda. de la Ilustración 114, Granada 18016, Spain; M.L. Iruela-Arispe, Department of Molecular, Cell and Developmental Biology, UCLA, 615 Charles Young Drive East, Los Angeles, CA 90095, USA. [email protected]; [email protected] http://dx.doi.org/10.1016/j.matbio.2015.02.004 Edited by W.C. Parks and S. Apte Abstract ADAMTS (a disintegrin and metalloprotease with thrombospondin motifs) proteases comprise the most recently discovered branch of the extracellular metalloenzymes. Research during the last 15 years, uncovered their association with a variety of physiological and pathological processes including blood coagulation, tissue repair, fertility, arthritis and cancer. Importantly, a frequent feature of ADAMTS enzymes relates to their effects on vascular-related phenomena, including angiogenesis. Their specific roles in vascular biology have been clarified by information on their expression profiles and substrate specificity. Through their catalytic activity, ADAMTS proteases modify rather than degrade extracellular proteins. They predominantly target proteoglycans and glycoproteins abundant in the basement membrane, therefore their broad contributions to the vasculature should not come as a surprise. -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Serine Proteases with Altered Sensitivity to Activity-Modulating
(19) & (11) EP 2 045 321 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.04.2009 Bulletin 2009/15 C12N 9/00 (2006.01) C12N 15/00 (2006.01) C12Q 1/37 (2006.01) (21) Application number: 09150549.5 (22) Date of filing: 26.05.2006 (84) Designated Contracting States: • Haupts, Ulrich AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 51519 Odenthal (DE) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • Coco, Wayne SK TR 50737 Köln (DE) •Tebbe, Jan (30) Priority: 27.05.2005 EP 05104543 50733 Köln (DE) • Votsmeier, Christian (62) Document number(s) of the earlier application(s) in 50259 Pulheim (DE) accordance with Art. 76 EPC: • Scheidig, Andreas 06763303.2 / 1 883 696 50823 Köln (DE) (71) Applicant: Direvo Biotech AG (74) Representative: von Kreisler Selting Werner 50829 Köln (DE) Patentanwälte P.O. Box 10 22 41 (72) Inventors: 50462 Köln (DE) • Koltermann, André 82057 Icking (DE) Remarks: • Kettling, Ulrich This application was filed on 14-01-2009 as a 81477 München (DE) divisional application to the application mentioned under INID code 62. (54) Serine proteases with altered sensitivity to activity-modulating substances (57) The present invention provides variants of ser- screening of the library in the presence of one or several ine proteases of the S1 class with altered sensitivity to activity-modulating substances, selection of variants with one or more activity-modulating substances. A method altered sensitivity to one or several activity-modulating for the generation of such proteases is disclosed, com- substances and isolation of those polynucleotide se- prising the provision of a protease library encoding poly- quences that encode for the selected variants. -

R&D Assay for Alzheimer's Disease
R&DR&D assayassay forfor Alzheimer’sAlzheimer’s diseasedisease Target screening⳼ Ⲽ㬔 antibody array, ᢜ⭉㬔 ⸽ἐⴐ Amyloid β-peptide Alzheimer’s disease⯸ ኸᷠ᧔ ᆹ⸽ inhibitor, antibody, ELISA kit Surwhrph#Surilohu#Dqwlerg|#Duud| 6OUSFBUFE 1."5SFBUFE )41 $3&# &3, &3, )41 $3&# &3, &3, 壤伡庰䋸TBNQMF ɅH 侴䋸嵄䍴䋸BOBMZUFT䋸䬱娴哜塵 1$ 1$ 1$ 1$ 5IFNPTUSFGFSFODFEBSSBZT 1$ 1$ QQ α 34, .4, 503 Q α 34, .4, 503 %SVHTDSFFOJOH0òUBSHFUFòFDUT0ATHWAY涭廐 6OUSFBUFE 堄币䋸4BNQMF侴䋸8FTUFSOPS&-*4"䍘䧽 1."5SFBUFE P 8FTUFSOCMPU廽喜儤应侴䋸0, Z 4VCTUSBUF -JHIU )31DPOKVHBUFE1BO "OUJQIPTQIPUZSPTJOF .FBO1JYFM%FOTJUZ Y $BQUVSF"OUJCPEZ 5BSHFU"OBMZUF "SSBZ.FNCSBOF $3&# &3, &3, )41 .4, Q α 34, 503 Human XL Cytokine Array kit (ARY022, 102 analytes) Adiponectin,Aggrecan,Angiogenin,Angiopoietin-1,Angiopoietin-2,BAFF,BDNF,Complement,Component C5/C5a,CD14,CD30,CD40L, Chitinase 3-like 1,Complement Factor D,C-Reactive Protein,Cripto-1,Cystatin C,Dkk-1,DPPIV,EGF,EMMPRIN,ENA-78,Endoglin, Fas L,FGF basic,FGF- 7,FGF-19,Flt-3 L,G-CSF,GDF-15,GM-CSF,GRO-α,Grow th Hormone,HGF,ICAM-1,IFN-γ,IGFBP-2,IGFBP-3, IL-1α,IL-1β, IL-1ra,IL-2,IL-3,IL-4,IL- 5,IL-6,IL-8, IL-10,IL-11,IL-12, IL-13,IL-15,IL-16,IL-17A,IL-18 BPa,IL-19,IL-22, IL-23,IL-24,IL-27, IL-31,IL-32α/β/γ,IL-33,IL-34,IP-10,I-TAC,Kallikrein 3,Leptin,LIF,Lipocalin-2,MCP-1,MCP-3,M-CSF,MIF,MIG,MIP-1α/MIP-1β,MIP-3α,MIP-3β,MMP-9, Myeloperoxidase,Osteopontin, p70, PDGF-AA, PDGF-AB/BB,Pentraxin-3, PF4, RAGE, RANTES,RBP4,Relaxin-2, Resistin,SDF-1α,Serpin E1, SHBG, ST2, TARC,TFF3,TfR,TGF- ,Thrombospondin-1,TNF-α, uPAR, VEGF, Vitamin D BP Human Protease (34 analytes) / -
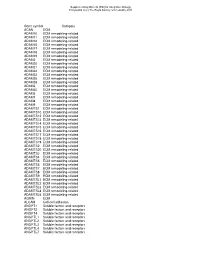
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

Pharmnotes February 2019
PharmNOTES Summary about new FDA products, generic medication, medical products, and WHAT IS IN THE PIPELINE. From: FEBRUARY 2019 Date: 3/7/2019 ©2019 PharmPiX. All rights reserved Table of Contents Page News 3 New FDA Approved Products 4-12 Jeuveau™ (prabotulinumtoxinA-xvfs) 4-5 Cablivi™ (caplacizumab-yhdp) 6-8 Egaten™ (triclabendazole) 9-10 Esperoct™ (turoctocog alfa pegol) 11-12 New FDA Approved Indications 13-14 New FDA Approved Dosage Forms, Formulations, Combinations, and Other Differences 15 New First-Time Generic Drug Approval 16 Pipeline 17-18 References 19 2 NEWS………………………… Drug Issue Date News/Event Increased risk of 02/21/2019 The FDA has concluded that there is an increased risk of death with Uloric (febuxostat) compared to another gout medicine, death with Uloric™ allopurinol. As a result, the Uloric™ prescribing information will include a Boxed Warning. The FDA is also limiting the (febuxostat) approved use of Uloric™ to certain patients who are not treated effectively or experience severe side effects with allopurinol. Recommendations for healthcare professionals: • Reserve Uloric™ for use only in patients who have failed or do not tolerate allopurinol. • Counsel patients about the cardiovascular risk with Uloric™ and advise them to seek medical attention immediately if they experience the following symptoms: chest pain, shortness of breath, rapid or irregular heartbeat, numbness or weakness on one side of the body, dizziness, trouble talking, sudden severe headache. For more details regarding this safety issue, please visit: https://www.fda.gov/Drugs/DrugSafety/ucm631182.htm Risk of blood clots in 02/25/2019 The FDA is alerting the public that a safety clinical trial found an increased risk of blood clots in the lungs and death when a 10 the lungs and death mg twice daily dose of tofacitinib (Xeljanz™, Xeljanz XR™) was used in patients with rheumatoid arthritis (RA). -

Development and Validation of a Protein-Based Risk Score for Cardiovascular Outcomes Among Patients with Stable Coronary Heart Disease
Supplementary Online Content Ganz P, Heidecker B, Hveem K, et al. Development and validation of a protein-based risk score for cardiovascular outcomes among patients with stable coronary heart disease. JAMA. doi: 10.1001/jama.2016.5951 eTable 1. List of 1130 Proteins Measured by Somalogic’s Modified Aptamer-Based Proteomic Assay eTable 2. Coefficients for Weibull Recalibration Model Applied to 9-Protein Model eFigure 1. Median Protein Levels in Derivation and Validation Cohort eTable 3. Coefficients for the Recalibration Model Applied to Refit Framingham eFigure 2. Calibration Plots for the Refit Framingham Model eTable 4. List of 200 Proteins Associated With the Risk of MI, Stroke, Heart Failure, and Death eFigure 3. Hazard Ratios of Lasso Selected Proteins for Primary End Point of MI, Stroke, Heart Failure, and Death eFigure 4. 9-Protein Prognostic Model Hazard Ratios Adjusted for Framingham Variables eFigure 5. 9-Protein Risk Scores by Event Type This supplementary material has been provided by the authors to give readers additional information about their work. Downloaded From: https://jamanetwork.com/ on 10/02/2021 Supplemental Material Table of Contents 1 Study Design and Data Processing ......................................................................................................... 3 2 Table of 1130 Proteins Measured .......................................................................................................... 4 3 Variable Selection and Statistical Modeling ........................................................................................ -

Von Willebrand Factor and ADAMTS13 Activity in Relation to Risk of Dementia
www.nature.com/scientificreports OPEN Von Willebrand factor and ADAMTS13 activity in relation to risk of dementia: a population- Received: 7 December 2017 Accepted: 21 March 2018 based study Published: xx xx xxxx Frank J. Wolters 1,2, Johan Boender3, Paul S. de Vries4, Michelle A. Sonneveld3, Peter J. Koudstaal2, Moniek P. de Maat3, Oscar H. Franco1, M. Kamran Ikram1,2, Frank W. Leebeek3 & M. Arfan Ikram 1 Low ADAMTS13 activity is associated with an increased risk of cardiovascular disease, which is generally attributed to its proteolytic efects on Von Willebrand factor (VWF). Cardiovascular health is an important determinant of cognitive decline, but the association of either VWF or ADAMTS13 with risk of dementia is unknown. Between 1997–2002, we measured VWF antigen and ADAMTS13 activity in 6055 participants of the population-based Rotterdam Study (mean age 69.3 years, 57.2% women). At baseline, 85 participants had dementia, and during 15 years of follow-up 821 developed dementia. Higher VWF was associated with prevalence and risk of dementia, unafected by concurrent ADAMTS13 activity, but estimates strongly attenuated over time and were no longer statistically signifcant at 4 years of follow-up (relative risks [95% CI] per standard deviation increase– cross-sectional: 1.37 [1.06– 1.77], and longitudinal: 1.05 [0.97–1.14]). In contrast, low ADAMTS13 was associated with increased risk of dementia throughout follow-up (hazard ratio per SD decrease– 1.16 [1.06–1.28]), which alike for ischaemic stroke, was modifed by the presence of diabetes (P-interaction = 0.003). In conclusion, higher VWF and low ADAMTS13 activity are associated with increased risk of dementia, but diferences in time-course and lack of synergistic efects may indicate in part independent underlying mechanisms. -

Expression of ADAMTS13 and PCNA in the Placentas of Gestational Diabetic Mothers
Int. J. Morphol., 39(1):38-44, 2021. Expression of ADAMTS13 and PCNA in the Placentas of Gestational Diabetic Mothers Expresión de ADAMTS13 y PCNA en las Placentas de Madres Diabéticas Gestacionales Süleyman Cemil Oglak1 & Mehmet Obut1 OGLAK, S. C. & OBUT, M. Expression of ADAMTS13 and PCNA in the placentas of gestational diabetic mothers. Int. J. Morphol., 39(1):38-44, 2021. SUMMARY: GDM is linked with overexpression of inflammatory cytokines and increased oxidative stress, leading to endothelial dysfunction and vascular disorder. Weaimed to examine the expression of ADAMTS13 and PCNA in the placentas of gestational diabe- tes mellitus (GDM) patients to investigate the effects of hypoxia, induced by GDM, on proliferation and extracellular matrix formation in the maternal and fetal placenta cells. A total of 60 placentas were collected from pregnant women admitted to the obstetrics clinic. Thirty of them were diagnosed with GDM, and 30 of them were diagnosed with non-GDM patients. Samples were fixed in 10 % formaldehyde, after routine follow-up, embedded in paraffin wax. Sections of 5 µm were cut stained with Mayer Hematoxylin-Eosin, examined under a light microscope. Sections for immunohistochemical analysis were cut and processed for antigen retrievalin citrate solution. Sections were incubated with ADAMTS13 and PCNA primary antibodies, counterstained with hematoxylin, and evaluate under a light microscope. In histopathological examination, the non-diabetic placentas showed that decidua cells in the maternal region were polygonal with oval nuclei and organized in groups. In the GDM group, there were pyknosis and apoptotic changes in decidua cell nuclei. Vacuolar areas were observed in large cavities in maternal connective tissue.