Insomnia Characteristics and Clinical Correlates in Operation Enduring Freedom/Operation Iraqi Freedom Veterans with Post-Trauma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sleep Problems
Sleep Problems About 70 million Americans have some kind of sleep problem, and for many it’s a long-term problem. Even though sleep problems are very common, they are very often undiagnosed and untreated. Here are descriptions of some of the most common sleep problems. Bruxism Bruxism is grinding, gnashing, or clenching your teeth during sleep or in situations that make you feel anxious or tense. It can be mild and happen only once in a while, or it may be violent and happen often. Bruxism most often happens in the early part of the night. You may not be aware that you have bruxism until your teeth or jaws are damaged. People who have bruxism are also more likely to snore and develop sleep apnea. Hypersomnia Hypersomnia is excessive daytime sleepiness or prolonged nighttime sleep. If you have hypersomnia, you feel very drowsy during the day and have an overwhelming urge to fall asleep, even after getting enough sleep at night. You often doze, nap, or fall asleep in situations where you need or want to be awake and alert. Other symptoms may include irritability, mild depression, trouble concentrating, and memory loss. Kleine-Levin Syndrome Kleine-Levin syndrome is a rare disorder that causes you to be extremely drowsy off and on. You may sleep up to 20 hours a day. Other symptoms include eating too much, being irritable, feeling disoriented, lacking energy, and being very sensitive to noise. The disorder usually starts in the late teens and is more common in men than in women. Symptoms may last for days to weeks, then go away, and then come back. -

Sleep Disturbances in Patients with Persistent Delusions: Prevalence, Clinical Associations, and Therapeutic Strategies
Review Sleep Disturbances in Patients with Persistent Delusions: Prevalence, Clinical Associations, and Therapeutic Strategies Alexandre González-Rodríguez 1 , Javier Labad 2 and Mary V. Seeman 3,* 1 Department of Mental Health, Parc Tauli University Hospital, Autonomous University of Barcelona (UAB), I3PT, Sabadell, 08280 Barcelona, Spain; [email protected] 2 Department of Psychiatry, Hospital of Mataró, Consorci Sanitari del Maresme, Institut d’Investigació i Innovació Parc Tauli (I3PT), CIBERSAM, Mataró, 08304 Barcelona, Spain; [email protected] 3 Department of Psychiatry, University of Toronto, #605 260 Heath St. West, Toronto, ON M5T 1R8, Canada * Correspondence: [email protected] Received: 1 September 2020; Accepted: 12 October 2020; Published: 16 October 2020 Abstract: Sleep disturbances accompany almost all mental illnesses, either because sound sleep and mental well-being share similar requisites, or because mental problems lead to sleep problems, or vice versa. The aim of this narrative review was to examine sleep in patients with delusions, particularly in those diagnosed with delusional disorder. We did this in sequence, first for psychiatric illness in general, then for psychotic illnesses where delusions are prevalent symptoms, and then for delusional disorder. The review also looked at the effect on sleep parameters of individual symptoms commonly seen in delusional disorder (paranoia, cognitive distortions, suicidal thoughts) and searched the evidence base for indications of antipsychotic drug effects on sleep. It subsequently evaluated the influence of sleep therapies on psychotic symptoms, particularly delusions. The review’s findings are clinically important. Delusional symptoms and sleep quality influence one another reciprocally. Effective treatment of sleep problems is of potential benefit to patients with persistent delusions, but may be difficult to implement in the absence of an established therapeutic relationship and an appropriate pharmacologic regimen. -

Dyssomnia Sleep Disorders.Pdf
Dyssomnia Sleep Disorders Dyssomnia Sleep Disorders By Yolanda Smith, BPharm Dyssomnia is a broad type of sleep disorders involving difficulty falling or remaining asleep, which can lead to excessive sleepiness during the day due to the reduced quantity, quality or timing of sleep. This is distinct from parasomnias, which involves abnormal behavior of the nervous system during sleep. Symptoms indicative a dyssomnia sleep disorder may include difficulty falling asleep, intermittent awakenings during the night or waking up earlier than usual. As a result of the reduced or disrupted sleep, most patients do not feel well rested and have less ability to perform during the day. In many cases, lifestyle habits have an impact on the disorder, including stress, physical pain or discomfort, napping during the day, bedtime or use of stimulants. Dyssomnia Sleep Disorders There are two main types of dyssomnia sleep disorders according to the origin or cause or the disorder: extrinsic and intrinsic. Both of these are covered in more detail below, in addition to general principles in the diagnosis and treatment of the disorders. Extrinsic dyssomnias are sleep disorders that originate from external causes and may include: Insomnia Sleep apnea Narcolepsy Restless legs syndrome Periodic Limb movement disorder Hypersomnia Toxin-induced sleep disorder Kleine-Levin syndrome Intrinsic dyssomnias are sleep disorders that originate from internal causes and may include: Altitude insomnia Substance use insomnia Sleep-onset association disorder Nocturnal paroxysmal dystonia Limit-setting sleep disorder Diagnosis The differential diagnosis between the types of dyssomnias usually begins with a consultation about the sleep history of the individual, including the onset, frequency and duration of sleep. -

What%Is%Idiopathic%Hypersomnia?%
What%is%Idiopathic%Hypersomnia?% Idiopathic*hypersomnia*is*sleeping*too*much*(hypersomnia)*without*an*obvious*cause.*It*is*different* from*narcolepsy,*because*idiopathic*hypersomnia*does*not*involve*suddenly*falling*asleep*or*losing* muscle*control*due*to*strong*emotions*(cataplexy).* Causes* The*usual*approach*is*to*consider*other*potential*causes*of*excessive*daytime*sleepiness.* Other*sleep*disorders*that*may*cause*daytime*sleepiness*include:* •Isolated*sleep*paralysis* •Narcolepsy* •Obstructive*sleep*apnea* •Restless*leg*syndrome* Other*causes*of*excessive*sleepiness*include:* •Atypical*depression* •Certain*medications* •Drug*and*alcohol*use* •Low*thyroid*function*(hypothyroidism)* •Previous*head*injury* Symptoms* Symptoms*often*develop*slowly*during*adolescence*or*young*adulthood.*They*include:* •Daytime*naps*that*do*not*relieve*drowsiness* •Difficulty*waking*from*a*long*sleep*KK*may*feel*confused*or*disoriented* •Increased*need*for*sleep*during*the*day*KK*even*while*at*work,*or*during*a*meal*or*conversation* •Increased*sleep*time*KK*up*to*14*K*18*hours*per*day* Other*symptoms*may*include:* •Anxiety* •Feeling*irritated* •Loss*of*appetite* •Low*energy* •Restlessness* •Slow*thinking*or*speech* •Trouble*remembering* Cataplexy*KK*suddenly*falling*asleep*or*losing*muscle*control*KK*which*is*part*of*narcolepsy,*is*NOT*a* symptom*of*idiopathic*hypersomnia.* Exams*and*Tests* The*health*care*provider*will*take*a*detailed*sleep*history.*Tests*may*include:* •MultipleKsleep*latency*test* •Sleep*study*(polysomnography,*to*identify*other*sleep*disorders)* -

Hypersomnia (Hypersomnolence) Symptoms and Diagnosis
Hypersomnia (Hypersomnolence) Symptoms and Diagnosis Hypersomnia (Hypersomnolence) Symptoms and Diagnosis By Yolanda Smith, BPharm Hypersomnia, also known as hypersomnolence, is a condition involving excessive daytime sleepiness or prolonged nighttime sleep on a recurring basis. Adolescents and young adults are most likely to be affected by the condition. It often causes affected individuals to take repeated naps throughout the day, which may disrupt other activities, such as work, study or social activities. These naps typically only provide temporary relief of symptoms and the desire to nap returns shortly afterwards. Common Symptoms It is common for people with hypersomnia to have difficulty waking up, particularly after a long sleep. They may feel disorientated and confused, which can continue for several hours in some patients. Excessive daytime sleepiness is the defining symptom of hypersomnia, despite getting a full night’s sleep. This may inhibit affected individuals from participating in daily routines or events. Additionally, it can be more difficult for them to maintain normal function in family, social and work environments. It can cause affected individuals to perform poorly and may lead to distress about other areas of their life. In particular, patients affected by hypersomnia are more likely to suffer from depression and anxiety than the general population. Although not all patients experience other signs and symptoms, hypersomnia may also be associated with: Anxiety Agitation Clouded thought processes and decision-making Depression Hallucinations Low energy levels Reduced appetite Reduced memory Restlessness Slow speech Diagnostic Techniques The primary diagnostic criterion for primary hypersomnia is excessive daytime sleepiness for at least one month in acute conditions or three months in persistent conditions. -
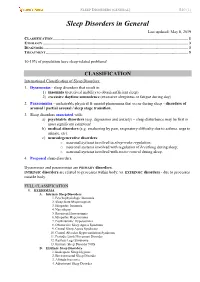
Sleep Disorders in General Last Updated: May 8, 2019 CLASSIFICATION
SLEEP DISORDERS (GENERAL) S40 (1) Sleep Disorders in General Last updated: May 8, 2019 CLASSIFICATION ...................................................................................................................................... 1 ETIOLOGY ................................................................................................................................................ 3 DIAGNOSIS................................................................................................................................................ 3 TREATMENT ............................................................................................................................................. 5 10-15% of population have sleep-related problems! CLASSIFICATION International Classification of Sleep Disorders: 1. Dyssomnias - sleep disorders that result in: 1) insomnia (perceived inability to obtain sufficient sleep) 2) excessive daytime somnolence (excessive sleepiness or fatigue during day) 2. Parasomnias - undesirable physical & mental phenomena that occur during sleep - disorders of arousal / partial arousal / sleep stage transition. 3. Sleep disorders associated with: a) psychiatric disorders (esp. depression and anxiety) – sleep disturbance may be first or most significant symptom! b) medical disorders (e.g. awakening by pain, respiratory difficulty due to asthma, urge to urinate, etc). c) neurodegenerative disorders: o neuronal systems involved in sleep-wake regulation; o neuronal systems involved with regulation of breathing during -

Pediatric Sleep: What Should We Know?
Pediatric Sleep: what should we know? C. MARIA RIVA MD PEDIATRIC SLEEP PROGRAM DIRECTOR MEDICAL UNIVERSITY OF SOUTH CAROLINA 2019 Objectives How sleep changes with age Sleep hygiene, sleep requirements Frequent sleep disorders: insomnia, hypersomnia conditions, sleep disordered breathing, parasomnias sleep studies in children, indications and difficulties Hypnogram Prevalence of pediatric sleep conditions In 2-18 y of age: Night terrors 40% (2-12 y of age) Nightmares 30% (<5y of age) Sleepwalking 30% (3-10 y of age) Insomnia (sleep onset and maintenance) 30% Bedtime resistance 15% (school age) Periodic limb movement disorder/RLS 5-10% Snoring 10% Obstructive Sleep Apnea (OSA) 1-2% Narcolepsy 0.05% Sleepwalking and other parasomia in children. UpToDate Sept 2017 Pediatric Sleep Disorders. Sufen Chiu MD. Medscape 2014. Clinical cases……….. Case study……Amber Amber is a 4 y old girl is in for a well child check. She has no medical problems. Since she started preschool 3 months ago, she has difficulty falling asleep and wakes up several times during the night. One parent reads her stories at bedtime (7 pm) for at least 30 min. She will come out of her room after the parent leaves and most of the time the father ends up staying with her until she falls asleep (8:30-9 pm). She wakes up at night and goes to the parents’ room. The mother gets up and stays with Amber until she falls back to sleep. Amber wakes up at 7:30 am, and takes a 2 hr nap during the day). Amber is not tired during the day. -

Post Traumatic Parasomnia-Case Series
Sleep Medicine and Disorders: International Journal Short Communication Open Access Post traumatic parasomnia-case series Abstract Volume 1 Issue 5 - 2017 Post traumatic stress disorders are associated with different sleep disorders such as Vyjayanthi S insomnia, frequent awakenings, nightmares and periodic limb movement disorders. However parasomnias that are known to occur due to lack of REM atonia and different Department of Psychiatry, MS Ramaiaha College, India quality of post traumatic nightmares from idiopathic nightmares and dream enactment behavior disorder that is seen independent of an actual post traumatic stress disorder Correspondence: Vyjayanthi S, Department of Psychiatry, have received little attention. Three case series of post traumatic somnambulism, MS Ramaiaha College, Gokula Extension, Bangalore, 560 054, Karnataka, India, Email [email protected] automatic texting and bruxism are reported to highlight this phenomenon. Received: November 16, 2017 | Published: December 21, parasomnia, post traumatic stress disorders, REM atonia, somnambulism, Keywords: 2017 bruxism Abbrevations: PTSD, post traumatic stress disorders; REM, narrative therapy. He was also given lorazepam during the therapy rapid eye movement and recovered completely in 6 months. Introduction Case vignette 2: automatic writing or texting in sleep Post traumatic stress disorders are associated with sleep A twenty three years old girl presented with complaints of disturbances that are considered as perhaps the core feature of automatic writing or texting to her mother at nights and no recall of the disorder.1 Nightmares, insomnia, hypersomnia, periodic limb the events during the day. Most of her text messages were about her movements have all been found to be associated with post traumatic mother being unjust in forgiving her biological brother who was 6 stress disorders2 Non nightmare related awakenings have also been years older to her and had sexually abused her. -

Idiopathic Hypersomnia Severity Scale
IDIOPATHIC HYPERSOMNIA SEVERITY SCALE On the basis of your symptoms during the past month: 1. What for you is the ideal duration of night-time sleep (at the weekend or on holiday, for example)? 3 11 hours or more 2 more than 9 hours and less than 11 hours 1 between 7 hours and 9 hours 0 less than 7 hours 2. When circumstances require that you get up at a particular time in the morning (for example for work or studies, or to take the children to school during the week), do you feel that you have not had enough sleep? 3 always 2 often 1 sometimes 0 never 3. Is it extremely difficult for you, or even impossible, to wake in the morning without several alarm calls or the help of someone close? 3 always 2 often 1 sometimes 0 never 4. After a night’s sleep, how long does it take you to feel you are functioning properly after you get up (in other words fully functional, both physically and intellectually)? 4 2 hours or more 3 more than 1 hour but less than 2 hours 2 between 30 minutes and 1 hour 1 less than 30 minutes 0 I feel I am functioning properly as soon as I wake up 5. In the minutes after waking up, do you ever do irrational things and/or say irrational things, and/or are you very clumsy (for example, tripping up, breaking things or dropping things)? 3 always 2 often 1 sometimes 0 never 6. During the day, when circumstances allow, do you ever take a nap? 4 very often (6-7 times a week) 3 often (4-5 times a week) 2 sometimes (2-3 times a week) 1 rarely (once a week) 0 never 7. -

Schizoaffective Disorder?
WHAT IS SCHIZOAFFECTIVE DISORDER? BASIC FACTS • SYMPTOMS • FAMILIES • TREATMENTS RT P SE A Mental Illness Research, Education and Clinical Center E C I D F I A C VA Desert Pacific Healthcare Network V M R E E Long Beach VA Healthcare System N T T N A E L C IL L LN A E IC S IN Education and Dissemination Unit 06/116A S R CL ESE N & ARCH, EDUCATIO 5901 E. 7th street | Long Beach, CA 90822 basic facts Schizoaffective disorder is a chronic and treatable psychiatric Causes illness. It is characterized by a combination of 1) psychotic symp- There is no simple answer to what causes schizoaffective dis- toms, such as those seen in schizophrenia and 2) mood symptoms, order because several factors play a part in the onset of the dis- such as those seen in depression or bipolar disorder. It is a psychi- order. These include a genetic or family history of schizoaffective atric disorder that can affect a person’s thinking, emotions, and be- disorder, schizophrenia, or bipolar disorder, biological factors, en- haviors and can impact all aspects of daily living, including work, vironmental stressors, and stressful life events. school, social relationships, and self-care. Research shows that the risk of schizoaffective disorder re- Schizoaffective disorder is considered a psychotic disorder sults from the influence of genes acting together with biological because of its prominent features of hallucinations and delusions. and environmental factors. A family history of schizoaffective dis- Therefore, people with this illness have periods when they have order does not necessarily mean children or other relatives will difficulty understanding the reality around them. -

Dysthymia and Apathy: Diagnosis and Treatment
Hindawi Publishing Corporation Depression Research and Treatment Volume 2011, Article ID 893905, 7 pages doi:10.1155/2011/893905 Review Article Dysthymia and Apathy: Diagnosis and Treatment Junko Ishizaki1, 2 and Masaru Mimura3 1 Department of Psychiatry, Nagata Hospital, 5173 Goji-cho, Miyakonojo-shi, Miyazaki 885-0084, Japan 2 Department of Neuropsychiatry, Showa University School of Medicine, 6-11-11 Kita-Karasuyama, Setagaya-ku, Tokyo 157-8577, Japan 3 Department of Neuropsychiatry, Keio University School of Medicine, 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan Correspondence should be addressed to Masaru Mimura, [email protected] Received 6 December 2010; Accepted 24 April 2011 Academic Editor: Mathias Berger Copyright © 2011 J. Ishizaki and M. Mimura. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Dysthymia is a depressive mood disorder characterized by chronic and persistent but mild depression. It is often difficult to be distinguished from major depression, specifically in its partially remitted state because “loss of interest” or “apathy” tends to prevail both in dysthymia, and remitted depression. Apathy may also occur in various psychiatric and neurological disorders, including schizophrenia, stroke, Parkinson’s disease, progressive supranuclear palsy, Huntington’s disease, and dementias such as Alzheimer’s disease, vascular dementia, and frontotemporal dementia. It is symptomatologically important that apathy is related to, but different from, major depression from the viewpoint of its causes and treatment. Antidepressants, especially noradrenergic agents, are useful for depression-related apathy. However, selective serotonin reuptake inhibitors (SSRIs) may be less effective for apathy in depressed elderly patients and have even been reported to worsen apathy. -

The Implications of Hypersomnia in the Context of Major Depression: Results from a Large, International, Observational Study
European Neuropsychopharmacology (2019) 29, 471–481 www.elsevier.com/locate/euroneuro The implications of hypersomnia in the context of major depression: Results from a large, international, observational study a a, b c a A. Murru , G. Guiso , M. Barbuti , G. Anmella , a, d ,e a ,f , g g h N. Verdolini , L. Samalin , J.M. Azorin , J. Jules Angst , i j k a, l C.L. Bowden , S. Mosolov , A.H. Young , D. Popovic , m c a, ∗ a M. Valdes , G. Perugi , E. Vieta , I. Pacchiarotti , For the BRIDGE-II-Mix Study Group a Barcelona Bipolar and Depressive Disorders Unit, Institute of Neuroscience, Hospital Clinic, University of Barcelona, IDIBAPS, CIBERSAM, Barcelona, Catalonia, Spain b Clinica Psichiatrica, Dipartimento di Igiene e Sanità, Università di Cagliari, Italy c Division of Psychiatry, Clinical Psychology and Rehabilitation, Department of Medicine, University of Perugia, Santa Maria della Misericordia Hospital, Edificio Ellisse, 8 Piano, Sant’Andrea delle Fratte, 06132, Perugia, Italy d FIDMAG Germanes Hospitalàries Research Foundation, Sant Boi de Llobregat, Barcelona, Catalonia, Spain e Division of Psychiatry, Clinical Psychology and Rehabilitation, Department of Medicine, Santa Maria della Misericordia Hospital, University of Perugia, Perugia, Italy f CHU Clermont-Ferrand, Department of Psychiatry, University of Auvergne, Clermont-Ferrand, France g Fondation FondaMental, Hôpital Albert Chenevier, Pôle de Psychiatrie, Créteil, France h Department of Psychiatry, Psychotherapy and Psychosomatics, Psychiatric Hospital, University of Zurich, Zurich,